Communication in Chronic Pain Conditions: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Robyn Holton|Robyn Holton]], [[User:Frank Ryan|Frank Ryan]], [[User:Shawn Swartz|Shawn Swartz]], [[User:Elaine McDermott|Elaine McDermott]], [[User:Noel McLoughlin|Noel McLoughlin]], [[User:Zeeshan Hussain Mundh|Zeeshan Mundhas]]</div> | '''Original Editor '''- [[User:Robyn Holton|Robyn Holton]], [[User:Frank Ryan|Frank Ryan]], [[User:Shawn Swartz|Shawn Swartz]], [[User:Elaine McDermott|Elaine McDermott]], [[User:Noel McLoughlin|Noel McLoughlin]], [[User:Zeeshan Hussain Mundh|Zeeshan Mundhas]]</div> | ||
| Line 13: | Line 10: | ||
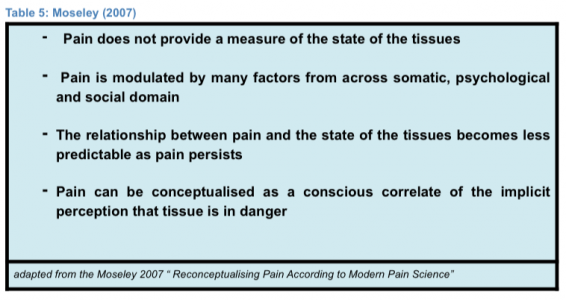
Many believe [[Pain Behaviours|pain]] is a simple sensation that you get after, lets say “closing the car door on your finger”. It’s easy to understand in a structural model of reasoning, which believes that the more pain you get the more tissue damage you are causing. Although it is not as simple as this, and much of the persistent pain that physiotherapists see on a everyday basis would not be adequately addressed by this model of thinking. Recent authors have indicated that pain could be a measure of potential threat rather than an indication of tissue health.<ref name="Moseley 2003" /><br> Lorimer Moseley’s 2007 paper “Reconceptualising Pain According to Modern Pain Science” suggests that :<ref name="Moseley 2007">Moseley, G. (2007). Reconceptualising pain according to modern pain science. Phys. Ther. Rev., 12(3), pp.169-178.</ref><br> [[Image:TABLE5pain.png|center|600x300px]] | Many believe [[Pain Behaviours|pain]] is a simple sensation that you get after, lets say “closing the car door on your finger”. It’s easy to understand in a structural model of reasoning, which believes that the more pain you get the more tissue damage you are causing. Although it is not as simple as this, and much of the persistent pain that physiotherapists see on a everyday basis would not be adequately addressed by this model of thinking. Recent authors have indicated that pain could be a measure of potential threat rather than an indication of tissue health.<ref name="Moseley 2003" /><br> Lorimer Moseley’s 2007 paper “Reconceptualising Pain According to Modern Pain Science” suggests that :<ref name="Moseley 2007">Moseley, G. (2007). Reconceptualising pain according to modern pain science. Phys. Ther. Rev., 12(3), pp.169-178.</ref><br> [[Image:TABLE5pain.png|center|600x300px]] | ||
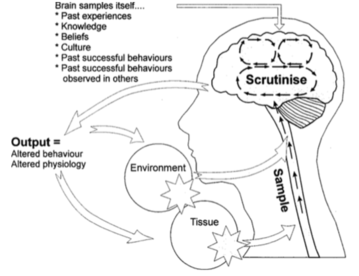
If we look at the work of Louis Gifford and the Mature Organism Model <ref name="Gifford 1998" />(1998) we see that when we get an input [[Nociception|nociceptive stimuli]] the nerve impulse travels to the brain and is sampled against a number of different factors such as: | If we look at the work of Louis Gifford and the Mature Organism Model <ref name="Gifford 1998">Gifford LS. Topical issues in pain 1. Whiplash–science and management. Fear avoidance beliefs and behaviour. 1998.</ref>(1998) we see that when we get an input [[Nociception|nociceptive stimuli]] the nerve impulse travels to the brain and is sampled against a number of different factors such as: | ||
[[Image: | [[Image:MatureOModel picture.png|border|right|359x359px]] | ||
* Proprioception - the perception of the position of the body in space. The information is received from joints, muscles, tendons and skin | |||
* Interoception - information from nociceptors about the internal state of our body and the thermal, mechanical and chemical state of organs and tissues. | |||
* Exteroception - the five senses (sight, taste, smell, touch, hearing and balance) | |||
* Cognition - Pain can be linked to knowledge, memory, belief, expectation, feelings, mood, perceptions.<br> | |||
After the brain scrutinises all these unconscious pieces of information it asks itself, “How dangerous is this really?” Pain is a good thing and tries to protect our tissues, we as physiotherapists need to monitor if pain is adaptive or maladaptive .<ref name="Stewart 2014">Stewart M. The road to pain reconceptualisation: Do metaphors help or hinder the journey?. Pain and Rehabilitation-the Journal of Physiotherapy Pain Association. 2014 Jan 1;2014(36):24-31.</ref> | |||
== Every Chronic Pain Was Once Acute == | == Every Chronic Pain Was Once Acute == | ||
