Hip Dysplasia in Adolescents and Adults: Difference between revisions
No edit summary |
No edit summary |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== | == Introduction == | ||
Hip Dysplasia is a term used to describe a variety of abnormalities in which the acetabulum is shallow or incorrectly oriented, and therefore does not properly contain the femoral head. | |||
Hip dysplasia can present in adolescence or adulthood:<ref>Pun S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5127949/#CR5 Hip dysplasia in the young adult caused by residual childhood and adolescent-onset dysplasia.] Current Reviews in Musculoskeletal Medicine [Internet]. 2016 Sep 9;9(4):427–34.</ref> | |||
A. As a residual diagnosis from infancy – | |||
# a. a patient may have had multiple treatments or surgeries throughout their life and always known their symptoms may worsen at some point, or | |||
# b. it may have been treated and resolved in infancy and been asymptomatic for number of years, with the patient having no knowledge that symptoms could reoccur in adulthood. | |||
B. As a completely new diagnosis in adolescence or adulthood | |||
Adult hip dysplasia falls into the category of ‘Young adult hip conditions’ which refers to a specialty in orthopedics focusing on hip pathologies in patients from adolescence until those roughly in their 50s. This is due to the differential diagnoses and surgeries around these types of pathologies requiring more specialist input than those of hip pathologies in older adults. | |||
Terms used: | |||
* Hip Dysplasia | |||
* Developmental Dysplasia of the hip (DDH) | |||
* Congenital Dislocation of the hip (CDH) | |||
* “Clicky hips” | |||
* “Loose hips” | |||
* Acetabular Dysplasia | |||
Hip dysplasia both in infancy and adulthood has links with early-onset hip osteoarthritis (OA)<ref>Jacobsen S, Sonne-holm S, Søballe K, Gebuhr P, Lund B. [https://pubmed.ncbi.nlm.nih.gov/16097538/ Hip dysplasia and osteoarthrosis.] Acta Orthopaedica. 2005 Jan;76(2):149–58.</ref> <ref>Kaya M, Suzuki T, Emori M, Yamashita T. [https://pubmed.ncbi.nlm.nih.gov/25331654/ Hip morphology influences the pattern of articular cartilage damage.] Knee Surgery, Sports Traumatology, Arthroscopy. 2014 Sep 11;24(6):2016–23.</ref> <ref>Reijman M, Hazes JMW, Pols HAP, Koes BW, Bierma-Zeinstra SMA. [https://pubmed.ncbi.nlm.nih.gov/15751071/ Acetabular dysplasia predicts incident osteoarthritis of the hip: The Rotterdam study.] Arthritis & Rheumatism. 2005;52(3):787–93.</ref> <ref>Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5213917/ The John Charnley Award: Redefining the Natural History of Osteoarthritis in Patients With Hip Dysplasia and Impingement.] Clinical Orthopaedics and Related Research. 2017 Feb 1;475(2):336–50.</ref>, therefore timely diagnosis is necessary to provide potential treatment options which can delay the development of OA. | |||
== Clinically Relevant Anatomy == | |||
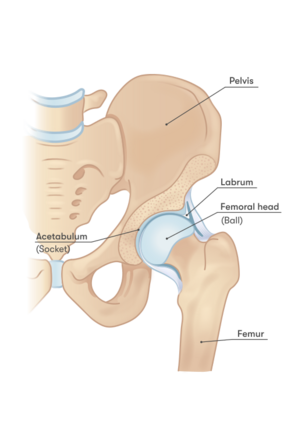
The hip joint is a synovial ball and socket joint, made up of the femoral head, which sits inside the acetabulum. The acetabulum is cup shaped, normally positioned in the pelvis facing antero-laterally. The hip joint capsule consists of circular and longitudinal fibers extending from the rim of the acetabulum, extending to the neck of the femur, and is reinforced by the iliofemoral, pubofemoral and ischiofemoral ligaments. The hip joint transmits weight from the trunk to the lower limb and allows for a wide range of movement along with stability created by the joint capsule. The acetabulum and head of the femur are covered in hyaline articular cartilage. The outer rim of the acetabulum is lined with the acetabular labrum. This helps to deepen the acetabulum, absorb shock and creates a suction seal in order to stabilize the femoral head in its socket.<ref name=":0">Palastanga N, Soames R. Anatomy and Human Movement: Structure and Function. 6th ed. London: Elsevier; 2012. (page 287-8; page 295-6)</ref> <ref>Kuntzman AJ, Tortora GJ. Anatomy and Physiology for the Manual Therapies. John Wiley & Sons; 2010. (page 244-5)</ref> The direction of the shaft of the femur in the frontal and horizontal planes also contribute to the stability of the femoral head in the acetabulum. In the horizontal plane, the femur is usually anteverted to approximately 10 degrees in adults.<ref name=":0" /> | |||
