Lower Extremity Functional Scale (LEFS): Difference between revisions
mNo edit summary |
Nehal Shah (talk | contribs) m (Added validity of LEFS) |
||
| (48 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- Emily Hanson | '''Original Editor ''' - [[User:Emily Hanson|Emily Hanson]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | ||
</div> | </div> | ||
The | == '''Background''' == | ||
The lower extremity functional scale (LEFS) is a valid patient-rated outcome measure (PROM) for the measurement of lower extremity function. It was first developed by Binkley et al. (1999) in a group of patients with various musculoskeletal conditions<ref name="Binkley et al." /> like THR, TKR, OA of Hip etc. The scale is originally developed in English language and according to western culture. | |||
The scale consist of 4 groups with 20 questions. The questions in these group focus on activities with increasing physical demands like questions from walking between rooms to running on uneven ground<ref>Backes M, Dingemans SA, Schep NW, Bloemers FW, Van Dijkman B, Garssen FP, Haverlag R, Hoogendoorn JM, Joosse P, Mirck B, Postma V. Wound Infections Following Implant removal below the knee: the effect of antibiotic prophylaxis; the WIFI-trial, a multi-centre randomized controlled trial. BMC surgery. 2015 Dec;15:1-6.</ref>. The scoring of this scale varies from 0 (extreme difficulty/unable to perform activity) to 4 (no difficulty). The total score can be obtained by summing the scores of the individual items. The maximum score of 80 indicates no functional limitations and the minimum score of 0 indicates extreme limitations. | |||
Studies have shown that LEFS is a reliable tool in clinical practice to assess impact of the conditions on lower extremity functions<ref>Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA. Measurement properties of the lower extremity functional scale: a systematic review. journal of orthopaedic & sports physical therapy. 2016 Mar;46(3):200-16.</ref> | |||
== | == Purpose == | ||
In patients undergoing Orthopedic /trauma surgery, due to pre-existing conditions, at times it becomes difficult to assess pre-disease physical function. This is because questionnaires pertaining to pre-disorder physical functions are affected by recall bias. This poses a challenge for the physicians to measure the treatment effects. If Normative data of PROMs are available, they pose as reference data for healthy population<ref>Aasheim T, Finsen V. The DASH and the QuickDASH instruments. Normative values in the general population in Norway. Journal of Hand Surgery (European Volume). 2014 Feb;39(2):140-4.</ref> | |||
The purpose of taking Lower Extremity Functional Scale (LEFS) is to measure "patients' initial function, ongoing progress, and outcome" for a wide range of lower-extremity conditions.<ref name="Binkley et al.">Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther 1999;79:371-383.</ref>Taking the scale at regular intervals will enable to objectively document patient progress throughout the course of treatment.<br> | |||
[[File:Lower Extremity Functional Scale.png|frameless|581x581px|right]] | |||
== Intended Population == | |||
The LEFS is | The LEFS is intended for use with adults, with lower extremity conditions like Hip OA, THR, TKR, Trauma surgery for lower extremity etc.<ref name="Binkley et al." /> | ||
== Method of Use == | |||
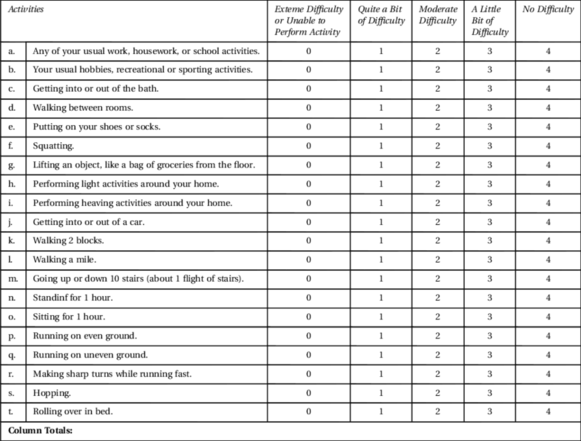
The LEFS is a self-report questionnaire. Patients answer the question "Today, <u>do you</u> or <u>would you</u> have any difficulty at all with:" in regards to twenty different everyday activities.<ref name="Binkley et al." /> | |||
Patients select an answer from the following scale for each activity listed: | |||
#Extreme Difficulty or Unable to Perform Activity | |||
#Quite a Bit of Difficulty | #Quite a Bit of Difficulty | ||
#Moderate Difficulty | #Moderate Difficulty | ||
| Line 27: | Line 34: | ||
#No Difficulty | #No Difficulty | ||
The patient's score is tallied at the bottom of the page. The maximum possible score is 80 points, indicating very high function. The minimum possible score is 0 points, indicating very low function. | The patient's score is tallied at the bottom of the page. The maximum possible score is 80 points, indicating very high function. The minimum possible score is 0 points, indicating very low function. | ||
