Ultrasound Scans
Ultrasound: An Overview[edit | edit source]
Not to be confused with Therapeutic Ultrasound, medical ultrasonography uses high frequency broadband sound waves in the megahertz range that are reflected by tissue to varying degrees to produce (up to 3D) images (commonly associated with imaging the fetus in pregnant women). Ultrasonography is generally considered safe imaging with the World Health Organizations saying:
"Diagnostic ultrasound is recognized as a safe, effective, and highly flexible imaging modality capable of providing clinically relevant information about most parts of the body in a rapid and cost-effective fashion"[1].
There are several divisions in which ultrasound can be used as a diagnostic tool. These divisions include cardiovascular ultrasound, abdominal ultrasound, and musculoskeletal ultrasound.
- Cardiovascular Ultrasound - The use of diagnostic ultrasound to view the musculature of the heart as well as arteries and veins throughout the human body.[2]
- Abdominal Ultrasound - The use of diagnostic ultrasound to view the abdominal viscera and the contents within them. This also includes the viewing of fetus in utero.[2]
Musculoskeletal Ultrasound[edit | edit source]
Musculoskeletal Ultrasound can be defined as the use of diagnostic ultrasound with the intent to view structures of the musculoskeletal system. These structures include muscles, tendons, ligaments, nerves, and joints. The use of ultrasound to view these structures can be helpful in the diagnosis of musculoskeletal pathologies including, but not limited to, tendinopathies, strains, sprains, tears, and arthritic changes within joint spaces.[2]
Equipment Involved In MSK Ultrasound[edit | edit source]
- Ultrasound Tower
- Tower styles will vary depending upon different manufacturers.
- Transducer
- Phased - use of low frequency to visualize deeper structures such as the heart. The smaller head allows for navigation around the ribs to view contents within the ribcage.[2]
- Linear - use of high frequency and high resolution up to 5cm, generally used for MSK ultrasound.[2]
- Curved - use of lower frequency used to visualize deeper structures such as abdominal organs, viscera, obstetrics, and gynecological needs.[2]
- Ultrasound Medium
- A specific gel manufactured for ultrasound transmission will be needed to use in adjunct with the transducer heads.
This short video gives a animated insight into how US scans work
How to Perform an MSK Ultrasound Scan[edit | edit source]
The overall process to performing an ultrasound is relatively simple. This is one advantage to using ultrasound for diagnostic imaging. Once you have gathered all necessary equipment, you will want to position the patient in a manner that allows access to the desired area for scanning while maintaining patient comfort. You will then apply a gel medium to the area of choice and place the transducer onto the gel. Steps on how to position and manipulate the transducer will be provided in the video(s) below. Once you have completed the ultrasound you will shut off the machine and clean off the gel medium from the transducer and treatment area. Please watch the video provided, to learn more about performing an ultrasound scan.
Transducer Movements[edit | edit source]
Advantages[edit | edit source]
While it may provide less anatomical detail than techniques such as CT or MRI, it has several advantages which make it ideal in numerous situations
- Can view moving structures such as muscles and tendons to assess integrity and possible impingement throughout differing ranges of motion[6]
- Emits no ionizing radiation[7]
- Can be used for elastography to assess tissue softening by measuring displacement before and after a compression force is applied[6]
- It is very safe to use and does not appear to cause any adverse effects, although information on this is not well documented
- Procedures are relatively inexpensive and quick to perform
- Ultrasound scanners can be taken to critically ill patients in intensive care units, avoiding the danger caused while moving the patient to the radiology department
- The real time moving image obtained can be used to guide drainage and biopsy procedures
- Doppler capabilities on modern scanners allow the blood flow in arteries and veins to be assessed[6]
Disadvantages/Limitations[edit | edit source]
The disadvantages and limitations of diagnostic ultrasound include:
- Equipment costs can range from $1,000 to $70,000 per device[8]
- Ultrasound techniques require extensive anatomical knowledge and training[7][9]
- Limited penetration due to more dense tissues blocking ultrasound waves[9]
- A lower frequency is required for optimal imaging of deep tissues leading to lower resolution images[7]
- Incomplete assessment of joints and bone due to reflection of all sound waves back into the transducer head upon contact with bone[9]
- Anisotropy (part of the tissue that is there but not visualized) can occur when sound waves are not perpendicular to the targeted structure[7]
Who Can Use MSK Ultrasound?[edit | edit source]
MSK ultrasound can be utilized by radiologists and non-radiologists. Healthcare providers from different disciplines have the option of utilizing ultrasound, in terms of diagnostic imaging. Physicians that wish to use it have to take the necessary steps to acquire the certifications and education. Possessing an in-depth understanding of neurological and musculoskeletal anatomy is optimal. There is no current educational infrastructure available within healthcare programs. As the use of MSK ultrasound is becoming more popular, more online courses and continuing education opportunities are becoming available[10].
