Gastroesophageal Reflux Disease: Difference between revisions
No edit summary |
No edit summary |
||
| Line 147: | Line 147: | ||
It is essential for the physical therapist to take note of the patient's medications; listen for complaints of headache, constipation, diarrhea, abdominal pain and dizziness; and report those findings to the doctor. | It is essential for the physical therapist to take note of the patient's medications; listen for complaints of headache, constipation, diarrhea, abdominal pain and dizziness; and report those findings to the doctor. | ||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values<ref name="PUB med" /> == | ||
Diagnostic tests are not typically needed unless the symptoms are severe. Physicians will order diagnostic tests to diagnose GERD or other complications if there are severe symptoms, the symptoms are not relieved with medications or the symptoms returned.<br> | |||
Diagnostic tests used to diagnose GERD: | |||
*Esophagogastroduodenoscopy | |||
*Barium swallow | |||
*Continuous esophageal pH mointoring | |||
*Esophageal manometry | |||
== Etiology/Causes == | == Etiology/Causes == | ||
Revision as of 15:20, 20 April 2011
Original Editors - Tessa Puckett from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Gastroesophageal reflux disease (GERD), sometimes referred to as esophagitis, is a condition that results from reflux (backward flow) of the stomach contents into the esophagus. Reflux of infectious agents, chemical irritants, physical agents such as radiation and nasogastric intubation can cause GERD and can irritate and inflame the esophagus causing heartburn, belching, sore throat and other symptoms. Heartburn and indigestion are not other words for GERD, but are common symptoms of the condition. [1][2][3]
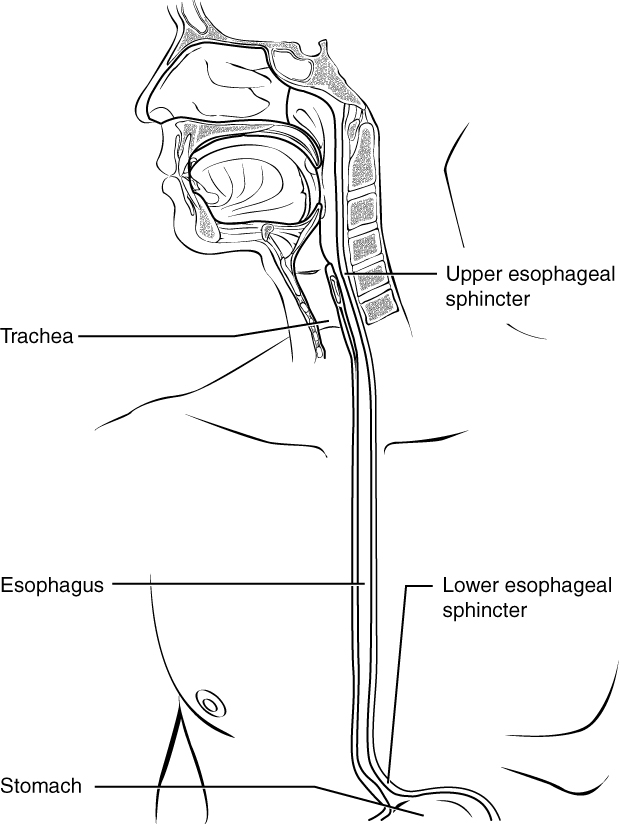
[Photo courtesy of the National Center for Biotechnology Information, U.S. National Library of Medicine. Available at http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001311/figure/d19e2114/?report=objectonly.]
Prevalence[edit | edit source]
add text here
Characteristics/Clinical Presentation[3][2][edit | edit source]
Pain in the lower substernal are can arise as a result of relfux or GERD; it is commonly described as "heartburn" or "indigestion". GERD is also described as gripping, squeezing or burning sensations in the substernal area.
Onset of GERD can occur when lying flat on the back, after meals, or bending forward and is usually worse at night. It is important to note that reflux or GERD is often confused with angina or a heart attack and should be reported to the doctor. GERD is not typically exercise induced and is relieved with antacids; this can help differentiate between angina/heart attack and reflux.
Chest pain referred from the upper gastrointestinal tract can radiate from the chest posteriorly to the upper back or interscapular or subscapular regions from vertebrae T10 - L2.
Common Symptoms:
- Heartburn
- Bitter/sour taste in the back of the throat
- Abdominal bloating/Abdominal discomfort
- Gas
- Chronic Cough
- Feeling the food is trapped behind the breastbone or in the throat
- Nausea after eating
- Burning sensation that begins at the xiphoid processs and radiates up toward the neck
- Intense sharp pain behind sternum with radiation to the back
Less Common Symptoms:
- Difficulty swallowing (dysphagia)
- Hiccups
- Hoarseness or change in voice
- Sore throat
Associated Co-morbidities[edit | edit source]
Patients with a past medical history of alcoholism, cirrhosis of the liver, peptic ulcers, esophageal varices, esophageal cancer, and long term use of NSAID's are more likely to have symptoms of GERD and should have diagnostic tests performed to rule out more severe conditions or diagnose GERD. [2]
Medications[2][edit | edit source]
Medications used to treat symptoms of GERD include: Antacids, Histamine 2 Receptor Blockers, and Proton Pump Inhibitors.
