Arteriosclerosis: Difference between revisions
(Created page with "<div class="noeditbox">This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}...") |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Uchechukwu Chukwuemeka|Uchechukwu Chukwuemeka]] <br> | |||
<div class="editorbox"> '''Original Editor '''- [[User: | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== | == Introduction == | ||
As one ages, the elasticity of the arterial walls reduces causing the wall to harden. The condition is referred to as arteriosclerosis (age-related stiffening and widening of the large arteries). It is pathologically distinct and some authors cap it as an umbrella name for three vascular diseases namely: [[atherosclerosis]], [[Atherosclerosis|arteriolosclerosis]], and Mönckeberg’s sclerosis<ref>Fishbein MC, Fishbein GA. Arteriosclerosis: facts and fancy. Cardiovascular Pathology. 2015; 24: 335–342. <nowiki>http://dx.doi.org/10.1016/j.carpath.2015.07.007</nowiki>. </ref> <ref>Kumar V, Abbas A, Aster J. Robbins & Cotran. Pathologic Basis of Disease. 9th ed. Philadelphia: Saunders; 2014.</ref>Therefore, it is likely that arteriosclerosis is the sequelae of a complicated pathological process involving multiple triggers and pathophysiology. There are neither symptoms nor signs of this condition because it’s an [[Ageing and Changes in Other Systems|ageing]] process. | |||
== Clinically Relevant Anatomy == | |||
Arteries supply the body with oxygenated blood – with the exception of the pulmonary arteries from the [[Anatomy of the Human Heart|heart]]; these carry deoxygenated blood to the [[Lung Anatomy|lungs]], and the umbilical artery, which carries deoxygenated blood from the foetus to the placenta. Blood travels from the arteries to the arterioles and to the capillaries, where [[Respiratory Physiotherapy|gaseous exchange]] takes place. | |||
The largest artery is the [[aorta]], which extends from the left ventricle down the left side of the body. It divides into four major regions, the ascending aorta, aortic arch, thoracic aorta, and abdominal aorta. | |||
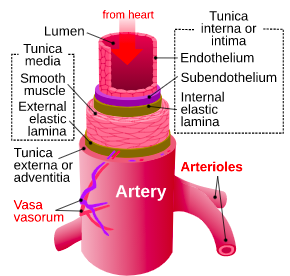
[[File:Artery layers.png|thumb|Arterial wall layers]] | |||
Arteries can be divided into elastic arteries, muscular arteries, and arterioles | |||
# Elastic arteries are the largest (1-2.5cm in diameter) and comprise large amounts of elastin as well as [[Muscle: Smooth|smooth muscle]]. They have a large lumen with a low resistance to blood flow and can expand and recoil to accommodate changes in blood volume. | |||
# Muscular arteries regulate local blood flow and deliver blood to individual organs. They measure 0.3mm-1cm in diameter and possess more smooth muscle but less elastin than elastic arteries. | |||
# Arterioles are the smallest arteries (0.01-0.3mm in diameter). In certain areas, they have all three vascular layers (tunica intima, media, and externa). When they are close to the capillaries they comprise a single smooth muscle layer overlying endothelial cells<span class="reference" id="cite_ref-:4_5-0"></span><ref>Nursing times. Vascular system. Available from: <nowiki>https://www.nursingtimes.net/clinical-archive/cardiovascular-clinical-archive/vascular-system-1-anatomy-and-physiology-26-03-2018/</nowiki> (accessed 29 June 2022)</ref> | |||
== | == Mechanism of Injury / Pathological Process == | ||
The regression models reviewed by Cecelja and Chowienczyk<ref>Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. ''Hypertension.'' 2009;54:1328 –1336</ref> indicate that age and [[Blood Pressure|blood pressure]] account for 50% of Pulse wave velocity (PWV) variation. It means that other risk factors asides from age and blood pressure also contribute to arteriosclerosis. Cross-sectional studies have highlighted potential culprits, such as medial calcification<ref>McEniery CM, McDonnell BJ, So A, Aitken S, Bolton CE, Munnery M, et al. Aortic calcification is associated with aortic stiffness and isolated systolic hypertension in healthy individuals. Hypertension. 2009; 53:524 –531</ref>, inflammation<ref>Yasmin, McEniery CM, Wallace S, Mackenzie IS, Cockcroft JR, Wilkinson IB. C-reactive protein is associated with arterial stiffness in apparently healthy individuals. Arterioscler Thromb Vasc Biol. 2004;24: 969–974</ref>, and deposition of advanced glycation end products<ref>Semba RD, Najjar SS, Sun K, Lakatta EG, Ferrucci L. Serum carboxymethyl-lysine, an advanced glycation end product, is associated with increased aortic pulse wave velocity in adults. Am J Hypertens. 