Post Operative Physiotherapy for Pronator Teres Tendon Transfer
Original Editor - Tanvi Korba Top Contributors - Tanvi Korba and Kim Jackson
Introduction[edit | edit source]
Peripheral nerve injuries can occur in a variety of ways. Peripheral nerve injuries (PNI) most frequently result from three mechanisms: stretch, laceration, and compressions. The Seddon Classification and the Sunderland Classification are the two most widely used classifications for PNI. The type of injury determines whether or not the peripheral nervous system can regenerate nerves. The degree of functional impairment resulting from nerve lesions is linked to the lesion's severity. A nerve lesion can cause Wallerian degeneration. It is an active process of anterograde axon degeneration at the distal end. [1]
Patients with peripheral nerve injuries can benefit from the use of nerve injury rehabilitation techniques in their care. Damage to peripheral nerves can impair an individual's ability to perform manual, social, and functional tasks. It could lead to impairments. Thus, patients with peripheral nerve injuries have been treated with physiotherapy techniques such as kinetic therapy, electrical stimulation, magnetotherapy, and bio-laser stimulation.[2]
Proximal radial nerve injuries are seen mainly in patients with humeral shaft fractures[3]. Tendon and nerve transfers are utilised if the Functional recovery is not observed after primary nerve repair. This surgical option is available for reconstruction of the wrist, thumb, and finger extension. The motor branch of the flexor digitorum superficialis (FDS) is used for the motor branch of the extensor carpi radialis brevis (ECRB). It is mainly used for a synergistic effect. The FDS function gets affected if the only branch of the FDS nerve is cut off. In such case scenarios, pronator teres (PT) nerve transfer to the extensor carpi radialis longus (ECRL) nerve is preferred to achieve and restore wrist extension[4]. For wrist extension reconstruction, the ECRB muscle is preferred over the ECRL due to ECRB muscle’s central location. That provides better-balanced radio-ulnar deviation during wrist extension[5][6][7]. Outcomes of tendon transfer are considered favourable when patients achieve good wrist extension, finger extension, thumb extension, and hand grip[8].
Procedure[edit | edit source]
This video describes the indications and techniques of tendon transfers for radial nerve palsy.
Indications of Surgery[edit | edit source]
Indications[9] for tendon transfers in high radial nerve injuries are:
- Unlikely nerve recovery- No change or plateaued recovery observed over the past few months with the help of assessment techniques
- No recovery following nerve repair surgery
- Failure to achieve recovery after a period of non-surgical management
Evaluation[edit | edit source]
A team approach can effectively address pre-operative issues and enhance post-operative success. The ideal team would consist of a hand surgeon, physician assistant or nurse practitioner, hand therapist (Occupational or Physical therapist), electro-diagnostician, social worker, the client, and family.
- Neural recovery status- By using electrodiagnostic tests such as electromyography or nerve conduction studies
- Musculoskeletal assessment- Active and Passive range of motion available in the involved joint, active range during functional tasks
- Strength of the muscles- Manual muscle testing or hand-held dynamometry, Grip, and pinch dynamometers
- Assessment of function/ dexterity to document pre-operative performance
- Testing for sensibility- The Weinstein Enhanced Sensibility Test or Semmes-Weinstein monofilaments are used to measure touch pressure threshold and discrimination assessment using static or moving two-point discrimination.
- Patient-related factors such as compliance, motivation, finances, previous and current interests/ abilities including other psychosocial issues such as emotional distress due to neuropathic pain.
- Outcome measures- DASH score, Quick DASH score [10][11]
Post-Operative Treatment[edit | edit source]
Education[edit | edit source]
This includes information on post-operative guidelines, activity limitations, exercise programme, splints/ orthosis, and timeline for therapy.
