Patellofemoral Pain Syndrome and Hip Strength: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Kim Jackson moved page Relationship Between Hip Muscle Strength and Patellofemoral Pain Syndrome to Patellofemoral Pain Syndrome and Hip Strength: More appropriate title) |
||
| (34 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original | '''Original Editors ''' - [[User:Ajay Upadhyay|Ajay Upadhyay]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Iliotibial tract.jpg|right|frameless]] | |||
[[Patellofemoral Pain Syndrome|Patellofemoral pain syndrome]] (PFPS) is one of the most common conditions limiting athletes. There is a growing body of evidence suggesting that dysfunction at the hip may be a contributing factor in PFPS.<ref>Meira EP, Brumitt J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445210/ Influence of the hip on patients with patellofemoral pain syndrome: a systematic review]. Sports health. 2011 Sep;3(5):455-65.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445210/<nowiki/>(accessed 2.12.2021)</ref> | |||
Numerous studies have interpreted anatomic and [[Biomechanics|biomechanical]] factors for PFPS. Traditionally, research and clinical practice have focused on an imbalance between the [[Vastus Lateralis|vastus lateralis]] (VO) and the [[Vastus Medialis Oblique|vastus medialis oblique]] (VMO) that can lead to increased lateral stress in the [[Patellofemoral Joint|patellofemoral joint]]. This abnormal patellar tracking (secondary to an imbalance in [[Quadriceps Muscle|quadriceps]] muscle performance) is thought to result in PFPS. Nonoperative treatments have focused mainly on developing strength and balance in quadriceps muscles, particularly VMO. Although quadriceps exercise is the most commonly prescribed intervention, many patients experience a decrease in pain and dysfunction but not total resolution.<ref name=":0">Na Y, Han C, Shi Y, Zhu Y, Ren Y, Liu W. [https://journals.sagepub.com/doi/full/10.1177/23259671211017503 Is Isolated Hip Strengthening or Traditional Knee-Based Strengthening More Effective in Patients With Patellofemoral Pain Syndrome?] A Systematic Review With Meta-analysis. Orthopaedic Journal of Sports Medicine. 2021 Jul 28;9(7):23259671211017503.Available:https://journals.sagepub.com/doi/full/10.1177/23259671211017503 (accessed 2.12.2021)</ref> | |||
= | Recently, PFPS has been proposed to be related to strength deficits of the [[Hip Anatomy|hip musculature]] and [[Core stability|core]] endurance. In biomechanical studies, persons with PFPS have demonstrated excessive hip internal rotation and hip adduction as well as weak hip abductors, external rotators, and hip extensors compared with pain-free individuals.<ref name=":0" /> | ||
A 2018 sytematic review concluded that hip and knee strengthening is not only effective, but is also superior to knee strengthening alone for decreasing [[Pain Assessment|pain intensity]] and improving activity in people with patellofemoral pain.<ref name=":1">Nascimento LR, Teixeira-Salmela LF, Souza RB, Resende RA. [https://www.jospt.org/doi/10.2519/jospt.2018.7365 Hip and knee strengthening is more effective than knee strengthening alone for reducing pain and improving activity in individuals with patellofemoral pain: a systematic review with meta-analysis.] journal of orthopaedic & sports physical therapy. 2018 Jan;48(1):19-31. Available:https://www.jospt.org/doi/10.2519/jospt.2018.7365 (accessed 2.12.2021)</ref> | |||
== | == Physiotherapy == | ||
A 2018 systematic review confirmed that isolated hip strengthening and knee strengthening were equivalent for treatment of PFPS. However, hip strengthening alone has been proven to reduce pain and improve function in people with PFPS, and so has quadriceps strengthening alone. | |||
The best option is to perform both quad hip strengthening exercises ie [[Strength Training|Strength training]] of the hip muscles, accompanied by strengthening of [[Knee|knee muscles]], should be included in clinical management of individuals with patellofemoral pain in order to reduce pain and improve activity.<ref name=":1" /> | |||
== | == Anatomy == | ||
[[File:PFJ-ligaments.jpg|right|frameless]] | |||
The patella is the largest sesamoid bone. It is located within the complex of the quadriceps and patellar tendon. Through its articulation with the femoral trochlea, the patellofemoral joint forms a highly complex unit with potential for joint instability. Patellofemoral joint stability is multifactorial and can be categorized into static and dynamic stabilizers.<ref>Rhee, S. J., Pavlou, G., Oakley, J., Barlow, D., & Haddad, F. Modern management of patellar instability. International Orthopaedics. 2012; Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3508055/pdf/264_2012_Article_1669.pdf (accessed 2.12.2021)</ref> See here for more information [[Patellofemoral Joint]] | |||