Antacids
- Neutralizes the acid
- Does not reduce it (same amount of acid is produced)
- Available over the counter, do not require a prescription
- Includes Mylanta, Maalox, Tums, Rolaids
File:Mylanta.jpg File:Tums.jpg File:Rolaids enlarge1.jpg
Histamine-2 Receptor Blockers
- Reduce stomach acid produced by the stomach
- Some are sold over the counter
- Over the Counter H2 Blockers: Pepcid, Zantac, Tagamet, and Axid
File:Pepcid.jpg File:Zantac.jpg
Proton Pump Inihibitors
- Most potent acid-suppressing agent
- Stops acid from forming, instead of neutralizing it
- Some PPI's are sold over the counter
- Use caution when used without medial supervision
- PPI's can mask more serious conditions in the esophagus and stomach
- Over the counter PPI's: Prilosec (omeprazole) and Zegerid
- PPI's requiring a prescription: Prevacid, Protonix, Nexium (esomperalzole), and Aciphex
File:Prilosec.jpg File:Nexium.jpg File:Zegerid-rebate.jpg
People taking the above listed medications should report to the doctor if they have complaints of headache, constipation, diarrhea, abdominal pain, or dizziness.
It is essential for the physical therapist to take note of the patient's medications; listen for complaints of headache, constipation, diarrhea, abdominal pain and dizziness; and report those findings to the doctor.
Diagnostic Tests/Lab Tests/Lab Values[3][edit | edit source]
Diagnostic tests are not typically needed unless the symptoms are severe. Physicians will order diagnostic tests to diagnose GERD or other complications if there are severe symptoms, the symptoms are not relieved with medications or the symptoms returned.
Diagnostic tests used to diagnose GERD:
- Esophagogastroduodenoscopy
- Barium swallow
- Continuous esophageal pH mointoring
- Esophageal manometry
Etiology/Causes[edit | edit source]
- Lower Esophageal Sphincter (LES) Dysfunction
The LES is a ring of muscle fibers that functions to close the opening between the esophagus and the stomach. When the LES is not functioning properly, the stomach contents (food, liquid, and stomach acid) can move backward into the esophagus causing damage to the esophagus. The backward flow of food from the stomach into the esphophagus is called reflux. [3]
[Photo courtesy of the National Center for Biotechnology Information, U.S. National Library of Medicine. Available at http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001311/figure/A000265.B19609/?report=objectonly]
- Medications [3]
Several medications can cause GERD or make it worse
Medication Class: Example Medication
Nonsteroidal anti-inflammatory drugs (NSAID's): Advil (ibruprofen), Motrin, Aleve
Anticholinergics: Bentyl
Beta Blockers: Toprol XL
Bronchodilators: Advair
Calcium Channel Blockers: Norvasc
Hormone Replacement Therapy: Progesterone
Sedatives (benzodiazepines): Valium, Xanax
Tricyclic Antidepressants: Doxepin
- Obesity
- Smoking
- Alcohol
Systemic Involvement[edit | edit source]
Musculoskeletal:
Untreated ulcers can cause biomechanical changes in muscular contractions and spinal movement. Patient may present with musculoskeletal deficits or dysfunctions because of the untreated ulcer. It is important for the physical therapist to take a good medical history to reveal actual cause of musculoskeletal dysfunction. Patients may think that heartburn while lying flat, difficulty swallowing, or chronic cough is unrelated to their recent onset of midscapular pain or thoracic back pain; thus, it is imperative to ask the patient if they have had any symptoms of GERD and if they are being treated by a medical doctor for the diagnosis.[2]
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
Shakers Head Lift Exercise PDF Handout from The Ohio State University Medical Center Department of Rehabilitation Services - Dodd Hall[4]
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports/ Case Studies[edit | edit source]
Chronic gastroesophageal reflux disease and its effect on laryngeal visualization and intubation: a case report. [5]
A Randomized Study Comparing the Shaker Exercise with Traditional Therapy: A Preliminary Study [6]
Resources
[edit | edit source]
National Institue of Health MedlinePlus: http://www.nlm.nih.gov/medlineplus
National Digestive Disease Information Clearinghouse:http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/
eMedicine Health: http://www.emedicinehealth.com
International Foundation for Functional Gastrointestinal Disorders: http://www.aboutgerd.org/
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1PW-O5V9EIraHx6Utb0JkY5qObdTZAlZCEHZnz9rPDhn_kksht|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier; 2009.
- ↑ 2.0 2.1 2.2 2.3 2.4 Goodman, Snyder. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th Ed. Philadelphia: WB Saunders; 2003.
- ↑ 3.0 3.1 3.2 3.3 3.4 National Center for Biotechnology Information, U.S. National Library of Medicine. Gastroesophageal reflux disease. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001311/ (accessed 17 March 2011).
- ↑ The Ohio State University Medical Center Department of Rehabilitation Services - Dodd Hall. Exercises to Improve Swallowing. http://medicalcenter.osu.edu/PatientEd/Materials/PDFDocs/dis-cond/general/exercises-swallowing.pdf (accessed 31 March 2011).
- ↑ Stevens L. Chronic gastroesophageal reflux disease and its effect on laryngeal visualization and intubation: a case report. AANA Journal [serial on the Internet. (2002, Oct), [cited March 17, 2011]; 70(5): 373-375. Available from: MEDLINE.]
- ↑ Logemann, JA, Rademaker, A, Pauloski, BR, et al. A Randomized Study Comparing the Shaker Exercise with Traditional Therapy: A Preliminary Study. Dysphagia. [serial on the Internet. (2009 December), [cited March 31, 2011]; 24(4): 403–411. Available from: PubMed.]