As pain carries on the patient may become more anxious, stressed, helpless, sedentary, further reinforcing the brain’s choice to cause pain.<ref name="Moseley 2003">Moseley | As pain carries on the patient may become more anxious, stressed, helpless, sedentary, further reinforcing the brain’s choice to cause pain.<ref name="Moseley 2003">Moseley GL. A pain neuromatrix approach to patients with chronic pain. Manual therapy. 2003 Aug 1;8(3):130-40.</ref>,<ref name="Gifford 2000">Gifford L. Topical Issues in Pain 2: Biopsychosocial assessment and management Relationships and pain. AuthorHouse; 2013 Sep 9.</ref>We often see a fire alarm that goes off from a piece of burning toast similarly our bodies alarm system can malfunction in much the same way if the body becomes hypersensitive..<br>More and more research is starting to look at pain as a disorder rather than a symptom. <ref name="Bourke 2014">Bourke, J. The story of pain. 2014. London Oxford University Press.</ref> Just as asthma, diabetes or epileptic patients are educated on the mechanisms of their disease and how their actions could make their condition better or worse. Persistent pain patients should be introduced to their condition by facilitating dialogical critical thinking in a similar manner .<ref name="Yelland 2011" /> Often it can be easier to address peoples lack of care for their pain when patients have co-morbidities because physiotherapists are able to compare how poorly their pain is being managed. If we take a moment to look at Diabetes and persistent pain through the same lens and imagine that doctors had a patient coming in every 3 days for an insulin injection and an overnight stay because they weren't managing their diabetes correctly there would be a problem. In a physiotherapy setting, if a patient was coming into your clinic every 3 days for some manual therapy to decrease their pain while they otherwise poorly manage their condition, this would not be right. | ||
== Neuroscience Education == | |||
According to Louw et al. (2011) Neuroscience education is a cognitive-based intervention that aims at reducing pain and maladaptive behaviours by guiding patients to grasp an understanding of the mechanisms underpinning their pain experience.<ref name="Louw et al. 2011">Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011 Dec 1;92(12):2041-56.</ref> This semi-complex information needs to be delivered to the patient in a way that is clear and easy to understand. Language and other communication techniques such as drawings, pictures, videos, workbooks can aid patient learning. Research shows that traditionally clinicians tend to underestimate patients ability to understand complex pain, when in fact patients are interested in learning about their pain.<ref name="Louw et al. 2011" /> Multiple studies have shown that Neuroscience Education combined with graded exercise is in line with the best evidence available for treating persistent pain.<ref name="Louw et al. 2011" /> Resulting in decreased fear, pain, cognition and physical performance, increased pain thresholds during exercises, and reduced brain activity, especially the amygdala, that is usually involved with pain.<ref name="Louw et al. 2011" /><ref name="Veinante et al. 2013">Veinante P, Yalcin I, Barrot M. The amygdala between sensation and affect: a role in pain. Journal of molecular psychiatry. 2013 Dec 1;1(1):9.</ref><br> | |||
=== Explaining Pain: How to Do it in Under Ten Minutes === | === Explaining Pain: How to Do it in Under Ten Minutes === | ||
| Line 45: | Line 35: | ||
|} | |} | ||
== Clinical Example: Osteoarthritis == | |||
= | When explaining a condition such as osteoarthritis to a patient we must consider what their viewpoint of the condition must be. Osteoarthritis is a condition of cartilage degeneration, subchondral bone stiffening and active new bone formation<ref name="Heuts et al" />. Osteoarthritis is a complex sensory and emotional experience. An individual’s psychological characteristics and immediate psychological contest in which pain is experienced both influence their perception of pain<ref name="Hunter et al" />. | ||