== Biomechanics == | |||
See [[Clinical Biomechanics of Patellofemoral Pain Syndrome]]<br> | |||
== | == Strength of hip abductors and external rotators in PFPS == | ||
During ambulation hip abductors and external rotator muscle group act eccentrically to control the motion of hip adduction and hip internal rotation, respectively.<ref name="p0">Maria Zulluga. Sports physiotherapy applied science and practice:churchil livingstone,587-611.</ref> | |||
= | Weakness in the abductors may allow for excessive femoral adduction and this, in turn, may lead to more abducted, or valgus, position of the knee. Knee valgus is believed to increase the lateral force acting on the patella.<ref name="p1">David C, Reid: “Sports injury and assessment and rehabilitation”, Churchill Livingstone. 1992, pgs 345-398.</ref> | ||
Weakness of the hip external rotators may allow for excessive femoral internal rotation and this may lead to increased contact pressure between the lateral femoral condyle and the lateral facet of the patella. <ref name="p9">Robin EL. A rational approach to the treatment of patellofemoral pain. Clin Orthop 1979;144:107-109.</ref> | |||
== | Hip external rotators and abductors are also contributing in pelvic stability and leg alignment by eccentrically controlling femoral internal rotation and influencing hip adduction during weight bearing activities.<ref name="p7">Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med 2002;36:95-101.</ref><ref name="p8">I.A. Kapanji. The physiology of joints. 5th ed;2,100-101.</ref> | ||
Weakness of these muscles may increase medial femoral rotation, valgus knee moments, or cause a gluteus medius gait. These deviations may alter the adduction/abduction moments at the hip or lead to an increased Q-angle, which may subsequently alter tracking of the patella, increase compressive forces on the patellofemoral joint, and ultimately lead to knee pain.<ref name="p9" /> | |||
== | Theoretically, weakness of the abductors and external rotators may be associated with poor control of eccentric femoral adduction and internal rotation during weight-bearing activities, leading to misalignment of patellofemoral joint as the femur medially rotates underneath the patella.<ref name="p6">Insall J. Current Concepts Review: patellar pain. J Bone Joint Surg Am. 1982;64:147-152.</ref><ref name="p9" /><ref name="p0" /><br> | ||
== References == | |||
<references /> | |||
<br><br> | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 09:58, 24 January 2022
Original Editors - Ajay Upadhyay
Top Contributors - Ajay Upadhyay, 127.0.0.1, WikiSysop, Kim Jackson, Lucinda hampton, Admin and Wanda van Niekerk
Introduction[edit | edit source]
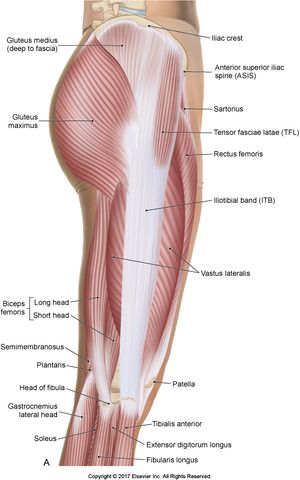
Patellofemoral pain syndrome (PFPS) is one of the most common conditions limiting athletes. There is a growing body of evidence suggesting that dysfunction at the hip may be a contributing factor in PFPS.[1]
Numerous studies have interpreted anatomic and biomechanical factors for PFPS. Traditionally, research and clinical practice have focused on an imbalance between the vastus lateralis (VO) and the vastus medialis oblique (VMO) that can lead to increased lateral stress in the patellofemoral joint. This abnormal patellar tracking (secondary to an imbalance in quadriceps muscle performance) is thought to result in PFPS. Nonoperative treatments have focused mainly on developing strength and balance in quadriceps muscles, particularly VMO. Although quadriceps exercise is the most commonly prescribed intervention, many patients experience a decrease in pain and dysfunction but not total resolution.[2]
Recently, PFPS has been proposed to be related to strength deficits of the hip musculature and core endurance. In biomechanical studies, persons with PFPS have demonstrated excessive hip internal rotation and hip adduction as well as weak hip abductors, external rotators, and hip extensors compared with pain-free individuals.[2]
A 2018 sytematic review concluded that hip and knee strengthening is not only effective, but is also superior to knee strengthening alone for decreasing pain intensity and improving activity in people with patellofemoral pain.[3]
Physiotherapy[edit | edit source]
A 2018 systematic review confirmed that isolated hip strengthening and knee strengthening were equivalent for treatment of PFPS. However, hip strengthening alone has been proven to reduce pain and improve function in people with PFPS, and so has quadriceps strengthening alone.