2009;22:74 –79</ref>. With increasing age and shear pressure, the arterial wall gradually looses its elasticity and became stiff and dilated. The hardening of the arteries will further precipitate increased blood flow turbulence, further giving rise to increased pressure. This, in turn, will cause plaque depositions that can narrow the lumen of the vessel giving rise to either atherosclerosis, arteriolosclerosis, or Mönckeberg’s sclerosis depending on the site of stiffness and deposition of atheroma. | |||
Aortic stiffness can independently predict future cardiovascular risk in different populations<ref>Laurent S, Cockcroft JR, van Bortel LM, Boutouyrie P, Giannattasio C, Hayoz D, et al. Abridged version of the expert consensus document on arterial stiffness. Artery Res. 2007;1:2–12.</ref>. Thus, arteriosclerosis could directly enhance [[Cardiovascular Disease|cardiovascular disease]] in many ways. Hardening of the large arteries has deleterious hemodynamic consequences, including a rise in pulse pressure and a reduction in shear stress oscillations (rate). A low diastolic and increased systolic pressure lowers myocardial blood flow while increasing the workload of the left ventricle; which may culminate in myocardial ischemia, fibrosis, and/or heart failure. A high pulse pressure may add more forceful push (pulsatility) in fragile capillaries, leading to damage, especially in high-flow, low-resistance organs (e.g. [[Kidney|kidneys]] and [[Brain Anatomy|brain]]), and also accelerate aortic stiffening via increased wall stress<ref>Wilkinson IB, McEniery CM, Cockcroft JR. Arteriosclerosis and Atherosclerosis Guilty by Association. Available from: <nowiki>http://ahajournals.org</nowiki> (accessed May 25, 2022)</ref> | |||
== Diagnostic Procedures == | |||
Doppler ultrasound: this is to measure the flow of blood and analyze if unusual or there are blockages | |||
Blood test: this is to check for any disease and measure [[cholesterol]] and glucose level. | |||
[[Electrocardiogram]]: this is to measure the electrical activities of the heart. | |||
Stress analysis: this is done to ascertain how the heart responds to stress using [[Heart Arrhythmias: Assessment|echocardiogram]] to take pictures of the heart during an exercise. | |||
== Management / Interventions == | |||
There are no treatments for arteriosclerosis because it is often due to ageing. Other arterial disorders it could give rise to can be managed. For further reading, see atherosclerosis...<br>Lifestyle changes such as aerobic exercises, a good diet, optimal blood pressure maintenance, and stress management can minimize the chances of early development. | |||
== Differential Diagnosis == | |||
* [[Atherosclerosis]] is a disease of elastic and large muscular arteries in which the atheroma is the characteristic lesion<ref>Atherosclerosis VS Arteriosclerosis, know the difference- southflocardio. May 25 2022</ref>. Atheromas are plaques deposited around the arterial wall. These deposits are usually fat and cholesterol accumulation that could narrow and/or block the lumen resulting in turbulent blood flow and increased pressure. Almost all cardiovascular risk factors give rise to atherosclerosis. | |||
* Mönckeberg's is a calcification process that involves only the tunica media<ref>Mönckeberg J. Über die reine Mediaverkalkung der Extremitätenarterien und ihr Verhalten zur Arteriosklerose. Virchows Arch 1903:141–67</ref>. Mönckeberg's may be idiopathic or associated with diabetes mellitus and/or renal failure. | |||
* Arteriolosclerosis is a thickening of the wall of very small arteries, those with one or two layers of smooth muscle cells, by intimal fibromuscular tissue or “hyaline” deposition, typically associated with hypertension or diabetes. | |||
== Conclusion == | |||
In summary, arteriosclerosis is mostly due to ageing. There are no symptoms and as such, no cure. But, some lifestyle changes such as [[aerobic exercises]], healthy diet, optimal blood pressure maintenance, and stress management can minimize the chances of early development. The arterial stiffness could lead to atheroma formation in the vessel leading to atherosclerosis. | |||
