Vaccines
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Sukhi Dhaliwal, Kim Jackson, Kirenga Bamurange Liliane and Nupur Smit Shah
Introduction[edit | edit source]
Vaccination is one of the most effective ways to prevent diseases. Vaccines protect against more than 25 debilitating or life-threatening diseases, including measles, polio, diphtheria, meningitis, influenza, tetanus, typhoid and cervical cancer.[1]
A vaccine is a pharmacologic compound that improves a person's immunity to a particular disease.
- When a disease-causing bacterium or virus invades the human body, the immune system recognizes the material as foreign, usually by detecting specific protein portions of the invading organism, known as antigens.
- Vaccines contain a form of the disease-causing agent, whether it be a weakened or killed form of the microbe itself, an inactivated version of its toxins, or a protein from the surface of the microbe.
- By introducing a form of the agent, the vaccine presents the antigen to the immune system, allowing it to recognize the antigen as foreign and develop antibodies and memory T-lymphocytes against those antigens.
- This allows a more rapid and robust immune response should the body be exposed to the organism in the future.
- In the absence of vaccination, the first exposure to the natural organism may prove fatal before the immune system can mount a sufficient immune response.[2]
Currently, the majority of children receive their vaccines on time. However, nearly 20 million worldwide still miss out – putting them at risk of serious diseases, death, disability and ill health.[1]
Vaccines are a form of immunotherapy.
Different Types of Vaccines[edit | edit source]
There are many different types of vaccines in use today, they represents the different strategies used to reduce the risk of illness and disease by inducing a beneficial immune response.
- Inactivated Vaccines - use a previously virulent version of the bacteria or virus that has been inactivated (killed) with chemicals, heat or radiation.Usually do not provide protection that is as strong as live vaccines, may require several doses over time. Examples include: Hepatitis A, Rabies Vaccine, Polio Vaccine and most influenza vaccines. [3]
- Live Attenuated Vaccines - Use a weakened or inactive form of a live virus to produce an immune response. They create a strong and long lasting immune response in just 1 or 2 doses, however may not be suitable for those that are immunocompromised. Examples include: Measles, mumps, rubella, and chickenpox vaccines.[3]
- Messenger RNA Vaccine (mRNA Vaccines) - Do not use the live virus, uses mRNA inside a lipid membrane to teach cells how to make a protein that will trigger an immune response. The mRNA is protected until it gets inside the cells and translates it into the antigen protein. The mRNA lasts a few days and is naturally broken down and removed by the body, RNA vaccines are not capable of combining with human genetic code (DNA) so it cannot change or influence our genes. Examples include: Moderna COVID-19 Vaccine and Pfizer-BioNTech COVID-19 Vaccine. CDC infographic: How mRNA COVID-19 Vaccines Work [4][5][3]
- Subunit, Recombinant, Polysaccharide, and Conjugate Vaccines - Use a specific piece of the bacteria or the virus that is required to elicit a protective immune response, for example like its protein, sugar or casing around the antigen. Gives a very strong immune response , can be used on anyone that needs them; May require boosters for ongoing protection against disease. Examples include: Haemophilus influenza type B vaccine. Hepatitis B, HPV (Human papilomavirus), Whooping Cough, Pneumococcal disease, Meningococcal disease and Shingles. [3]
- Toxoid Vaccines - Use the toxin made by the bacteria to create an immune response that is targeted to the toxin and not the bacteria itself. Requires boosters for ongoing protection. Examples include: Tetanus, Diphtheria and Pertussis vaccine.[3]
- Viral Vector Vaccines - uses a modified version of a different virus as a vector to deliver instructions to our cells to stimulate an immune response. Examples include: Oxford-AstraZeneca COVID-19 vaccine uses a non replicating viral vector called ChAdOx1; Johnson & Johnson Janssen Vaccine (COVID-19). CDC infographic: How Viral Vector COVID-19 Vaccines Work [4][6][3]
Developing A New Vaccine[edit | edit source]
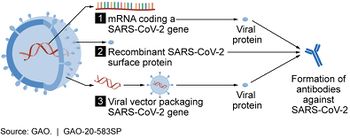
Image R: Vaccine candidate mechanisms for SARS-CoV-2 The general stages of the development cycle of a vaccine are:
- Exploratory stage
- Pre-clinical stage
- Clinical development - 3 phase process. During Phase I, small groups of people receive the trial vaccine. In Phase II, the clinical study is expanded and vaccine is given to people who have characteristics (such as age and physical health) similar to those for whom the new vaccine is intended. In Phase III, the vaccine is given to thousands of people and tested for efficacy and safety.
