Tracheostomy: Difference between revisions
No edit summary |
No edit summary |
||
| (10 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Natalie Patterson |Natalie Patterson ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== '''Introduction''' == | |||
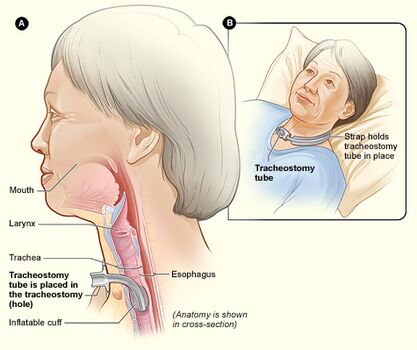
[[File:Tracheostomy NIH.jpeg|right|frameless|417x417px]] | |||
A tracheostomy is a [[Surgery and General Anaesthetic|surgical]] opening in the anterior wall of the [[Trachea and Larynx|trachea]]. Traditionally a tracheostomy is performed as an open surgical procedure, however safe and reliable percutaneous tracheostomy techniques have been developed, allowing for the bedside placement of a tracheostomy in many patients<ref>Raimonde AJ, Westhoven N, Winters R. Tracheostomy.Available:https://www.ncbi.nlm.nih.gov/books/NBK559124/ (accessed 18.5.2022)</ref>. | |||
This 6 minute video explains what a tracheotomy is. | |||
{{#ev:youtube|ULb5q6aBuic|300}} | |||
==== '''Percutaneous Tracheostomy''' ==== | ==== '''Percutaneous Tracheostomy''' ==== | ||
Percutaneous Tracheostomy involves Seldinger technique and dilatation of trachea between rings<ref name=":1">Life in the fast lane Available: https://litfl.com/percutaneous-tracheostomy/ (accessed 18.5.2022)</ref>. | |||
= | |||
A percutaneous tracheotomy (PT) is typically performed in a hospital room. The doctor makes a small incision near the base of the front of the neck. A special lens is fed through the mouth so that the surgeon can view the inside of the throat. Using this view of the throat, the surgeon guides a needle into the windpipe to create the tracheostomy hole, then expands it to the appropriate size for the tube<ref name=":2">Mayo clinic Tracheostomy Available: https://www.mayoclinic.org/tests-procedures/tracheostomy/about/pac-20384673<nowiki/>(accessed 18.5.2022)</ref>. Bedside PT generates significant cost savings by eliminating operating room and anesthesia charges. Bronchoscopy is commonly used as a visual aid during PT. Ultrasound (US)-guided PT is gaining popularity<ref>Al-Shathri Z, Susanto I. Percutaneous tracheostomy. InSeminars in Respiratory and Critical Care Medicine 2018 Dec (Vol. 39, No. 06, pp. 720-730). Thieme Medical Publishers.Available: https://pubmed.ncbi.nlm.nih.gov/30641590/<nowiki/>(accessed 18.5.2022)</ref>. | |||
==== '''Surgical Tracheostomy''' ==== | ==== '''Surgical Tracheostomy''' ==== | ||
Surgical Tracheostomy involves dissection and incision of trachea under direct vision<ref name=":1" />.[[File:Tracheostomy with tube.jpeg|thumb|Tracheostomy with tube]] | |||
Surgical tracheotomy can be performed in an operating room or in a hospital room. The person is positioned on there back, and a rolled-up towel (or equivalent) is placed under your shoulders to help stretch persons neck. Local anaesthetic is injected into the target area, and a skin incision (cut) is made. The surgeon will then open either the trachea (this is called a ‘tracheostomy’) or the cricothyroid membrane - the thinnest part of the airway below the larynx (this is called a ‘cricothyroidotomy’). The airway tube is inserted into the trachea and person is connected to the oxygen supply. The entire procedure is done as quickly as possible<ref name=":2" />. | |||
== Indications for a Tracheostomy<ref name=":0">NHS e-Learning for Healthcare and the Royal College of Anaesthetists. Understanding Tracheostomies and Laryngectomies. Available at https://cs1.e-learningforhealthcare.org.uk/content/NTSP_01_001/d/ELFH_Session/_/session.html#overview.html (accessed 23 May 2020)</ref> == | == Indications for a Tracheostomy<ref name=":0">NHS e-Learning for Healthcare and the Royal College of Anaesthetists. Understanding Tracheostomies and Laryngectomies. Available at https://cs1.e-learningforhealthcare.org.uk/content/NTSP_01_001/d/ELFH_Session/_/session.html#overview.html (accessed 23 May 2020)</ref> == | ||