The best option is to perform both quad hip strengthening exercises ie Strength training of the hip muscles, accompanied by strengthening of knee muscles, should be included in clinical management of individuals with patellofemoral pain in order to reduce pain and improve activity.[3]
Anatomy[edit | edit source]
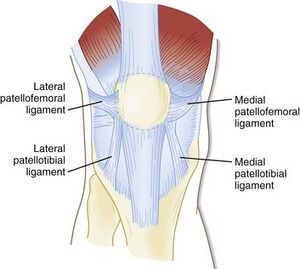
The patella is the largest sesamoid bone. It is located within the complex of the quadriceps and patellar tendon. Through its articulation with the femoral trochlea, the patellofemoral joint forms a highly complex unit with potential for joint instability. Patellofemoral joint stability is multifactorial and can be categorized into static and dynamic stabilizers.[4] See here for more information Patellofemoral Joint
Biomechanics[edit | edit source]
See Clinical Biomechanics of Patellofemoral Pain Syndrome
Strength of hip abductors and external rotators in PFPS[edit | edit source]
During ambulation hip abductors and external rotator muscle group act eccentrically to control the motion of hip adduction and hip internal rotation, respectively.[5]
Weakness in the abductors may allow for excessive femoral adduction and this, in turn, may lead to more abducted, or valgus, position of the knee. Knee valgus is believed to increase the lateral force acting on the patella.[6]
Weakness of the hip external rotators may allow for excessive femoral internal rotation and this may lead to increased contact pressure between the lateral femoral condyle and the lateral facet of the patella. [7]
Hip external rotators and abductors are also contributing in pelvic stability and leg alignment by eccentrically controlling femoral internal rotation and influencing hip adduction during weight bearing activities.[8][9]
Weakness of these muscles may increase medial femoral rotation, valgus knee moments, or cause a gluteus medius gait. These deviations may alter the adduction/abduction moments at the hip or lead to an increased Q-angle, which may subsequently alter tracking of the patella, increase compressive forces on the patellofemoral joint, and ultimately lead to knee pain.[7]
Theoretically, weakness of the abductors and external rotators may be associated with poor control of eccentric femoral adduction and internal rotation during weight-bearing activities, leading to misalignment of patellofemoral joint as the femur medially rotates underneath the patella.[10][7][5]
References[edit | edit source]
- ↑ Meira EP, Brumitt J. Influence of the hip on patients with patellofemoral pain syndrome: a systematic review. Sports health. 2011 Sep;3(5):455-65.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445210/(accessed 2.12.2021)
- ↑ 2.0 2.1 Na Y, Han C, Shi Y, Zhu Y, Ren Y, Liu W. Is Isolated Hip Strengthening or Traditional Knee-Based Strengthening More Effective in Patients With Patellofemoral Pain Syndrome? A Systematic Review With Meta-analysis. Orthopaedic Journal of Sports Medicine. 2021 Jul 28;9(7):23259671211017503.Available:https://journals.sagepub.com/doi/full/10.1177/23259671211017503 (accessed 2.12.2021)
- ↑ 3.0 3.1 Nascimento LR, Teixeira-Salmela LF, Souza RB, Resende RA. Hip and knee strengthening is more effective than knee strengthening alone for reducing pain and improving activity in individuals with patellofemoral pain: a systematic review with meta-analysis. journal of orthopaedic & sports physical therapy. 2018 Jan;48(1):19-31. Available:https://www.jospt.org/doi/10.2519/jospt.2018.7365 (accessed 2.12.2021)
- ↑ Rhee, S. J., Pavlou, G., Oakley, J., Barlow, D., & Haddad, F. Modern management of patellar instability. International Orthopaedics. 2012; Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3508055/pdf/264_2012_Article_1669.pdf (accessed 2.12.2021)
- ↑ 5.0 5.1 Maria Zulluga. Sports physiotherapy applied science and practice:churchil livingstone,587-611.
- ↑ David C, Reid: “Sports injury and assessment and rehabilitation”, Churchill Livingstone. 1992, pgs 345-398.
- ↑ 7.0 7.1 7.2 Robin EL. A rational approach to the treatment of patellofemoral pain. Clin Orthop 1979;144:107-109.
- ↑ Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med 2002;36:95-101.
- ↑ I.A. Kapanji. The physiology of joints. 5th ed;2,100-101.
- ↑ Insall J. Current Concepts Review: patellar pain. J Bone Joint Surg Am. 1982;64:147-152.