[[File:Hip anatomy.png|center|437x437px|Hip Anatomy]] | |||
There is an excellent description of the [[Hip Anatomy|hip anatomy]] in a dedicated Physiopedia article for Hip. | |||
== Pathology == | |||
A dysplastic hip consists of a shallow or incorrectly oriented acetabulum, sometimes combined with ligament laxity.<ref>Muldoon M, Gosey G, Healey R, Santore R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5479188/#:~:text=Summary%3A%20In%20this%20prospective%20observational,prevalence%20of%20hypermobility%20in%20dysplasia. Hypermobility: a Key Factor in Hip Dysplasia. A Prospective Evaluation of 266 Patients.] Journal of Hip Preservation Surgery. 2016 Sep;3(suppl_1).</ref> <ref>Ayanoğlu S, Çabuk H, Kuşku Çabuk F, Beng K, Yildirim T, Uyar Bozkurt S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8524823/ Greater presence of receptors for relaxin in the ligamentum teres of female infants who undergo open reduction for developmental dysplasia of the hip.] Journal of Orthopaedic Surgery and Research [Internet]. 2021 Oct 18;16(1).</ref> This causes unequal loading across the hip joint, and over time the acetabular labrum hypertrophies in order to compensate for the bony deficiency.<ref>Hartig-Andreasen C, Søballe K, Troelsen A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3584604/ The role of the acetabular labrum in hip dysplasia.] Acta Orthopaedica [Internet]. 2013 Feb 1;84(1):60–4.</ref> <ref>Klaue K, Durnin C, Ganz R. [https://pubmed.ncbi.nlm.nih.gov/1670443/#:~:text=In%20acetabular%20dysplasia%2C%20the%20acetabular,is%20an%20incongruent%20shallow%20acetabulum. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip.] The Journal of Bone and Joint Surgery British volume. 1991 May;73-B(3):423–9.</ref> The labrum is then prone to injury or tear. Subsequently, the suction seal which normally exists in the hip joint is lost, resulting in further instability. In some cases, the femoral shaft is anteverted or retroverted, or the inclination of femoral neck is greater than it should be, causing a ‘coxa valga’.<ref name=":0" /> | |||
Due to these pathophysiological mechanisms, secondary hip osteoarthritis develops at a faster rate in a dysplastic hip as compared to a normal hip joint. | |||
[[File:Hip dysplasia.jpeg|center|375x375px]] | |||
Acetabular dysplasia is on a spectrum, ranging from minor abnormalities in the morphology of the joint, through to more severe abnormalities, or even a dislocating hip. It is usually not possible to gauge exactly when OA will begin to develop in a dysplastic hip joint. For some, OA and a need for a THR may occur as early as in late adolescence or twenties, if diagnosis has been delayed or prior treatments unsuccessful.<ref>Pallante GD, Statz JM, Milbrandt TA, Trousdale RT. [https://pubmed.ncbi.nlm.nih.gov/31977814/ Primary Total Hip Arthroplasty in Patients 20 Years Old and Younger.] Journal of Bone and Joint Surgery. 2020 Jan 22;102(6):519–25.</ref> For others, it may be the case that less severe or asymptomatic hip dysplasia does not cause a problem or require treatment until much later in life, if at all. Due to patchy reliability of diagnoses amongst this patient cohort, it is difficult to ascertain the rates of diagnosis in relation to the severity of abnormalities. | |||
Acetabular dysplasia has more recently been categorized into 3 patterns: Global, Anterior-superior deficiency, Global deficiency and Posterior-superior deficiency. | |||
{| class="wikitable sortable mw-collapsible" | |||
|Anterior-superior: | |||
|Insufficient anterior wall of the acetabulum. | |||
|- | |||
|Global/Lateral: | |||
|Deficiency of the lateral wall of the acetabulum as well as the anterior and/or/or posterior wall of the acetabulum. | |||
|- | |||
|Posterior-Superior: | |||
|Insufficient posterior wall of the acetabulum, with associated over-coverage of the anterior acetabulum wall. This may be described as acetabular retroversion or as a pincer impingement of the femoral head against the anterior acetabular rim. | |||
|} | |||
<br> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Revision as of 18:02, 7 June 2024
Introduction[edit | edit source]
Hip Dysplasia is a term used to describe a variety of abnormalities in which the acetabulum is shallow or incorrectly oriented, and therefore does not properly contain the femoral head.
