PT 858: Charcot-Marie-Tooth Disease Case Study
Original Editor -
Top Contributors -
Abstract[edit | edit source]
Introduction[edit | edit source]
Client Characteristics[edit | edit source]
The patient is a 25-year-old male. He works as an accountant and recently moved to the city for a job. He was diagnosed with autosomal dominant Charcot-Marie-Tooth (CMT) disease type 1A by a neurologist at the at of 14. To manage his symptoms, he typically sees a physiotherapist once a month, however, due to the busyness of the move, he was unable to see his physiotherapist for the 3 months leading up to moving and was unable to get an appointment with a new physiotherapist until now, one month after he moved. The patient has had multiple ankle sprains in the past 4 months, and in the past month has been unable to run due to an increased frequency of tripping over his own feet when increasing speed, in addition to general pain on the plantar surface of the foot. He reports feeling frustrated that he hasn’t be able to run and having a decreased mood. The patient self-referred to physiotherapy for maintenance of his condition and treatment.
Examination Findings[edit | edit source]
Subjective[edit | edit source]
History of Present Illness
In the past month, the patient has noticed that anytime he tried to increase his pace while walking, he found himself tripping over his feet and had to slow down to avoid falling. Prior to this, the patient reports tripping over his feet while running, and he believes this to be the cause of his recent sprained ankles. He reports that prior to 4 months ago, he would have ankle sprains occasionally, around once every year. However, in the past 4 months, he reports having one ankle sprain roughly every six weeks, with both ankles having been affected. The patient has not yet had any treatment for his ankle sprains, due to his missed appointments, but has received physiotherapy for treatment of CMT prior.
With respect to patient pain, he has reported an increase in plantar foot pain bilaterally in the past 3 months. The patient reports an increase in pain with walking over the last month. In addition, he also reports an increase in fatigue throughout the day, finding it more challenging to complete tasks around his home, such as cooking and cleaning.
Past Medical History
He was diagnosed with major depression disorder at 21.
The patient has had previous ankle sprains to both his left ankle (7 and 5 years ago) and his right ankle (4 and 3 years ago). He went to physio for the first ankle sprain 7 years ago, but not for the others.
In the past 4 months, he has had one sprain to his left ankle and 2 to his right ankle.
Medications
Ibuprofen (400 mg) 2 times per day for pain in ankles.
Fluoxetine (30 mg) once per day in the morning, though the patient reports that he often forgets to take it.
Health Habits
No history of smoking and consumes 2-3 alcoholic beverages per week.
Family History
His mother had autosomal dominant CMT type 1A, diagnosed when she was 16 years old.
Social History
The patient works as an accountant and lives alone in a one-bedroom apartment on the second floor of a building in a mid-sized city. There are 5 flights of stairs total inside the building, but there is an elevator. The patient’s parents and siblings live in another city around 3 hours away. When able, the patient enjoys running as well as cooking.
Functional History
The patient was independent in iADLs and bADLs. He did not use a gait aid, but has rearfoot varus wedge accommodative orthotics for his pes cavus. Prior to his ankle sprains, was running an average of 10-12 km per week and strength training 3 times each week .
Current Functional Status
He does not currently use gait aids or adaptive equipment, but is still wearing his orthotics. The patient feels he is moving slower and movements are more effortful, as well as that his sense of balance is not the same.
At home, he often chooses to take the elevator instead of walking the 2 flights of stairs to his third floor apartment and in recent weeks, has found he is too tired to cook, which he enjoys doing, and orders take-out more than usual.
Objective[edit | edit source]
Observation
- Mild (R) mid-thoracic scoliosis
- UE muscle tone appears normal
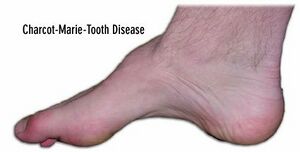
- Bilateral pes cavus, more extreme arch of (R) foot, varus heel angle from posterior POV
- Bilateral hammer toes
- Distal mild muscle wasting of bilateral lower legs, stork inverted champagne bottle appearance notable on anterio-lateral leg
Range of Motion
Upper Extremity - All joints within normal limits for passive and active range
Lower Extremity - Hip extension: 14 degrees (R), 16 degrees (L); Ankle Dorsiflexion: 5 degrees (R), 6 degrees (L)
***all end feels normal
Manual Muscle Testing
| Grade /5 (R) | Grade /5 (L) | |
| Hip Extension | 4+ | 4+ |
| Hip Flexion | 4 | 4 |
| Knee Extension | 5 | 5 |
| Knee Flexion | 4+ | 5 |
| Ankle Dorsiflexion | 3 | 3+ |
| Ankle Plantar Flexion | 4 | 4 |
| Ankle Inversion | 3+ | 3+ |
| Ankle Eversion | 5 | 5 |
Specific Muscle Strength Testing: determined tibialis anterior, extensor digitorum longus and extensor hallicus longus are primarily responsible for decreased strength of foot dorsiflexors and inverters
Neurological Assessment
Dermatomes: no deficits above the knee bilaterally. Below the knee does not follow a specific dermatomal pathway - altered sensation in L4-S1 below knee bilaterally. Patient presents with a stocking pattern.
UMN: Babinski (-), Hoffman’s (-), Oppenheimer’s (-)
LMN/Deep Tendon Reflexes:
- C6: Biceps/brachioradialis – 2 (normal)
- C7: Triceps – 2 (normal)
- L3L4: Patellar Tendon – 2 (normal)
- S1S2: Achilles Tendon – 1 (hyporeflexia)
Special Tests: Upper Extremity - Spurlings (-), Distraction (-), Vertebral Artery (-); Lower Extremity - Slump (-), Straight Leg Raise (-)
Sensation Testing:
A) Superficial Sensations: Light touch, temperature sense, and sharp/dull discrimination intact above the knee and impaired below the knee bilaterally.
B) Deep Sensations: Vibration sense intact above the knee and impaired below the knee bilaterally. Proprioreception/Kinesthesia impaired bilaterally for ankle dorsiflexion/plantarflexion.
Balance:
- Romberg Test (+) - loss of balance within 15 seconds with eyes open and 5 seconds with eyes closed
- Mini Best Score: 22/28
Observational Gait Analysis
Decreased stride length and increased time in double support were noted with no observable differences in stance phase, swing phase, or arm swing. There were noticeable bilateral pes cavus, distal mild bilateral lower legs, and anterior pelvic tilt. Increased compensation was observable at bilateral hips (hip hiking and circumduction). Bilateral mild foot drop was also observed. Using the 10m walk test, a gait speed of 1.2m/sec was calculated, which is lower than age normative values. Patient completed repeated heel walking for 20m, during the last 10m of the task bilateral reduction in ankle dorsiflexion was noted.
Outcome Measures
Clinical Impression[edit | edit source]
Analysis[edit | edit source]
Patient is a 25-year-old male with worsening lower extremity instability over the last 4 weeks that has impeded his ability to run. He presents with impaired balance, proprioception, reduced lower extremity strength, and overall reduced physical activity. Although the patient has CMT type 1A that will continue to progress, their previous high level of function plus activity, and young age are positive indicators for slowed progression of disability associated with his condition. Patient is a good candidate for physical therapy activities aimed at increasing strength of lower extremities, increasing dynamic balance, education on pacing, and optimizing participation in previously enjoyed physical activities.