Protection Phase Goals[edit | edit source]
This entails guarding the area with reduced sensitivity and securing the surgical site. Following tendon transfer surgery, the affected limb is immobilised in a bulky dressing with a plaster. Afterwards, the cast or a customised thermoplastic orthosis replaces it and lasts for three to five weeks. The extremity positioned in the orthosis depends on the surgical procedure and the clinical picture. The splint is assessed at regular intervals to ensure comfort and protection of the surgical site. To prevent the operating limb from swelling, it is advised to keep it elevated. Non-involved proximal joint movement helps to prevent secondary joint stiffness and decrease distal extremity oedema. [10][11]
Phase of Transfer Activation[edit | edit source]
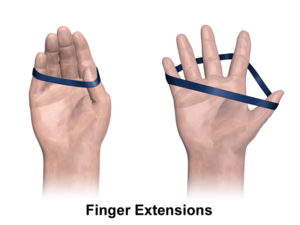
It also involves the transferred muscle's activation. Sessions are kept brief and within the limits of the patient's tolerance. In order to avoid fatigue and damage to the transferred muscle, the patients are advised to move slowly. The patient is instructed to wear an orthosis during the day at home and take it off for exercise. Soft tissue mobility techniques and oedema control are reinforced. Isolated movements are performed in a plane that is gravity-free during the first phase. The therapist uses the place-and-hold method if they are having trouble doing so. In order to do this, the therapist must gently place the limb in the new position while asking the patient to hold it. The transferred muscle's previous and current roles must be performed simultaneously in order for them to learn the new role. In order to activate the pronator teres muscle, which is used as a wrist extensor during surgery, the patient must simultaneously pronate their forearm and extend their wrist. Any jerky or forceful movements ought to be avoided. The forearm should be in a roughly 20-degree pronation; if the patient is experiencing difficulty activating the transfer, they are asked to perform pronation while receiving counter-pressure from the therapist. With the assistance of this resisted pronation, the transferred muscle will be stimulated to produce a wrist extension. Techniques for activating muscles include therapeutic whirlpool, mirror visual feedback, NMES, and biofeedback. [10][11] The flexor carpi ulnaris may be transferred to the extensor digitorum communis (EDC) to improve digit extension. If this surgery is carried out, the patient will be instructed to extend the MCP joints while flexing the wrist to neutral from an extended position during this phase. Patient is educated not to flex the wrist forcefully during this exercise. [10]
Rehabilitation Phase[edit | edit source]
The orthosis may be stopped during this phase or worn at night following the surgeon's instructions. If, by the eighth week following surgery, the patient can activate the transferred muscle without assistance, then he is ready for functional task practice and strengthening. Upper extremity strengthening, resisted pinch, and grip exercises are added to the programme as per patient tolerance. It is also encouraged for the client to engage in everyday activities, recreational pursuits, and work-related activities. These training sessions are set up in a block, random, or serial format. [10][11]
References[edit | edit source]
- ↑ Conforti L, Gilley J, Coleman MP. Wallerian degeneration: an emerging axon death pathway linking injury and disease. Nature Reviews Neuroscience. 2014 Jun;15(6):394-409.
- ↑ Suszyński K, Marcol W, Górka D. Physiotherapeutic techniques used in the management of patients with peripheral nerve injuries. Neural regeneration research. 2015 Nov;10(11):1770.
- ↑ Ekholm R, Ponzer S, Törnkvist H, Adami J, Tidermark J. The Holstein-Lewis humeral shaft fracture: aspects of radial nerve injury, primary treatment, and outcome. Journal of orthopaedic trauma. 2008 Nov 1;22(10):693-7.
- ↑ García-López A, Navarro R, Martinez F, Rojas A. Nerve transfers from branches to the flexor carpi radialis and pronator teres to reconstruct the radial nerve. The Journal of Hand Surgery. 2014 Jan 1;39(1):50-6.
- ↑ Sammer DM, Chung KC. Tendon transfers part I: principles of transfer and transfers for radial nerve palsy. Plastic and reconstructive surgery. 2009 May;123(5):169e.
- ↑ Moussavi AA, Saied A, Karbalaeikhani A. Outcome of tendon transfer for radial nerve paralysis: Comparison of three methods. Indian journal of orthopaedics. 2011 Dec;45:558-62.
- ↑ Bertelli JA, Tacca CP, Duarte EC, Ghizoni MF, Duarte H. Transfer of the pronator quadratus motor branch for wrist extension reconstruction in brachial plexus palsy. Plastic and reconstructive surgery. 2012 Dec 1;130(6):1269-78.
- ↑ Ishida O, Ikuta Y. Analysis of Tsuge's procedure for the treatment of radial nerve paralysis. Hand surgery. 2003 Jul;8(01):17-20.
- ↑ Tsuge K. Tendon transfers for radial nerve palsy. Australian and New Zealand Journal of Surgery. 1980 Jun;50(3):267-72.
- ↑ 10.0 10.1 10.2 10.3 10.4 Hunter JM, Mackin EJ, Callahan AD, Skirven TM, Schneider LH, Osterman AL. Rehabilitation of the hand and upper extremity. InRehabilitation of the hand and upper extremity 2002 (pp. 1096-1096).
- ↑ 11.0 11.1 11.2 11.3 Richford J, Abdullah S, Norhafizah M, Juliana I, Rashdeen F, Razana A. Outcome of tendon transfers for radial nerve palsy in a Malaysian tertiary centre. Malaysian orthopaedic journal. 2018 Mar;12(1):1.