Menarche to Menopause
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Wanda van Niekerk and Ewa Jaraczewska
Introduction[edit | edit source]
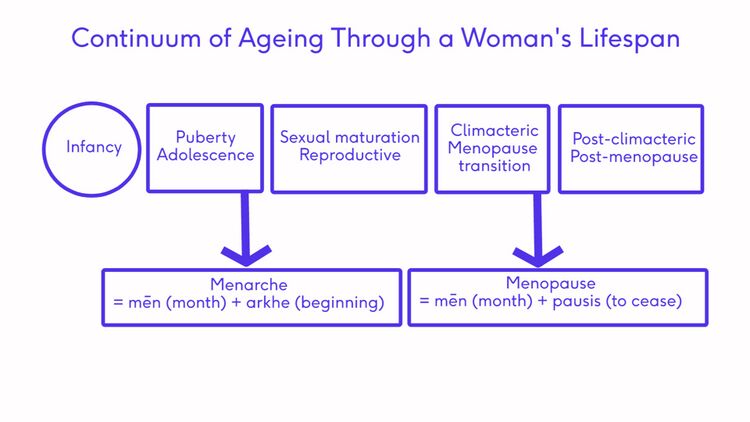
A female will spend approximately 12% of her life from birth to menarche, approximately 40% after menarche and through her reproductive years and approximately 40% from menopause through her post-menopausal years. Pregnancy and the postpartum can take from 12 to 24 months, for a complicated case, which works out to possibly 2% of her life. Women spend a great deal of time preparing for and understanding pregnancy and birth, but don't seem to apply the same understanding and consideration to the other aspects of their health, that includes menarche and menopause. We should be focusing understanding on these transitions in life and preparing adequately for them.
Complex Female Developmental Process[edit | edit source]
The above illustration shows the transitions a female will pass through in an average life span. The onset of these transitions can be estimated by looking at common signs and symptoms.
Diagnosis of Stages[edit | edit source]
The transitional stages are made by a functional diagnosis looking at the signs and symptoms. The aim of making a diagnosis as to the stage is to offer the person support, care and education. Not all women pass through the stages in life in a completely linear process. The might move back and forth between stages or even skip a stage. This is not always indicative of a problem or that the women is not healthy. All it shows is that these stages and transitions are to be understood by the individual so they can care for themselves appropriately at the phase they are currently in.
Common considerations[edit | edit source]
- Age of Female
- Younger (8-16 yrs) for menarche transition
- Older (45-54 yrs) for menopause transition
- Character of Menses
- Regularity
- Duration
- Flow heaviness
- Physical changes
- Breast budding
- Growth spurt
- Low energy/fatigue
- Acne, bloating
- Fluid retention
- Mental changes
- Moodiness
- Short temperedness
- Difficulty concentrating
Puberty[edit | edit source]
Puberty is the transitional stage that leads up to menarche. Regular monitoring[1] using a Health Client Check should be conducted during this phase, with regular educational conversations from the age of approximately 6 years old.
During this phase, fertility cannot be assumed as there is no definitive point at which eggs become viable. This knowledge could only be assumed after the onset of menarche. The education regarding contraception is essential to the health of a female in this transitional time.
Puberty happens to everyone within the ages of 6-16 yrs, but menarche is unique to females occurring approximately 2 years after the onset of secondary sex characteristic changes (specifically breast budding), at the approximate age of 12.4 years. This age has been decreasing presumably due to nutrition and lifestyle changes but further research is required on tis topic.
HPG Axis[edit | edit source]
The structures involved in this stage are the HPG Axis and the adrenal glands. The HPG axis consists of the hypothalamus, pituitary gland and the ovaries. A pulsing release of gonadotropin-releasing hormone stimulates the pituitary gland to release two important hormones: Luteinising hormone (LH), and Follicle-stimulating hormone (FSH). This initiates the production of oestrogen, which is needed to stimulate the secondary sexual characteristics along, with the adrenals. Adrenal gland maturation is an independent but interrelated process. Other hormones are also involved before puberty to mature the eggs in the ovaries and become key to maintaining the cyclic reproductive function.
Health Client Check:[edit | edit source]
The onset of puberty for a female should be identified and monitored for evidence of supporting good health or to identify disease processes that may require treatment. Regular health visit monitoring should include a visual exam of external primary sex characteristics including the external genitalia. When a female is sexually active, an examination of the internal primary sex characteristics should be advised. A Health Client Check also entails a height and weight measurement with the identification of the appearance of any secondary sex characteristics. These basic markers should be reviewed at each health visit.
- Visual exam for external primary sex characteristics
- Height/Weight
- Identification of appearance of secondary sex characteristics
- Prepubertal genital exam by a doctor
Sexual Maturity Rating (SMR) - Tanner Stages[edit | edit source]
Sexual Maturity Rating, SMR, better known as Tanner Stages, is an objective classification system that providers use to document and track the development and sequence of secondary sex characteristics of children during puberty. In females, the most important characteristics are breast development and pubic hair growth. There are other characteristics that are noteworthy, those being a rounded or hourglass figure, increased hip girth, an increased body fat composition, and comparatively to our male counterparts, a slower ability to generate muscle mass and less upper body strength.