| Line 55: | Line 29: | ||
* A tracheostomy is usually well tolerated and typically does not require sedation once it has been inserted. | * A tracheostomy is usually well tolerated and typically does not require sedation once it has been inserted. | ||
* It is the best way of invasively ventilating a patient in the medium to long term, it provides a secure airway without directly interfering with the larynx | * It is the best way of invasively ventilating a patient in the medium to long term, it provides a secure airway without directly interfering with the [[Trachea and Larynx|larynx]] | ||
* It can facilitate weaning from ventilation. | * It can facilitate [[Ventilation and Weaning|weaning from ventilation.]] | ||
* It can enable long-term mechanical ventilation of patients, either in an acute setting or long term. | * It can enable long-term mechanical ventilation of patients, either in an acute setting or long term. | ||
===== '''<nowiki/>Protecting the airway''' ===== | ===== '''<nowiki/>Protecting the airway''' ===== | ||
* Some patients are at high risk of aspirating secretions or gastric contents into the airway. E.g. neuromuscular disorders, head injuries, unconsciousness, stroke or following prolonged disuse such as after trans-laryngeal intubation (Endotracheal Tube) | * Some patients are at high risk of aspirating secretions or gastric contents into the airway. E.g[[Neuromuscular Disorders|. neuromuscular disorders]], [[Traumatic Brain Injury|head injuries]], unconsciousness, [[stroke]] or following prolonged disuse such as after trans-laryngeal intubation (Endotracheal Tube) | ||
* A tracheostomy tube with the cuff inflated reduces the risk and offers some protection against aspiration | * A tracheostomy tube with the cuff inflated reduces the risk and offers some protection against aspiration | ||
* Sub-glottic suction systems can help to reduce secretions that enter the airway | * Sub-glottic suction systems can help to reduce secretions that enter the airway | ||
| Line 68: | Line 42: | ||
* To facilitate the removal of bronchial secretions where there is poor cough effort with sputum retention | * To facilitate the removal of bronchial secretions where there is poor cough effort with sputum retention | ||
* Tracheostomy allows manual insufflation-exsufflation ([[Assisted Coughing|cough assist]]) to be applied directly to the lungs | * Tracheostomy allows manual insufflation-exsufflation ([[Assisted Coughing|cough assist]]) to be applied directly to the [[Lung Anatomy|lungs]] | ||
* Suction directly into the trachea to help clear secretions.<ref name=":0" /> | * Suction directly into the trachea to help clear secretions.<ref name=":0" /> | ||
===== Other Reasons for a Tracheostomy<ref>The Johns Hopkins University. Reasons for a tracheostomy. Available from https://www.hopkinsmedicine.org/tracheostomy/about/reasons.html<nowiki/>(accessed 26 May 2020)</ref> ===== | ===== Other Reasons for a Tracheostomy<ref>The Johns Hopkins University. Reasons for a tracheostomy. Available from https://www.hopkinsmedicine.org/tracheostomy/about/reasons.html<nowiki/>(accessed 26 May 2020)</ref> ===== | ||
* Neuromuscular diseases paralyzing or weakening chest muscles and diaphragm | * Neuromuscular diseases paralyzing or weakening chest muscles and [[Diaphragm Anatomy and Differential Diagnosis|diaphragm]] | ||
* Aspiration related to muscle or sensory problems in the throat | * Aspiration related to muscle or sensory problems in the throat | ||
* Fracture of cervical vertebrae with spinal cord injury | * Fracture of cervical vertebrae with [[Spinal Cord Injury|spinal cord injury]] | ||
* Long-term unconsciousness or coma | * Long-term unconsciousness or coma | ||