Research has utilised qualitative methods and focus groups to establish the patient’s point of view. A common theme that is emerging is that patients are sometimes dissatisfied with the overall level of understanding, help and information that is given to them by healthcare professionals<ref name="Hill et al" />. Patients also expressed concern that there was a lack of understanding by healthcare professionals as to the impact that osteoarthritis can have on an individual’s life<ref name="Hill et al" />. As physiotherapists, we must be aware of current and alternative treatments for OA (hydrotherapy, acupuncture etc) as contradictory information being given to the patient from different sources may lead to confusion as to what exactly they should be doing<ref name="Hill et al" />. | |||
Somers et al highlights that patients may adopt certain attitudes towards pain<ref name="Somers et al" />; Patients who are pain catastrophizing tend to focus on and magnify their pain sensations. This group of patients tend to feel helpless in the face of pain. Patients who adopt this stance report higher levels of pain, have higher levels of psychological and physical disability. The second stance is patients who have pain related fear. They have a fear of physical activity as a result of feeling vulnerable to pain during activity. This group are more likely to engage in avoidance behaviours such as avoiding movement<ref name="Somers et al" />. We as physiotherapists must remember that OA patients with a fear of engaging in painful movements may be hesitant to engage in physical activity. This can contribute to a vicious cycle of a more restricted and a physically inactive lifestyle which will lead to increased pain and disability<ref name="Somers et al">Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Waters SJ, Riordan PA, Blumenthal JA, McKee DC, LaCaille L, Tucker JM, Schmitt D. Pain catastrophizing and pain-related fear in osteoarthritis patients: relationships to pain and disability. Journal of pain and symptom management. 2009 May 1;37(5):863-72.</ref> | |||
Hendry et alconducted qualitative research on primary care patients with OA<ref name="Hendry et al">Hendry M, Williams NH, Markland D, Wilkinson C, Maddison P. Why should we exercise when our knees hurt? A qualitative study of primary care patients with osteoarthritis of the knee. Family practice. 2006 Oct 1;23(5):558-67.</ref>. They found that personal experience, aetiology of arthritis and motivational factors all influenced compliance rates towards physical activity. Some patients believed that their joint problems were a direct result of heavy physical activity<ref name="Hill et al">Hill S, Dziedzic KS, Nio Ong B. Patients' perceptions of the treatment and management of hand osteoarthritis: a focus group enquiry. Disability and rehabilitation. 2011 Jan 1;33(19-20):1866-72.</ref>. This is where we as clinicians must be aware that patients may present questions such as; '''‘why should we exercise when our knees hurt?’''' In the same study patients were asking; '''‘if it is wear and tear on the bone, is it helping to do all this exercise, walking and that?’''' As physiotherapists we must be careful with our choice of words, phrases such as ‘wear and tear’ may be misinterpreted by some patients and lead to further maladaptive behaviour. Grime et al established that an ongoing concern of musculoskeletal professionals is that the use of this ‘wear and tear’ explanation often leads to decreased physical activity to avoid further ‘wearing of the joint’<ref name="Grime et al" />. | |||
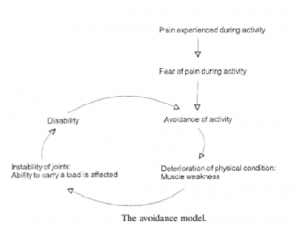
< | A unique approach adopted by a number of patients in the same study by Grime et al was the ‘use it or lose it’ approach<ref name="Grime et al">Grime J, Richardson JC, Ong BN. Perceptions of joint pain and feeling well in older people who reported being healthy: a qualitative study. Br J Gen Pract. 2010 Aug 1;60(577):597-603.</ref>. This simply put was use the joint or lose your functional ability. As physiotherapists we could utilise a similar approach to get our patients to comply with the physical exercise that we have prescribed as an intervention. Through effective communication we can increase a patient’s self efficacy and reduce their level of physical disability<ref name="Hunter et al" />. Patients with higher self-efficacy for pain control had higher thresholds for pain stimuli<ref name="Hunter et al">Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheumatic Disease Clinics of North America. 2008 Aug 1;34(3):623-43.</ref>. Exercise has been shown to have a positive effect on functional ability in patients with OA<ref name="Heuts et al" />. We as physiotherapists must consider the role of pain-related fear in patients with OA and investigate different treatment approaches to combat this behaviour<ref name="Heuts et al">Heuts PH, Vlaeyen JW, Roelofs J, de Bie RA, Aretz K, van Weel C, van Schayck OC. Pain-related fear and daily functioning in patients with osteoarthritis. Pain. 2004 Jul 1;110(1-2):228-35.</ref>. [[Image:Avoidance model 2.PNG|border|right|300x300px]] | ||