- Regulatory review and approval
- Manufacturing
- Quality control[7]
The 4.5 minute video below is an interesting watch
- Types of COVID-19 Vaccines available:
- Pfizer-BioNTech
- Moderna
- Johnson & Johnson's Janssen
- Oxford, AstraZeneca Vaccine
Status of other COVID-19 Vaccines within WHO EUL/PQ evaluation process can be found here. [9]
Clinical Significance[edit | edit source]
Vaccination is vital to public health. Disease prevention has been proven to prolong life expectancy and improve quality of life.
- Antivaccination movements have gained traction - diseases once thought to be eradicated or nearly eradicated have had significant outbreaks.
- Preventive measures such as vaccines are often overlooked by primary care providers and patients. For children, parents often do not know the appropriate schedule for vaccines, and therefore are often unaware of when their children are behind on vaccinations. Another common reason for missed vaccination is missed appointments for various reasons. Patient recall and reminder systems have been created and shown significant improvement in increasing vaccination compliance rates[2]
Contraindications[edit | edit source]
Contraindications to immunization are rare.
- The primary contraindication is an allergy to a vaccine or a component of the vaccine.
- Patients with a history of a compromised immune system, such as in AIDS or another immune deficiency, should use caution when vaccinating with a live attenuated vaccine.
- Live attenuated vaccines should not be given to a pregnant woman, unless there is an immediate risk (such as a polio epidemic), as the live vaccines have the potential to infect the fetus.
- Caution should be used when administering a vaccine to a child with an acute moderate to severe illness, with or without a fever. The cause of fever following vaccination in this population may be difficult to determine, whether it be continued illness or directly resulting from the vaccination. This may complicate the management of the illness.[2]
Administration[edit | edit source]
- Most human vaccines are administered by injection, although this approach is risky in the developing world where the use of injections can transmit diseases such as HIV infections.
- Live vaccines can be given orally but not killed vaccines.
- Alternatively, the use of the oral route and other mucosal surfaces have been explored as immunization route. For example, polio vaccination underwent a successful implementation via the oral route[10].
References[edit | edit source]
- ↑ 1.0 1.1 WHO Vaccines Available from:https://www.who.int/topics/vaccines/en/ (last accessed 6.6.2020)
- ↑ 2.0 2.1 2.2 Ginglen JG, Doyle MQ. Immunization. InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK459331/ (last accessed 6.6.2020)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Pollard, A.J., Bijker, E.M. A guide to vaccinology: from basic principles to new developments. Nat Rev Immunol 21, 83–100 (2021). https://doi.org/10.1038/s41577-020-00479-7
- ↑ 4.0 4.1 Mayo Clinic. Different types of Covid-19 vaccines: How they work. Available from:https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/different-types-of-covid-19-vaccines/art-20506465]] (accessed 26/01/2022)
- ↑ CDC. Understanding mRNA COVID-19 Vaccines. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/mrna.html (accessed 07/02/2022)
- ↑ CDC. Understanding Viral Vector COVID-19 Vaccines. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/viralvector.html (accessed 07/02/2022)
- ↑ CDC Vaccines Available from:https://www.cdc.gov/vaccines/basics/test-approve.html (last accessed 6.6.2020)
- ↑ Youreka Vaccine clinical trial Available from:https://www.youtube.com/watch?v=R4AUGdT3DE8&app=desktop (last accessed 6.6.2020)
- ↑ WHO. Regulation and Prequalification. Available from: https://www.who.int/teams/regulation-prequalification/eul/covid-19 (accessed 07/02/2022)
- ↑ Vaillant AA, Grella MJ. Vaccine (Vaccination). InStatPearls [Internet] 2019 Oct 21. StatPearls Publishing.Available from:https://www.statpearls.com/kb/viewarticle/30924 (last accessed 6.6.2020)