Approximately 2 to 2.5 years after a female is Tanner stage 2, a female will start to have her period. This is known as menarche, and when she begins to bleed, this is the start of the menstrual cycle and the reproductive stage.
Menarche [edit | edit source]
This occurs at the beginning of the reproductive stage and is marked by the first menstrual period. It occurs during the late stages of puberty and signals the probability of ovulation and the beginning of a woman’s reproductive years.[2]Chronological age is not a useful predictor, and the Tanner Stages and signs and symptoms are more accurate.
Early onset, or “Precocious Puberty”, occurs before age 8. This may indicate endocrine disorders related to obesity, low birth weight, mother's preeclampsia, stress and a lack of exercise.
The absence of menarche onset, or "Amenorrhea", could be indicative other processes in the body and pregnancy should be the first thing to be ruled out.
Late or delayed onset, “Primary Amenorrhea”, is when menarche fails to occur 3 years after breast development or after 16 years of age. This may indicate Diabetes mellitus type 1, asthma, untreated celiac disease, cystic fibrosis or inflammatory diseases. Late menarche is associated with a decreased risk of developing breast cancer, a decreased frequency of coronary heart disease and reduction in teen pregnancy.
Menstruation[edit | edit source]
A menstrual period defined as “the monthly shedding of the functional layer (the endometrial lining) of the uterus.”
At the beginning of the menstrual cycle, there are erratic hormone fluctuations which eventually stabilise. Follicles are present in a high percentage of girls, however, ovulation does not occur until the girl has had an average of six regular menstrual cycles and monthly ovulation does not become regular for several years.
An "ideal" menstrual cycle is 28 days long. Day one is the menses, or when the bleeding starts. This commonly lasts for five to seven days and menses is included in the follicular phase. After the cessation of bleeding, the endometrial lining, which is inner lining of the uterus, begins to thicken until the egg is released. Ovulation, which is the release of the egg, then occurs. The following phase is the Luteal phase. The egg could either be fertilised and implant in the thickened endometrium, or if it is not fertilised, the the egg and the thickened portion of the endometrium, is broken down and expelled.This is the beginning of Menses Day 1.
Schedule a medical check up if the girl:
- Has not started menstruating within 3 years of breast growth or by the age of 15
- Breasts have not started to grow by the age of 13
- Has a period that lasts more than 7 days
- Has severe pain during periods
- Bleeds between periods
- Gets sick or has a sudden onset of fever after using a tampon
- Has a period that occurs more frequently than 21 days or less frequently than 45 days
- Goes 3 months without a period after beginning menstruation
For more information, please see Menstruation and Menstrual Rehab
Menopause[edit | edit source]
This stage occurs at the end of the reproductive stage and is marked by the final menstrual period (FMP). [3]Exact timing of this period can not be forecast and is pinpointed retrospectively when 12 months have passed without a period. The beginning of this transition is referred to as perimenopause and is triggered by the ovaries. The number of viable follicles drop to less than 1,000 and the signs and symptoms can begin to disrupt life[4]. This phase usually occurs between the ages of 45-58 years, but chronological age is not an accurate predictor. The STRAW+10 Staging Scale and common signs and symptoms are a far more useful predictor.
After a female has had no menstrual cycles for 12 months, she enters the post-menopause stage.
Schedule a medical check up if the woman:
- Has lengthening or skipped cycles (3 or more) before age 40
- Has a period that lasts more than 7 days
- Has unusual or severe pain during/between periods, or in postmenopause
- Has vaginal dryness, pain or blood when wiping after toileting
- Has difficulty sleeping &/or feeling tired all the time
- Is experiencing decreased quality of life due to symptoms
- Is bleeding in postmenopause
For more information, please see Menopause.
Signs & Symptoms (S&S)[edit | edit source]
Health care providers should be approaching menopause in the same way as menarche:
- Monitoring for regular functioning
- Identifying issues early and treating
- Initiating conversations prior to transitions
- Encouraging clients to make ‘healthy choices’ within their capability
| Puberty to Menarche | Perimenopause to Menopause |
|---|---|
| Secondary sex characteristics more pronounced | Vasomotor symptoms VMS (hot flashes/ night sweats) |
| Growth spurt | Vaginal dryness or Genitourinary Syndrome of Menopause (GSM) |
| Moodiness, short tempered, emotional | Moodiness, short tempered, emotional |
| Low energy/fatigue | Low energy/fatigue |
| Breast tenderness | Breast tenderness |
| Muscle aches | Muscle aches |
| Headaches | Headaches |
| Abdominal cramps | Abdominal cramps |
| Lower back pain | Lower back pain |
| Difficulty concentrating | Difficulty concentrating |
| Bloating, fluid retention | Bloating, fluid retention |
| Joint pain | Joint pain |
| Food cravings | Food cravings |
| Acne | Acne |
| Diarrhea/constipation | Diarrhea/constipation |
| Trouble sleeping | Trouble sleeping |
Common Medical Concerns in the Menopause Transition:[edit | edit source]
- Primary Ovarian Insufficiency
- This is diagnosed when the ovaries stop working before the age of 40
- Genitourinary Syndrome in Menopause
- A condition in which the vaginal walls and the vulva become thin and easily to break down. Symptoms often include feeling hot and rough, bleeding when wiping after toileting and discomfort. This condition can be treated with topical creams.