== References | == References == | ||
<references />. | <references />. | ||
Revision as of 11:34, 28 June 2022
Top Contributors - Uchechukwu Chukwuemeka and Shaimaa Eldib
Introduction[edit | edit source]
As one ages, the elasticity of the arterial walls reduces causing the wall to harden. The condition is referred to as arteriosclerosis (age-related stiffening and widening of the large arteries). It is pathologically distinct and some authors cap it as an umbrella name for three vascular diseases namely: atherosclerosis, arteriolosclerosis, and Mönckeberg’s sclerosis[1] [2]Therefore, it is likely that arteriosclerosis is the sequelae of a complicated pathological process involving multiple triggers and pathophysiology. There are neither symptoms nor signs of this condition because it’s an ageing process.
Clinically Relevant Anatomy[edit | edit source]
Arteries supply the body with oxygenated blood – with the exception of the pulmonary arteries from the heart; these carry deoxygenated blood to the lungs, and the umbilical artery, which carries deoxygenated blood from the foetus to the placenta. Blood travels from the arteries to the arterioles and to the capillaries, where gaseous exchange takes place.
The largest artery is the aorta, which extends from the left ventricle down the left side of the body. It divides into four major regions, the ascending aorta, aortic arch, thoracic aorta, and abdominal aorta.
Arteries can be divided into elastic arteries, muscular arteries, and arterioles
- Elastic arteries are the largest (1-2.5cm in diameter) and comprise large amounts of elastin as well as smooth muscle. They have a large lumen with a low resistance to blood flow and can expand and recoil to accommodate changes in blood volume.
- Muscular arteries regulate local blood flow and deliver blood to individual organs. They measure 0.3mm-1cm in diameter and possess more smooth muscle but less elastin than elastic arteries.
- Arterioles are the smallest arteries (0.01-0.3mm in diameter). In certain areas, they have all three vascular layers (tunica intima, media, and externa). When they are close to the capillaries they comprise a single smooth muscle layer overlying endothelial cells[3]
Mechanism of Injury / Pathological Process[edit | edit source]
The regression models reviewed by Cecelja and Chowienczyk[4] indicate that age and blood pressure account for 50% of Pulse wave velocity (PWV) variation. It means that other risk factors asides from age and blood pressure also contribute to arteriosclerosis. Cross-sectional studies have highlighted potential culprits, such as medial calcification[5], inflammation[6], and deposition of advanced glycation end products[7]. With increasing age and shear pressure, the arterial wall gradually looses its elasticity and became stiff and dilated. The hardening of the arteries will further precipitate increased blood flow turbulence, further giving rise to increased pressure. This, in turn, will cause plaque depositions that can narrow the lumen of the vessel giving rise to either atherosclerosis, arteriolosclerosis, or Mönckeberg’s sclerosis depending on the site of stiffness and deposition of atheroma.
Aortic stiffness can independently predict future cardiovascular risk in different populations[8]. Thus, arteriosclerosis could directly enhance cardiovascular disease in many ways. Hardening of the large arteries has deleterious hemodynamic consequences, including a rise in pulse pressure and a reduction in shear stress oscillations (rate). A low diastolic and increased systolic pressure lowers myocardial blood flow while increasing the workload of the left ventricle; which may culminate in myocardial ischemia, fibrosis, and/or heart failure. A high pulse pressure may add more forceful push (pulsatility) in fragile capillaries, leading to damage, especially in high-flow, low-resistance organs (e.g. kidneys and brain), and also accelerate aortic stiffening via increased wall stress[9]
Diagnostic Procedures[edit | edit source]
Doppler ultrasound: this is to measure the flow of blood and analyze if unusual or there are blockages
Blood test: this is to check for any disease and measure cholesterol and glucose level.