Scopaz et al suggest psychological factors such as anxiety, fear and depression may also be related to physical function in patients with OA of the knee<ref name="Scopaz et al" />. Further to this, a model of fear-avoidance suggests that patients can either be adaptive and non-adaptive in their approach to their pain and functional ability<ref name="Scopaz et al" /> This model indicates that anxiety + fear-avoidance beliefs are significant predictors of self-report physical function in patients with knee OA<ref name="Scopaz et al">Scopaz KA, Piva SR, Wisniewski S, Fitzgerald GK. Relationships of fear, anxiety, and depression with physical function in patients with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation. 2009 Nov 1;90(11):1866-73.</ref>. Following on from this, we may also consider the avoidance model presented by Dekker et al<ref name="Dekker et al">Dekker J, Tola P, Aufdemkampe G, Winckers M. Negative affect, pain and disability in osteoarthritis patients: the mediating role of muscle weakness. Behaviour research and therapy. 1993 Feb 1;31(2):203-6.</ref>. This model indicates that a decreased muscle strength as a result of activity avoidance leads to activity limitations<ref name="Holla et al">Holla JF, van der Leeden M, Knol DL, Peter WF, Roorda LD, Lems WF, Wesseling J, Steultjens MP, Dekker J. Avoidance of activities in early symptomatic knee osteoarthritis: results from the CHECK cohort. Annals of Behavioral Medicine. 2012 Aug 1;44(1):33-42.</ref>. | |||
== Conclusion == | |||
< | It is important to recognise maladaptive behaviour and fear-avoidance when treating patients presenting with chronic pain. The approach and the language used when treating patients with chronic pain how we communicate can be as effective as the techniques we use. Avoid the use of phrases that can add to fear such as wear and tear as these can increase fear and maladaptive behaviours. Focus on: | ||
* Reassuring the patient that movement is beneficial | |||
* Explaining the benefits of exercise | |||
* Recognising and appreciating the patient's attitude and feelings towards their pain | |||
* Improving compliance and adherence to your treatment plan by explaining their condition in clear, simple language | |||
* Providing a simple, graduated exercise programme that fits into the patient's needs and lifestyle<nowiki/>''<nowiki/>'' | |||
==References== | ==References== | ||
<references /> | <references /> | ||
[[Category:Effective Communication]] | [[Category:Effective Communication]] | ||
Revision as of 02:59, 11 May 2020
Introduction[edit | edit source]
Acute pain conditions have a very good rate of healing, but health care systems still find that a large portion of these patients go on to experience persistent (chronic) pain and maladaptive behaviours .[1],[2] As a result Persistent Pain conditions place a huge strain on the healthcare system and economy .[1] Modern pain research tells us that often patient beliefs play a huge role in the transition from acute pain to chronicity. By better understanding patient beliefs and positively influencing them with reassurance and compassion we can better manage patients perception of pain .[1],[3] We know from nursing literature that pain is the most common reason for an individual to seek medical advice .[4] At times Healthcare Professionals can negatively impact patients beliefs about pain. It is common that some patients feel that their stories haven’t been listened to and consequently their pain is not validated.[5]
What is Pain?[edit | edit source]
Many believe pain is a simple sensation that you get after, lets say “closing the car door on your finger”. It’s easy to understand in a structural model of reasoning, which believes that the more pain you get the more tissue damage you are causing. Although it is not as simple as this, and much of the persistent pain that physiotherapists see on a everyday basis would not be adequately addressed by this model of thinking. Recent authors have indicated that pain could be a measure of potential threat rather than an indication of tissue health.[6]