The Alliance for Physician Certification and Advancement(APCA), American Institute for Ultrasound in Medicine(AIUM), and the American Physical Therapy Association (APTA) are three major corporations that are working together to endorse the use of diagnostic ultrasound in the physical therapy practice. The APCA offers a certification in the use of diagnostic ultrasound that can be acquired by physical therapists. This certification is known as Registered in Musculoskeletal Sonography Certification or RMSK. A few of the prerequisites to the RMSK certification include:[11]
- A current and valid license in PT.
- Attestation letter indicating performance of 150 ultrasound studies within the last 3 years.
- A patient log documenting all 150 patients that have been subjects of an ultrasound study.
Below are some links to further resources from the APCA, AIUM, and APTA:
APCA.org - RMSK for the Physical Therapist
APCA.org - Musculoskeletal Ultrasound Certification
APTA - Opportunities for PTs to Advance Proficiency in MSK Ultrasound
Clinical Relevance for the Physical Therapist[edit | edit source]
MSK ultrasound can be a beneficial resource for diagnostic imaging for practitioners. While it is a good resource to use in adjunct with MRI's, it can be beneficial for physical therapists to utilize to avoid having to refer out for imaging. MSK ultrasound allows therapists to observe tissue and joint structures throughout the rehabilitation process. Doing so, can allow you to monitor structures and/or architecture of tissue as they may change throughout rehabilitation. Being able to view structures in real time while you are treating the patient can allow you to determine whether subjective and objective findings correlate with your diagnostic hypothesis.[12]
Example Case Study: 52 y/o female presents with unilateral shoulder pain involving abduction, flexion, and external rotation, coupled with complaints of night pain. Symptoms began following a fall that consisted of her arm being outstretched (FOOSH). Suspected diagnosis: Rotator cuff pathology. Ultrasound scans can be used to view tissues within the shoulder, allowing you to confirm your diagnosis and monitor structural change throughout treatment.
Patient Perceptions: Often, patients may receive a specific diagnosis that they do not completely understand. Through utilization of diagnostic ultrasound, practitioners of physical therapy can give patients a better understanding of their diagnosis and an increase in reassurance of the accuracy of that diagnosis, which can potentially lead to better patient outcomes.[13]
Application of Ultrasound in Sports Injury[edit | edit source]
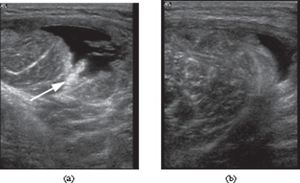
The ability to make correct ultrasonographic diagnosis in sports injuries is improving as advancing technology allows for high-resolution images in contemporary medical ultrasound. Ultrasonography demonstrates tissue structure with two-dimensional grayscale images. Blood flow in the tissue can be rapidly depicted with colour and power Doppler technique. Ultrasonography is the preferred imaging modality to study soft tissue lesions dynamically. With high-resolution images possible with ultrasonography, injuries of the muscle, tendon, ligament, bursa, bony structure, cartilage, and subcutaneous tissue can be accurately diagnosed (if the examiner is well trained). Recently, compact ultrasound machine machines are becoming increasingly available, leading to prompt ultrasonographic diagnosis of sports injuries on the field[14].