* Disorders of respiratory control such as congenital central hypoventilation or central apnea | * Disorders of respiratory control such as congenital central hypoventilation or central apnea | ||
* Facial surgery and facial burns | * Facial surgery and facial [[Burns Overview|burns]] | ||
* Anaphylaxis (severe allergic reaction) | * Anaphylaxis (severe allergic reaction) | ||
== Physiological Changes | == Physiological Changes == | ||
* The upper airway anatomical dead space can be reduced by up to 50%. - This space takes no part in gas exchange and adds to the work of breathing. Reducing this can help patients wean off a ventilator more easily. | * The upper airway anatomical dead space can be reduced by up to 50%. - This space takes no part in gas exchange and adds to the work of breathing. Reducing this can help patients wean off a ventilator more easily. | ||
* The natural warming, humidification and filtering of air that usually takes place in the upper airway is lost | * The natural warming, humidification and filtering of air that usually takes place in the upper airway is lost | ||
| Line 86: | Line 60: | ||
* The ability to swallow is adversely affected | * The ability to swallow is adversely affected | ||
* Sense of taste and smell can be lost which can have a negative impact on appetite. | * Sense of taste and smell can be lost which can have a negative impact on appetite. | ||
* Altered body image | * Altered body image<ref name=":0" /> | ||
== Complications == | == Complications == | ||
| Line 93: | Line 67: | ||
* Haemorrhage | * Haemorrhage | ||
* Misplacement of tube - within tissues around trachea or to main bronchus | * Misplacement of tube - within tissues around trachea or to main bronchus | ||
* Pneumothorax | * [[Pneumothorax]] | ||
* Tube occlusion | * Tube occlusion | ||
* Surgical emphysema | * Surgical emphysema | ||
| Line 102: | Line 76: | ||
* Partial or complete tube displacement | * Partial or complete tube displacement | ||
* Infection of the stoma site | * Infection of the stoma site | ||
* Infection of the bronchial tree (pneumonia) | * Infection of the bronchial tree ([[pneumonia]]) | ||
* Ulceration, and/or necrosis of trachea or mucosal ulceration by tube migration | * Ulceration, and/or necrosis of trachea or mucosal ulceration by tube migration | ||
* Risk of occlusion of the tracheostomy tube in obese or fatigued patients who have difficulty extending their neck | * Risk of occlusion of the tracheostomy tube in obese or fatigued patients who have difficulty extending their neck | ||
| Line 132: | Line 106: | ||
Patient may be able to eat and may be able to talk without a speaking valve. | Patient may be able to eat and may be able to talk without a speaking valve. | ||
{{#ev:youtube|KBbpxsznEPc|300}} | {{#ev:youtube|KBbpxsznEPc|300}}<ref>National Tracheostomy Safety Project. Understanding Tracheostomy Tubes (National Tracheostomy Safety Project). Available from https://www.youtube.com/watch?v=KBbpxsznEPc (Accessed May 31st 2020)</ref> | ||
=== '''Resources''' === | === '''Resources''' === | ||
| Line 143: | Line 117: | ||
[[Category:Respiratory]] | [[Category:Respiratory]] | ||
[[Category:Critical Care]] | [[Category:Critical Care]] | ||
[[Category:Interventions]] | |||
[[Category:Respiratory Disease - Interventions]] | |||
[[Category:Acute Care]] | |||
[[Category:Cardiopulmonary - Interventions]] | |||
[[Category:Cardiopulmonary]] | |||
Latest revision as of 03:04, 18 May 2022
Introduction[edit | edit source]
A tracheostomy is a surgical opening in the anterior wall of the trachea. Traditionally a tracheostomy is performed as an open surgical procedure, however safe and reliable percutaneous tracheostomy techniques have been developed, allowing for the bedside placement of a tracheostomy in many patients[1].