Lorimer Moseley’s 2007 paper “Reconceptualising Pain According to Modern Pain Science” suggests that :[7]
If we look at the work of Louis Gifford and the Mature Organism Model [8](1998) we see that when we get an input nociceptive stimuli the nerve impulse travels to the brain and is sampled against a number of different factors such as:
- Proprioception - the perception of the position of the body in space. The information is received from joints, muscles, tendons and skin
- Interoception - information from nociceptors about the internal state of our body and the thermal, mechanical and chemical state of organs and tissues.
- Exteroception - the five senses (sight, taste, smell, touch, hearing and balance)
- Cognition - Pain can be linked to knowledge, memory, belief, expectation, feelings, mood, perceptions.
After the brain scrutinises all these unconscious pieces of information it asks itself, “How dangerous is this really?” Pain is a good thing and tries to protect our tissues, we as physiotherapists need to monitor if pain is adaptive or maladaptive .[9]
Every Chronic Pain Was Once Acute[edit | edit source]
As pain carries on the patient may become more anxious, stressed, helpless, sedentary, further reinforcing the brain’s choice to cause pain.[6],[10]We often see a fire alarm that goes off from a piece of burning toast similarly our bodies alarm system can malfunction in much the same way if the body becomes hypersensitive..
More and more research is starting to look at pain as a disorder rather than a symptom. [11] Just as asthma, diabetes or epileptic patients are educated on the mechanisms of their disease and how their actions could make their condition better or worse. Persistent pain patients should be introduced to their condition by facilitating dialogical critical thinking in a similar manner .[5] Often it can be easier to address peoples lack of care for their pain when patients have co-morbidities because physiotherapists are able to compare how poorly their pain is being managed. If we take a moment to look at Diabetes and persistent pain through the same lens and imagine that doctors had a patient coming in every 3 days for an insulin injection and an overnight stay because they weren't managing their diabetes correctly there would be a problem. In a physiotherapy setting, if a patient was coming into your clinic every 3 days for some manual therapy to decrease their pain while they otherwise poorly manage their condition, this would not be right.
Neuroscience Education[edit | edit source]
According to Louw et al. (2011) Neuroscience education is a cognitive-based intervention that aims at reducing pain and maladaptive behaviours by guiding patients to grasp an understanding of the mechanisms underpinning their pain experience.[12] This semi-complex information needs to be delivered to the patient in a way that is clear and easy to understand. Language and other communication techniques such as drawings, pictures, videos, workbooks can aid patient learning. Research shows that traditionally clinicians tend to underestimate patients ability to understand complex pain, when in fact patients are interested in learning about their pain.[12] Multiple studies have shown that Neuroscience Education combined with graded exercise is in line with the best evidence available for treating persistent pain.[12] Resulting in decreased fear, pain, cognition and physical performance, increased pain thresholds during exercises, and reduced brain activity, especially the amygdala, that is usually involved with pain.[12][13]
Explaining Pain: How to Do it in Under Ten Minutes[edit | edit source]
Clinical Example: Osteoarthritis[edit | edit source]
When explaining a condition such as osteoarthritis to a patient we must consider what their viewpoint of the condition must be. Osteoarthritis is a condition of cartilage degeneration, subchondral bone stiffening and active new bone formation[14]. Osteoarthritis is a complex sensory and emotional experience. An individual’s psychological characteristics and immediate psychological contest in which pain is experienced both influence their perception of pain[15].