{{#ev:youtube|4CDhRMZCWQ4}}<br> | |||
== Evidence == | == Evidence == | ||
| Line 37: | Line 42: | ||
=== Reliability === | === Reliability === | ||
Internal reliability for the LEFS is excellent (α=0.96). Test-retest reliability estimates were R=.86 (95% lower limit CI=.80) for the entire sample (n=98) and R=.94 (95% lower limit CI=.89) for the subset of patients with more chronic conditions (n=31).<ref name="Binkley et al." />< | Internal reliability for the LEFS is excellent (α=0.96). Test-retest reliability estimates were R=.86 (95% lower limit CI=.80) for the entire sample (n=98) and R=.94 (95% lower limit CI=.89) for the subset of patients with more chronic conditions (n=31).<ref name="Binkley et al." /> | ||
Reliability of LEFS score with reassessment period of less than or equal to seven days was found to be ICC= 0.86, less than or equal to three weeks was found to be ICC = 0.87 and over longer reassessment periods of 2 to 12 months was found to be ICC = 0.75<ref>Hoogeboom TJ, de Bie RA, den Broeder AA, van den Ende CH. The Dutch Lower Extremity Functional Scale was highly reliable, valid and responsive in individuals with hip/knee osteoarthritis: a validation study. BMC musculoskeletal disorders. 2012 Dec;13:1-0.</ref><ref name=":0">Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA. Measurement properties of the lower extremity functional scale: a systematic review. journal of orthopaedic & sports physical therapy. 2016 Mar;46(3):200-16.</ref>in patients with Anterior Cruciate Ligament reconstruction and knee Osteoarthritis<ref name=":0" /> | |||
=== Validity === | === Validity === | ||
The LEFS is a valid tool as compared to the SF-36.<ref name="Binkley et al." />< | The LEFS is a valid tool as compared to the SF-36.<ref name="Binkley et al." />Studies have suggested low or marginal floor effect in the content validity<ref name=":0" /> | ||
LEFS have shown moderate to high concordance with Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) in individuals with THR and TKR<ref>Stratford PW, Kennedy DM, Hanna SE. Condition-specific Western Ontario McMaster Osteoarthritis Index was not superior to region-specific Lower Extremity Functional Scale at detecting change. Journal of Clinical Epidemiology. 2004 Oct 1;57(10):1025-32.</ref>. It has also shown high correlations with most subscales of His disability and Osteoarthritis Outcome Score and the region specific or joint specific measures<ref name=":0" />, moderate correlation with Knee injury and Osteoarthritis Outcome Score, visual analog scale for pain in patients with knee disorders and low back pain<ref name=":0" /> | |||
=== Responsiveness === | === Responsiveness === | ||
| Line 49: | Line 59: | ||
The minimum clinically important difference (MCID) for the LEFS is 9 points. That is, "Clinicians can be reasonably confident that a change of greater than 9 points is... a clinically meaningful functional change."<ref name="Binkley et al." /><br> | The minimum clinically important difference (MCID) for the LEFS is 9 points. That is, "Clinicians can be reasonably confident that a change of greater than 9 points is... a clinically meaningful functional change."<ref name="Binkley et al." /><br> | ||
The capacity of the LEFS to detect change in lower-extremity function appears to be superior to that of the SF-36 physical function subscale, as indicated by higher correlations with an external prognostic rating of change.<ref name="Binkley et al." / | The capacity of the LEFS to detect change in lower-extremity function appears to be superior to that of the SF-36 physical function subscale, as indicated by higher correlations with an external prognostic rating of change.<ref name="Binkley et al." /> | ||
=== Miscellaneous | The LEFS has good measurement properties--namely test-retest reliability and cross-sectional construct validity--and it could be an alternative to WOMAC-PF. <ref>Pua YH, Cowan SM, Wrigley TV, Bennell KL. [https://pubmed.ncbi.nlm.nih.gov/19282145/ The lower extremity functional scale could be an alternative to the Western Ontario and McMaster universities osteoarthritis index physical function scale.] Journal of clinical epidemiology. 2009 Oct 1;62(10):1103-11.</ref> | ||