This 6 minute video explains what a tracheotomy is.
Percutaneous Tracheostomy[edit | edit source]
Percutaneous Tracheostomy involves Seldinger technique and dilatation of trachea between rings[2].
A percutaneous tracheotomy (PT) is typically performed in a hospital room. The doctor makes a small incision near the base of the front of the neck. A special lens is fed through the mouth so that the surgeon can view the inside of the throat. Using this view of the throat, the surgeon guides a needle into the windpipe to create the tracheostomy hole, then expands it to the appropriate size for the tube[3]. Bedside PT generates significant cost savings by eliminating operating room and anesthesia charges. Bronchoscopy is commonly used as a visual aid during PT. Ultrasound (US)-guided PT is gaining popularity[4].
Surgical Tracheostomy[edit | edit source]
Surgical Tracheostomy involves dissection and incision of trachea under direct vision[2].
Surgical tracheotomy can be performed in an operating room or in a hospital room. The person is positioned on there back, and a rolled-up towel (or equivalent) is placed under your shoulders to help stretch persons neck. Local anaesthetic is injected into the target area, and a skin incision (cut) is made. The surgeon will then open either the trachea (this is called a ‘tracheostomy’) or the cricothyroid membrane - the thinnest part of the airway below the larynx (this is called a ‘cricothyroidotomy’). The airway tube is inserted into the trachea and person is connected to the oxygen supply. The entire procedure is done as quickly as possible[3].
Indications for a Tracheostomy[5][edit | edit source]
Airway obstruction[edit | edit source]
- To secure and clear the airway in upper respiratory tract obstruction
- An obstruction, often caused by a cancer, swelling of the airway, infection, inflammation or trauma
- Where an airway is predicted to get worse and possibly become actually obstructed E.g. after major head and neck surgery
Providing an artificial airway for ventilation[edit | edit source]
- A tracheostomy is usually well tolerated and typically does not require sedation once it has been inserted.
- It is the best way of invasively ventilating a patient in the medium to long term, it provides a secure airway without directly interfering with the larynx
- It can facilitate weaning from ventilation.
- It can enable long-term mechanical ventilation of patients, either in an acute setting or long term.
Protecting the airway[edit | edit source]
- Some patients are at high risk of aspirating secretions or gastric contents into the airway. E.g. neuromuscular disorders, head injuries, unconsciousness, stroke or following prolonged disuse such as after trans-laryngeal intubation (Endotracheal Tube)
- A tracheostomy tube with the cuff inflated reduces the risk and offers some protection against aspiration
- Sub-glottic suction systems can help to reduce secretions that enter the airway
Respiratory secretion management[edit | edit source]
- To facilitate the removal of bronchial secretions where there is poor cough effort with sputum retention
- Tracheostomy allows manual insufflation-exsufflation (cough assist) to be applied directly to the lungs
- Suction directly into the trachea to help clear secretions.[5]
Other Reasons for a Tracheostomy[6][edit | edit source]
- Neuromuscular diseases paralyzing or weakening chest muscles and diaphragm
- Aspiration related to muscle or sensory problems in the throat
- Fracture of cervical vertebrae with spinal cord injury
- Long-term unconsciousness or coma
- Disorders of respiratory control such as congenital central hypoventilation or central apnea
- Facial surgery and facial burns
- Anaphylaxis (severe allergic reaction)
Physiological Changes[edit | edit source]
- The upper airway anatomical dead space can be reduced by up to 50%. - This space takes no part in gas exchange and adds to the work of breathing. Reducing this can help patients wean off a ventilator more easily.