Research has utilised qualitative methods and focus groups to establish the patient’s point of view. A common theme that is emerging is that patients are sometimes dissatisfied with the overall level of understanding, help and information that is given to them by healthcare professionals[16]. Patients also expressed concern that there was a lack of understanding by healthcare professionals as to the impact that osteoarthritis can have on an individual’s life[16]. As physiotherapists, we must be aware of current and alternative treatments for OA (hydrotherapy, acupuncture etc) as contradictory information being given to the patient from different sources may lead to confusion as to what exactly they should be doing[16].
Somers et al highlights that patients may adopt certain attitudes towards pain[17]; Patients who are pain catastrophizing tend to focus on and magnify their pain sensations. This group of patients tend to feel helpless in the face of pain. Patients who adopt this stance report higher levels of pain, have higher levels of psychological and physical disability. The second stance is patients who have pain related fear. They have a fear of physical activity as a result of feeling vulnerable to pain during activity. This group are more likely to engage in avoidance behaviours such as avoiding movement[17]. We as physiotherapists must remember that OA patients with a fear of engaging in painful movements may be hesitant to engage in physical activity. This can contribute to a vicious cycle of a more restricted and a physically inactive lifestyle which will lead to increased pain and disability[17]
Hendry et alconducted qualitative research on primary care patients with OA[18]. They found that personal experience, aetiology of arthritis and motivational factors all influenced compliance rates towards physical activity. Some patients believed that their joint problems were a direct result of heavy physical activity[16]. This is where we as clinicians must be aware that patients may present questions such as; ‘why should we exercise when our knees hurt?’ In the same study patients were asking; ‘if it is wear and tear on the bone, is it helping to do all this exercise, walking and that?’ As physiotherapists we must be careful with our choice of words, phrases such as ‘wear and tear’ may be misinterpreted by some patients and lead to further maladaptive behaviour. Grime et al established that an ongoing concern of musculoskeletal professionals is that the use of this ‘wear and tear’ explanation often leads to decreased physical activity to avoid further ‘wearing of the joint’[19].
A unique approach adopted by a number of patients in the same study by Grime et al was the ‘use it or lose it’ approach[19]. This simply put was use the joint or lose your functional ability. As physiotherapists we could utilise a similar approach to get our patients to comply with the physical exercise that we have prescribed as an intervention. Through effective communication we can increase a patient’s self efficacy and reduce their level of physical disability[15]. Patients with higher self-efficacy for pain control had higher thresholds for pain stimuli[15]. Exercise has been shown to have a positive effect on functional ability in patients with OA[14]. We as physiotherapists must consider the role of pain-related fear in patients with OA and investigate different treatment approaches to combat this behaviour[14].
Scopaz et al suggest psychological factors such as anxiety, fear and depression may also be related to physical function in patients with OA of the knee[20]. Further to this, a model of fear-avoidance suggests that patients can either be adaptive and non-adaptive in their approach to their pain and functional ability[20] This model indicates that anxiety + fear-avoidance beliefs are significant predictors of self-report physical function in patients with knee OA[20]. Following on from this, we may also consider the avoidance model presented by Dekker et al[21]. This model indicates that a decreased muscle strength as a result of activity avoidance leads to activity limitations[22].
Conclusion[edit | edit source]
It is important to recognise maladaptive behaviour and fear-avoidance when treating patients presenting with chronic pain. The approach and the language used when treating patients with chronic pain how we communicate can be as effective as the techniques we use. Avoid the use of phrases that can add to fear such as wear and tear as these can increase fear and maladaptive behaviours. Focus on:
- Reassuring the patient that movement is beneficial
- Explaining the benefits of exercise
- Recognising and appreciating the patient's attitude and feelings towards their pain
- Improving compliance and adherence to your treatment plan by explaining their condition in clear, simple language
- Providing a simple, graduated exercise programme that fits into the patient's needs and lifestyle
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. The Annals of Family Medicine. 2013 Nov 1;11(6):527-34.