=== Miscellaneous === | |||
The LEFS has an error of +/- 5 points. That is, the tabulated score is within 5 points of a patient's "true" score.<ref name="Binkley et al." /><br> | The LEFS has an error of +/- 5 points. That is, the tabulated score is within 5 points of a patient's "true" score.<ref name="Binkley et al." /><br> | ||
== Adaptation in different countries == | |||
LEFS has been translated and adapted in different populations like, Italian, Canadian French, Dutch, Arabic, Brazilian Portugese, Malaysian, Finnish, Persian, Turkish, Taiwan, Chinese and Dutch translated and adapted version are also tested for validity and reliability. | |||
== | == Resources == | ||
[https://www.sralab.org/rehabilitation-measures/lower-extremity-functional-scale Lower Extremity Functional Scale] | |||
== References == | == References == | ||
<references /> | <references responsive="0" /> | ||
[[Category:Outcome Measures]] | |||
[[Category: | [[Category:Hip - Outcome Measures]] | ||
[[Category:Knee - Outcome Measures]] | |||
[[Category:Ankle - Outcome Measures]] | |||
[[Category:Foot - Outcome Measures]] | |||
[[Category:Hip]] | |||
[[Category:Knee]] | |||
[[Category:Ankle]] | |||
[[Category:Foot]] | |||
[[Category:Lumbar Spine - Outcome Measures]] | |||
Latest revision as of 13:56, 28 June 2024
Original Editor - Emily Hanson
Top Contributors - Emily Hanson, Naomi O'Reilly, Kim Jackson, Evan Thomas, Nehal Shah, Admin, Vidya Acharya, Lucinda hampton, Disha Rupareliya, WikiSysop, Mandeepa Kumawat, Shaimaa Eldib and Rishika Babburu
Background[edit | edit source]
The lower extremity functional scale (LEFS) is a valid patient-rated outcome measure (PROM) for the measurement of lower extremity function. It was first developed by Binkley et al. (1999) in a group of patients with various musculoskeletal conditions[1] like THR, TKR, OA of Hip etc. The scale is originally developed in English language and according to western culture.
The scale consist of 4 groups with 20 questions. The questions in these group focus on activities with increasing physical demands like questions from walking between rooms to running on uneven ground[2]. The scoring of this scale varies from 0 (extreme difficulty/unable to perform activity) to 4 (no difficulty). The total score can be obtained by summing the scores of the individual items. The maximum score of 80 indicates no functional limitations and the minimum score of 0 indicates extreme limitations.
Studies have shown that LEFS is a reliable tool in clinical practice to assess impact of the conditions on lower extremity functions[3]
Purpose[edit | edit source]
In patients undergoing Orthopedic /trauma surgery, due to pre-existing conditions, at times it becomes difficult to assess pre-disease physical function. This is because questionnaires pertaining to pre-disorder physical functions are affected by recall bias. This poses a challenge for the physicians to measure the treatment effects. If Normative data of PROMs are available, they pose as reference data for healthy population[4]
The purpose of taking Lower Extremity Functional Scale (LEFS) is to measure "patients' initial function, ongoing progress, and outcome" for a wide range of lower-extremity conditions.[1]Taking the scale at regular intervals will enable to objectively document patient progress throughout the course of treatment.
Intended Population[edit | edit source]
The LEFS is intended for use with adults, with lower extremity conditions like Hip OA, THR, TKR, Trauma surgery for lower extremity etc.[1]
Method of Use[edit | edit source]
The LEFS is a self-report questionnaire. Patients answer the question "Today, do you or would you have any difficulty at all with:" in regards to twenty different everyday activities.[1]
Patients select an answer from the following scale for each activity listed:
- Extreme Difficulty or Unable to Perform Activity
- Quite a Bit of Difficulty
- Moderate Difficulty
- A Little Bit of Difficulty
- No Difficulty
The patient's score is tallied at the bottom of the page. The maximum possible score is 80 points, indicating very high function. The minimum possible score is 0 points, indicating very low function.