- The natural warming, humidification and filtering of air that usually takes place in the upper airway is lost
- The patient's ability to speak is removed/reduced as the cuff impairs the swallowing mechanisms of the larynx
- The ability to swallow is adversely affected
- Sense of taste and smell can be lost which can have a negative impact on appetite.
- Altered body image[5]
Complications[edit | edit source]
Perioperative period[edit | edit source]
- Haemorrhage
- Misplacement of tube - within tissues around trachea or to main bronchus
- Pneumothorax
- Tube occlusion
- Surgical emphysema
- Loss of the upper airway
Postoperative period < 7 days[edit | edit source]
- Tube blockage with secretions or blood
- Partial or complete tube displacement
- Infection of the stoma site
- Infection of the bronchial tree (pneumonia)
- Ulceration, and/or necrosis of trachea or mucosal ulceration by tube migration
- Risk of occlusion of the tracheostomy tube in obese or fatigued patients who have difficulty extending their neck
- Tracheo-oesophageal fistula formation
- Haemorrhage
Late postoperative period >7 days[edit | edit source]
- Granulomata (a mass of granulation tissue) of the trachea may cause respiratory difficulty when the tracheostomy tube is removed
- Tracheal dilation, stenosis or tracheomalacia (trachea partly collapses especially during increased airflow)
- Scar formation-requiring revision
- Haemorrhage
Types of Tubes[edit | edit source]
Cuffed with fenestrated tubes[edit | edit source]
Used for patients who are on the ventilator but are not able to tolerate a speaking valve to speak
Cuffed with unfenestrated tubes[edit | edit source]
Used to obtain a closed circuit for ventilation
Uncuffed with fenestrated tubes[edit | edit source]
Used for patients who have difficulty using a speaking valve
Uncuffed with unfenestrated tubes[edit | edit source]
Used for patients with tracheal problems
Used for patients who are ready for decannulation
Patient may be able to eat and may be able to talk without a speaking valve.
Resources[edit | edit source]
UK National Tracheostomy Safety Project http://www.tracheostomy.org.uk/
Watch a Tracheostomy https://www.hopkinsmedicine.org/tracheostomy/video/watching.html
References[edit | edit source]
- ↑ Raimonde AJ, Westhoven N, Winters R. Tracheostomy.Available:https://www.ncbi.nlm.nih.gov/books/NBK559124/ (accessed 18.5.2022)
- ↑ 2.0 2.1 Life in the fast lane Available: https://litfl.com/percutaneous-tracheostomy/ (accessed 18.5.2022)
- ↑ 3.0 3.1 Mayo clinic Tracheostomy Available: https://www.mayoclinic.org/tests-procedures/tracheostomy/about/pac-20384673(accessed 18.5.2022)
- ↑ Al-Shathri Z, Susanto I. Percutaneous tracheostomy. InSeminars in Respiratory and Critical Care Medicine 2018 Dec (Vol. 39, No. 06, pp. 720-730). Thieme Medical Publishers.Available: https://pubmed.ncbi.nlm.nih.gov/30641590/(accessed 18.5.2022)
- ↑ 5.0 5.1 5.2 NHS e-Learning for Healthcare and the Royal College of Anaesthetists. Understanding Tracheostomies and Laryngectomies. Available at https://cs1.e-learningforhealthcare.org.uk/content/NTSP_01_001/d/ELFH_Session/_/session.html#overview.html (accessed 23 May 2020)
- ↑ The Johns Hopkins University. Reasons for a tracheostomy. Available from https://www.hopkinsmedicine.org/tracheostomy/about/reasons.html(accessed 26 May 2020)
- ↑ National Tracheostomy Safety Project. Understanding Tracheostomy Tubes (National Tracheostomy Safety Project). Available from https://www.youtube.com/watch?v=KBbpxsznEPc (Accessed May 31st 2020)