Electrocardiogram: this is to measure the electrical activities of the heart.
Stress analysis: this is done to ascertain how the heart responds to stress using echocardiogram to take pictures of the heart during an exercise.
Management / Interventions[edit | edit source]
There are no treatments for arteriosclerosis because it is often due to ageing. Other arterial disorders it could give rise to can be managed. For further reading, see atherosclerosis...
Lifestyle changes such as aerobic exercises, a good diet, optimal blood pressure maintenance, and stress management can minimize the chances of early development.
Differential Diagnosis[edit | edit source]
- Atherosclerosis is a disease of elastic and large muscular arteries in which the atheroma is the characteristic lesion[10]. Atheromas are plaques deposited around the arterial wall. These deposits are usually fat and cholesterol accumulation that could narrow and/or block the lumen resulting in turbulent blood flow and increased pressure. Almost all cardiovascular risk factors give rise to atherosclerosis.
- Mönckeberg's is a calcification process that involves only the tunica media[11]. Mönckeberg's may be idiopathic or associated with diabetes mellitus and/or renal failure.
- Arteriolosclerosis is a thickening of the wall of very small arteries, those with one or two layers of smooth muscle cells, by intimal fibromuscular tissue or “hyaline” deposition, typically associated with hypertension or diabetes.
Conclusion[edit | edit source]
In summary, arteriosclerosis is mostly due to ageing. There are no symptoms and as such, no cure. But, some lifestyle changes such as aerobic exercises, healthy diet, optimal blood pressure maintenance, and stress management can minimize the chances of early development. The arterial stiffness could lead to atheroma formation in the vessel leading to atherosclerosis.
References[edit | edit source]
- ↑ Fishbein MC, Fishbein GA. Arteriosclerosis: facts and fancy. Cardiovascular Pathology. 2015; 24: 335–342. http://dx.doi.org/10.1016/j.carpath.2015.07.007.
- ↑ Kumar V, Abbas A, Aster J. Robbins & Cotran. Pathologic Basis of Disease. 9th ed. Philadelphia: Saunders; 2014.
- ↑ Nursing times. Vascular system. Available from: https://www.nursingtimes.net/clinical-archive/cardiovascular-clinical-archive/vascular-system-1-anatomy-and-physiology-26-03-2018/ (accessed 29 June 2022)
- ↑ Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension. 2009;54:1328 –1336
- ↑ McEniery CM, McDonnell BJ, So A, Aitken S, Bolton CE, Munnery M, et al. Aortic calcification is associated with aortic stiffness and isolated systolic hypertension in healthy individuals. Hypertension. 2009; 53:524 –531
- ↑ Yasmin, McEniery CM, Wallace S, Mackenzie IS, Cockcroft JR, Wilkinson IB. C-reactive protein is associated with arterial stiffness in apparently healthy individuals. Arterioscler Thromb Vasc Biol. 2004;24: 969–974
- ↑ Semba RD, Najjar SS, Sun K, Lakatta EG, Ferrucci L. Serum carboxymethyl-lysine, an advanced glycation end product, is associated with increased aortic pulse wave velocity in adults. Am J Hypertens. 2009;22:74 –79
- ↑ Laurent S, Cockcroft JR, van Bortel LM, Boutouyrie P, Giannattasio C, Hayoz D, et al. Abridged version of the expert consensus document on arterial stiffness. Artery Res. 2007;1:2–12.
- ↑ Wilkinson IB, McEniery CM, Cockcroft JR. Arteriosclerosis and Atherosclerosis Guilty by Association. Available from: http://ahajournals.org (accessed May 25, 2022)
- ↑ Atherosclerosis VS Arteriosclerosis, know the difference- southflocardio. May 25 2022
- ↑ Mönckeberg J. Über die reine Mediaverkalkung der Extremitätenarterien und ihr Verhalten zur Arteriosklerose. Virchows Arch 1903:141–67
.