References[edit | edit source]
- ↑ WHO study group. TRAINING IN DIAGNOSTIC ULTRASOUND: ESSENTIALS, PRINCIPLES AND STANDARDS.Spain 1998 Available from: https://apps.who.int/iris/bitstream/handle/10665/42093/WHO_TRS_875.pdf;jsessionid=992840A3C30619985E80DCD5243B24CA?sequence=1 (last accessed 22.9.2019).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Varela T. Week twelve: Diagnostic imaging [unpublished lecture notes]. DPT551: Principles of clinical medicine, Arkansas Colleges of Health Education; lecture given 2022 Nov 02.
- ↑ NIBIB gov How Ultrasound Works Available from: https://www.youtube.com/watch?v=I1Bdp2tMFsY (last accessed 22.9.2019)
- ↑ Students of Musculoskeletal PT. Performance of MSK US. Available from: https://www.youtube.com/watch?v=nmwymSMe20U [last accessed 4/4/2023]
- ↑ Students of Musculoskeletal PT. Transducer Movements. Available from: https://www.youtube.com/watch?v=kXyOqMi30Uk [last accessed 4/4/2023]
- ↑ 6.0 6.1 6.2 Ian Beggs. Musculoskeletal Ultrasound [Internet]. Vol. 1st edition. Philadelphia: LWW; 2014 [cited 2023 Apr 4]. Available from: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,shib&db=e000xna&AN=1484402&site=eds-live
- ↑ 7.0 7.1 7.2 7.3 Roberts S. Ultrasound-pros and cons [Internet]. [Place unknown]: ESPA; c2023. Available from: https://www.euroespa.com/science-education/specialized-sections/espa-pain-committee/us-regional-anaesthesia/ultrasound-pros-and-cons/ (last accessed 4.4.2023)
- ↑ Ultrasound Machines and Medical Imaging Equipment [Internet]. [place unknown]: Ultrasound Solutions Corp.; c2022. How much does an ultrasound machine cost – 11 factors to consider; 2022, May 20 [cited 2023 April 4]; Available from: https://www.uscultrasound.com/ultrasound-machine-cost/
- ↑ 9.0 9.1 9.2 Baloch N, Hasan OH, Jessar MM, Hattori S, Yamada S. “Sports Ultrasound”, advantages, indications and limitations in upper and lower limbs musculoskeletal disorders. Review article. International Journal of Surgery. 2018 Jun 1;54:333-40. BibTeXEndNoteRefManRefWorks
- ↑ Smith J, Finnoff JT. Diagnostic and interventional musculoskeletal ultrasound: part 1. Fundamentals. PM&R. 2009 Jan 1;1(1):64-75.
- ↑ Alliance for Physician Certification and Advancement. RMSK for Physical Therapists [Internet]. Rockville, MD: Inteleos Inc.; 2023 [cited 2023 April 6]. Available from: https://www.apca.org/msk-physical-therapists/
- ↑ Faltus J, Boggess B, Bruzga R. The use of diagnostic musculoskeletal ultrasound to document soft tissue treatment mobilization of a quadriceps femoris muscle tear: a case report. International journal of sports physical therapy. 2012 Jun;7(3):342.
- ↑ Wheeler P. What do patients think about diagnostic ultrasound? A pilot study to investigate patient-perceived benefits with the use of musculoskeletal diagnostic ultrasound in an outpatient clinic setting. International Musculoskeletal Medicine. 2010 Jun 1;32(2):68-71.
- ↑ Chiang YP, Wang TG, Hsieh SF. Application of ultrasound in sports injury. Journal of Medical Ultrasound. 2013 Mar 1;21(1):1-8. Available from: https://www.sciencedirect.com/science/article/pii/S092964411300009X (last accessed 22.9.2019)