Hip dysplasia can present in adolescence or adulthood:[1]
A. As a residual diagnosis from infancy –
- a. a patient may have had multiple treatments or surgeries throughout their life and always known their symptoms may worsen at some point, or
- b. it may have been treated and resolved in infancy and been asymptomatic for number of years, with the patient having no knowledge that symptoms could reoccur in adulthood.
B. As a completely new diagnosis in adolescence or adulthood
Adult hip dysplasia falls into the category of ‘Young adult hip conditions’ which refers to a specialty in orthopedics focusing on hip pathologies in patients from adolescence until those roughly in their 50s. This is due to the differential diagnoses and surgeries around these types of pathologies requiring more specialist input than those of hip pathologies in older adults.
Terms used:
- Hip Dysplasia
- Developmental Dysplasia of the hip (DDH)
- Congenital Dislocation of the hip (CDH)
- “Clicky hips”
- “Loose hips”
- Acetabular Dysplasia
Hip dysplasia both in infancy and adulthood has links with early-onset hip osteoarthritis (OA)[2] [3] [4] [5], therefore timely diagnosis is necessary to provide potential treatment options which can delay the development of OA.
Clinically Relevant Anatomy[edit | edit source]
The hip joint is a synovial ball and socket joint, made up of the femoral head, which sits inside the acetabulum. The acetabulum is cup shaped, normally positioned in the pelvis facing antero-laterally. The hip joint capsule consists of circular and longitudinal fibers extending from the rim of the acetabulum, extending to the neck of the femur, and is reinforced by the iliofemoral, pubofemoral and ischiofemoral ligaments. The hip joint transmits weight from the trunk to the lower limb and allows for a wide range of movement along with stability created by the joint capsule. The acetabulum and head of the femur are covered in hyaline articular cartilage. The outer rim of the acetabulum is lined with the acetabular labrum. This helps to deepen the acetabulum, absorb shock and creates a suction seal in order to stabilize the femoral head in its socket.[6] [7] The direction of the shaft of the femur in the frontal and horizontal planes also contribute to the stability of the femoral head in the acetabulum. In the horizontal plane, the femur is usually anteverted to approximately 10 degrees in adults.[6]
There is an excellent description of the hip anatomy in a dedicated Physiopedia article for Hip.
Pathology[edit | edit source]
A dysplastic hip consists of a shallow or incorrectly oriented acetabulum, sometimes combined with ligament laxity.[8] [9] This causes unequal loading across the hip joint, and over time the acetabular labrum hypertrophies in order to compensate for the bony deficiency.[10] [11] The labrum is then prone to injury or tear. Subsequently, the suction seal which normally exists in the hip joint is lost, resulting in further instability. In some cases, the femoral shaft is anteverted or retroverted, or the inclination of femoral neck is greater than it should be, causing a ‘coxa valga’.[6]
Due to these pathophysiological mechanisms, secondary hip osteoarthritis develops at a faster rate in a dysplastic hip as compared to a normal hip joint.