Evidence[edit | edit source]
Reliability[edit | edit source]
Internal reliability for the LEFS is excellent (α=0.96). Test-retest reliability estimates were R=.86 (95% lower limit CI=.80) for the entire sample (n=98) and R=.94 (95% lower limit CI=.89) for the subset of patients with more chronic conditions (n=31).[1]
Reliability of LEFS score with reassessment period of less than or equal to seven days was found to be ICC= 0.86, less than or equal to three weeks was found to be ICC = 0.87 and over longer reassessment periods of 2 to 12 months was found to be ICC = 0.75[5][6]in patients with Anterior Cruciate Ligament reconstruction and knee Osteoarthritis[6]
Validity[edit | edit source]
The LEFS is a valid tool as compared to the SF-36.[1]Studies have suggested low or marginal floor effect in the content validity[6]
LEFS have shown moderate to high concordance with Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) in individuals with THR and TKR[7]. It has also shown high correlations with most subscales of His disability and Osteoarthritis Outcome Score and the region specific or joint specific measures[6], moderate correlation with Knee injury and Osteoarthritis Outcome Score, visual analog scale for pain in patients with knee disorders and low back pain[6]
Responsiveness[edit | edit source]
The minimum detectable change (MDC) for the LEFS is 9 points. That is, a change of more than 9 points represents a true change in the patient's condition.[1]
The minimum clinically important difference (MCID) for the LEFS is 9 points. That is, "Clinicians can be reasonably confident that a change of greater than 9 points is... a clinically meaningful functional change."[1]
The capacity of the LEFS to detect change in lower-extremity function appears to be superior to that of the SF-36 physical function subscale, as indicated by higher correlations with an external prognostic rating of change.[1]
The LEFS has good measurement properties--namely test-retest reliability and cross-sectional construct validity--and it could be an alternative to WOMAC-PF. [8]
Miscellaneous[edit | edit source]
The LEFS has an error of +/- 5 points. That is, the tabulated score is within 5 points of a patient's "true" score.[1]
Adaptation in different countries[edit | edit source]
LEFS has been translated and adapted in different populations like, Italian, Canadian French, Dutch, Arabic, Brazilian Portugese, Malaysian, Finnish, Persian, Turkish, Taiwan, Chinese and Dutch translated and adapted version are also tested for validity and reliability.
Resources[edit | edit source]
Lower Extremity Functional Scale
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther 1999;79:371-383.
- ↑ Backes M, Dingemans SA, Schep NW, Bloemers FW, Van Dijkman B, Garssen FP, Haverlag R, Hoogendoorn JM, Joosse P, Mirck B, Postma V. Wound Infections Following Implant removal below the knee: the effect of antibiotic prophylaxis; the WIFI-trial, a multi-centre randomized controlled trial. BMC surgery. 2015 Dec;15:1-6.
- ↑ Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA. Measurement properties of the lower extremity functional scale: a systematic review. journal of orthopaedic & sports physical therapy. 2016 Mar;46(3):200-16.
- ↑ Aasheim T, Finsen V. The DASH and the QuickDASH instruments. Normative values in the general population in Norway. Journal of Hand Surgery (European Volume). 2014 Feb;39(2):140-4.
- ↑ Hoogeboom TJ, de Bie RA, den Broeder AA, van den Ende CH. The Dutch Lower Extremity Functional Scale was highly reliable, valid and responsive in individuals with hip/knee osteoarthritis: a validation study. BMC musculoskeletal disorders. 2012 Dec;13:1-0.
- ↑ 6.0 6.1 6.2 6.3 6.4 Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA. Measurement properties of the lower extremity functional scale: a systematic review. journal of orthopaedic & sports physical therapy. 2016 Mar;46(3):200-16.
- ↑ Stratford PW, Kennedy DM, Hanna SE. Condition-specific Western Ontario McMaster Osteoarthritis Index was not superior to region-specific Lower Extremity Functional Scale at detecting change. Journal of Clinical Epidemiology. 2004 Oct 1;57(10):1025-32.
- ↑ Pua YH, Cowan SM, Wrigley TV, Bennell KL. The lower extremity functional scale could be an alternative to the Western Ontario and McMaster universities osteoarthritis index physical function scale. Journal of clinical epidemiology. 2009 Oct 1;62(10):1103-11.