- ↑ Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. Bmj. 1998 May 2;316(7141):1356.
- ↑ Moseley GL, Butler D. Explain pain. Clinical Journal of Pain. 2003;20:324-30.
- ↑ Nair M, Peate I, editors. Fundamentals of Applied Pathophysiology: An essential guide for nursing students. John Wiley & Sons; 2009 Mar 24.
- ↑ 5.0 5.1 Yelland M. What do patients really want?. International Musculoskeletal Medicine. 2011 Jan 1;33(1):1.
- ↑ 6.0 6.1 Moseley GL. A pain neuromatrix approach to patients with chronic pain. Manual therapy. 2003 Aug 1;8(3):130-40.
- ↑ Moseley, G. (2007). Reconceptualising pain according to modern pain science. Phys. Ther. Rev., 12(3), pp.169-178.
- ↑ Gifford LS. Topical issues in pain 1. Whiplash–science and management. Fear avoidance beliefs and behaviour. 1998.
- ↑ Stewart M. The road to pain reconceptualisation: Do metaphors help or hinder the journey?. Pain and Rehabilitation-the Journal of Physiotherapy Pain Association. 2014 Jan 1;2014(36):24-31.
- ↑ Gifford L. Topical Issues in Pain 2: Biopsychosocial assessment and management Relationships and pain. AuthorHouse; 2013 Sep 9.
- ↑ Bourke, J. The story of pain. 2014. London Oxford University Press.
- ↑ 12.0 12.1 12.2 12.3 Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011 Dec 1;92(12):2041-56.
- ↑ Veinante P, Yalcin I, Barrot M. The amygdala between sensation and affect: a role in pain. Journal of molecular psychiatry. 2013 Dec 1;1(1):9.
- ↑ 14.0 14.1 14.2 Heuts PH, Vlaeyen JW, Roelofs J, de Bie RA, Aretz K, van Weel C, van Schayck OC. Pain-related fear and daily functioning in patients with osteoarthritis. Pain. 2004 Jul 1;110(1-2):228-35.
- ↑ 15.0 15.1 15.2 Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheumatic Disease Clinics of North America. 2008 Aug 1;34(3):623-43.
- ↑ 16.0 16.1 16.2 16.3 Hill S, Dziedzic KS, Nio Ong B. Patients' perceptions of the treatment and management of hand osteoarthritis: a focus group enquiry. Disability and rehabilitation. 2011 Jan 1;33(19-20):1866-72.
- ↑ 17.0 17.1 17.2 Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Waters SJ, Riordan PA, Blumenthal JA, McKee DC, LaCaille L, Tucker JM, Schmitt D. Pain catastrophizing and pain-related fear in osteoarthritis patients: relationships to pain and disability. Journal of pain and symptom management. 2009 May 1;37(5):863-72.
- ↑ Hendry M, Williams NH, Markland D, Wilkinson C, Maddison P. Why should we exercise when our knees hurt? A qualitative study of primary care patients with osteoarthritis of the knee. Family practice. 2006 Oct 1;23(5):558-67.
- ↑ 19.0 19.1 Grime J, Richardson JC, Ong BN. Perceptions of joint pain and feeling well in older people who reported being healthy: a qualitative study. Br J Gen Pract. 2010 Aug 1;60(577):597-603.
- ↑ 20.0 20.1 20.2 Scopaz KA, Piva SR, Wisniewski S, Fitzgerald GK. Relationships of fear, anxiety, and depression with physical function in patients with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation. 2009 Nov 1;90(11):1866-73.
- ↑ Dekker J, Tola P, Aufdemkampe G, Winckers M. Negative affect, pain and disability in osteoarthritis patients: the mediating role of muscle weakness. Behaviour research and therapy. 1993 Feb 1;31(2):203-6.
- ↑ Holla JF, van der Leeden M, Knol DL, Peter WF, Roorda LD, Lems WF, Wesseling J, Steultjens MP, Dekker J. Avoidance of activities in early symptomatic knee osteoarthritis: results from the CHECK cohort. Annals of Behavioral Medicine. 2012 Aug 1;44(1):33-42.