Acetabular dysplasia is on a spectrum, ranging from minor abnormalities in the morphology of the joint, through to more severe abnormalities, or even a dislocating hip. It is usually not possible to gauge exactly when OA will begin to develop in a dysplastic hip joint. For some, OA and a need for a THR may occur as early as in late adolescence or twenties, if diagnosis has been delayed or prior treatments unsuccessful.[12] For others, it may be the case that less severe or asymptomatic hip dysplasia does not cause a problem or require treatment until much later in life, if at all. Due to patchy reliability of diagnoses amongst this patient cohort, it is difficult to ascertain the rates of diagnosis in relation to the severity of abnormalities.
Acetabular dysplasia has more recently been categorized into 3 patterns: Global, Anterior-superior deficiency, Global deficiency and Posterior-superior deficiency.
| Anterior-superior: | Insufficient anterior wall of the acetabulum. |
| Global/Lateral: | Deficiency of the lateral wall of the acetabulum as well as the anterior and/or/or posterior wall of the acetabulum. |
| Posterior-Superior: | Insufficient posterior wall of the acetabulum, with associated over-coverage of the anterior acetabulum wall. This may be described as acetabular retroversion or as a pincer impingement of the femoral head against the anterior acetabular rim. |
Clinical Presentation[edit | edit source]
add text here relating to the clinical presentation of the condition
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ Pun S. Hip dysplasia in the young adult caused by residual childhood and adolescent-onset dysplasia. Current Reviews in Musculoskeletal Medicine [Internet]. 2016 Sep 9;9(4):427–34.
- ↑ Jacobsen S, Sonne-holm S, Søballe K, Gebuhr P, Lund B. Hip dysplasia and osteoarthrosis. Acta Orthopaedica. 2005 Jan;76(2):149–58.
- ↑ Kaya M, Suzuki T, Emori M, Yamashita T. Hip morphology influences the pattern of articular cartilage damage. Knee Surgery, Sports Traumatology, Arthroscopy. 2014 Sep 11;24(6):2016–23.
- ↑ Reijman M, Hazes JMW, Pols HAP, Koes BW, Bierma-Zeinstra SMA. Acetabular dysplasia predicts incident osteoarthritis of the hip: The Rotterdam study. Arthritis & Rheumatism. 2005;52(3):787–93.
- ↑ Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ. The John Charnley Award: Redefining the Natural History of Osteoarthritis in Patients With Hip Dysplasia and Impingement. Clinical Orthopaedics and Related Research. 2017 Feb 1;475(2):336–50.
- ↑ 6.0 6.1 6.2 Palastanga N, Soames R. Anatomy and Human Movement: Structure and Function. 6th ed. London: Elsevier; 2012. (page 287-8; page 295-6)
- ↑ Kuntzman AJ, Tortora GJ. Anatomy and Physiology for the Manual Therapies. John Wiley & Sons; 2010. (page 244-5)
- ↑ Muldoon M, Gosey G, Healey R, Santore R. Hypermobility: a Key Factor in Hip Dysplasia. A Prospective Evaluation of 266 Patients. Journal of Hip Preservation Surgery. 2016 Sep;3(suppl_1).
- ↑ Ayanoğlu S, Çabuk H, Kuşku Çabuk F, Beng K, Yildirim T, Uyar Bozkurt S. Greater presence of receptors for relaxin in the ligamentum teres of female infants who undergo open reduction for developmental dysplasia of the hip. Journal of Orthopaedic Surgery and Research [Internet]. 2021 Oct 18;16(1).
- ↑ Hartig-Andreasen C, Søballe K, Troelsen A. The role of the acetabular labrum in hip dysplasia. Acta Orthopaedica [Internet]. 2013 Feb 1;84(1):60–4.
- ↑ Klaue K, Durnin C, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. The Journal of Bone and Joint Surgery British volume. 1991 May;73-B(3):423–9.
- ↑ Pallante GD, Statz JM, Milbrandt TA, Trousdale RT. Primary Total Hip Arthroplasty in Patients 20 Years Old and Younger. Journal of Bone and Joint Surgery. 2020 Jan 22;102(6):519–25.