- Diseases which increase in risk post menopause:
- Cardiovascular
- Diabetes/Obesity
- Osteoporosis
- Dementia
- Cancer, mainly breast and uterine
Regular Assessments to include:[edit | edit source]
- Blood work
- To establish baselines or eliminate conditions such as thyroid disease and diabetes
- Test lipid levels every 2-3 yrs starting at age 40 yrs more often if Cardiovascular Disease is a risk
- ONLY if there’s an indication, testing of Calcium, Vitamin D and Hormones might be recommended
- Height and Weight
- ECG baseline
- Bone density scan is recommended from age 40 years for a baseline with a repeat every 5 years
- Assess for sleep/rest habits
- Assess for depression as it’s prevalence increases
- Pap test
- Mammogram is recommended from age 40 and monitoring every 3 years
- Colonoscopy is recommended from age 55
- Encourage clients to track signs and symptoms to facilitate & direct care. Review this information regularly
Healthy Choices[edit | edit source]
- Exercise should include aerobic, strengthening and balance
- Diet/Nutrition for maintenance of health
- Do not smoke
- Moderate intake of alcohol
- Sleep 8 hours per day
- Relaxation techniques
Stages of Reproductive Aging Workshop (STRAW)[edit | edit source]
In 2001, Stages of Reproductive Aging Workshop, otherwise known as STRAW, put together a standard for reproductive ageing. In 2011, STRAW was updated and modified to STRAW+10, which is the gold standard to identify stages within the sexual reproductive periods of a woman's lifespan.
STRAW divided the adult female life into three broad phases: Reproductive, The menopausal transition, and Postmenopause. These three phases included a total of seven stages centered around the Final Menstrual Period, referred to as Stage 0. 1–4
The reproductive phase was divided into Stages -5, which is Early, -4, Classified as Peak, and -3 or Late. Stage–3 was characterized by regular menstrual cycles and increasing levels of FSH.
The menopausal transition phase consisted of Stage -2 which was called Early and Stage -1, Late. Stage –2 was characterized by variability in menstrual cycle length and increased levels of FSH. Stage –1 was characterized by onset of skipped cycles or amenorrhea of at least 60 days and continued elevation of FSH.[5][6]
The postmenopause phase contained Stages +1, Early and +2, Late.
Please click here for a link to and article containing this table with further explanations.
Links to helpful pages[edit | edit source]
Additional Resources[edit | edit source]
Videos:[edit | edit source]
- Menstrual cycle an NHS site video
- Dr Jen Gunter, TED Talks on What really happens to your body during Menopause?
- Video: Am I Normal? (Girls and Puberty)
- What is Menarche? Everything you need to know
Recommended for Providers:[edit | edit source]
- Menopause Health Tool, Dr Jean Hailes
- Practitioner’s Toolkit, Monash University 2014
- Menopause Preparedness Fact Sheet, The Society of Women’s Health Research -October 2021.
Recommended for Clients & Parents/Guardians :[edit | edit source]
- Menopause Fact Sheet, August 2019, Dr Jean Hailes, Women’s Health, Available in English, Arabic, Chinese (Simplified), Farsi, Greek, Hindi, Italian, Turkish and Vietnamese. (This project was funded by the Victorian Government)
- Menstrual Calendar, for tracking perimenopause phase, NAMS, 2015
- Red Hot Mamas
- Menopause Barbie
- The North American Menopause Society
- US Department of Health and Human Services
- Healthy Women
- Canadian Society of Obstetricians and Gynaecologists
- Menstruation Around the World
- Menopause Map is a great interactive tool to start with to personalize your journey.
References[edit | edit source]
- ↑ Mendle J, Beltz AM, Carter R, Dorn LD. Understanding puberty and its measurement: ideas for research in a new generation. Journal of Research on Adolescence. 2019 Mar;29(1):82-95.
- ↑ Lacroix AE, Gondal H, Langaker MD. Physiology, menarche. InStatPearls [Internet] 2021 Mar 27. StatPearls Publishing.
- ↑ Talaulikar V. Menopause transition: Physiology and symptoms. Best Practice & Research Clinical Obstetrics & Gynaecology. 2022 Mar 16.
- ↑ Santoro N, Kravitz HM. The Disruptive Changes of Midlife: A Biopsychosocial Adventure. Obstetrics and Gynecology Clinics. 2018 Dec 1;45(4):xv-ii.
- ↑ Woods NF, Mitchell ES, Coslov N, Richardson MK. Transitioning to the menopausal transition: a scoping review of research on the late reproductive stage in reproductive aging. Menopause. 2021 Apr 1;28(4):447-66.
- ↑ Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, De Villiers TJ, STRAW+ 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop+ 10: addressing the unfinished agenda of staging reproductive aging. The Journal of Clinical Endocrinology & Metabolism. 2012 Apr 1;97(4):1159-68.