Blood Pressure
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Lucinda hampton, Vidya Acharya, Wanda van Niekerk, Naomi O'Reilly and Angeliki Chorti
Introduction[edit | edit source]
In general, an individual’s “blood pressure" (systemic arterial pressure) refers to the pressure measured within large arteries in the systemic circulation. This number splits into systolic blood pressure and diastolic blood pressure.
Blood pressure is traditionally measured using auscultation with a mercury-tube sphygmomanometer. It is measured in millimeters of mercury and expressed in terms of systolic pressure over diastolic pressure.
- Systolic pressure refers to the maximum pressure within the large arteries when the heart muscle contracts to propel blood through the body.
- Diastolic pressure describes the lowest pressure within the large arteries during heart muscle relaxation between beating. [1]
Blood pressure is one of the most commonly measured clinical parameters and blood pressure values are major determinants of therapeutic decisions.[2]
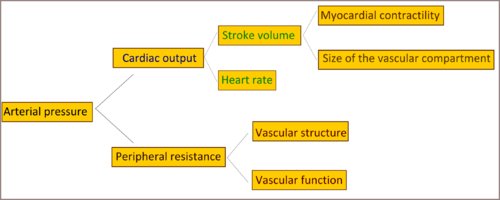
Arterial pressure directly corresponds to
- Cardiac output
- Arterial elasticity
- Peripheral vascular resistance
Blood pressure is remarkably easy to alter and can be affected by many activities.[1]
Maintaining Blood Pressure within normal limits[edit | edit source]
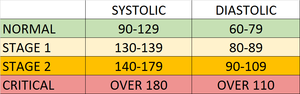
Maintaining blood pressure within normal limits is essential.
- A blood pressure between 140/80 mmHg to 159/99 mmHg is classified to as stage 1 hypertension.
- Stage 2 hypertension is a pressure between 160/100 mmHg to 179/109 mmHg.
- Hypertensive urgency describes a blood pressure greater than 180/110 mmHg.
- Hypertensive emergency refers to a very high blood pressure that results in potentially life-threatening symptoms and end-organ damage.
- Hypotension, on the other hand, is a blood pressure less than 90/60 mmHg.
It is crucial for the body to be able to adjust to acute changes in blood pressure and for the patient to receive medical treatment or lifestyle adjustments for chronic variations.
Mechanism of maintaining normal Blood Pressure[edit | edit source]
There are several mechanisms through which the body regulates arterial pressure.
Baroreceptor Reflex[edit | edit source]
In response to acute changes in blood pressure, the body responds through the baroreceptors located within blood vessels. Baroreceptors are a form of mechanoreceptor that become activated by the stretching of the vessel. This sensory information is conveyed to the central nervous system and used to influence peripheral vascular resistance and cardiac output.
There are two forms of baroreceptors.
- High-Pressure Baroreceptors: Two baroreceptors are located within the high-pressure arterial system:
- The carotid baroreceptor responds to both increases and decreases in blood pressure and sends afferent signals via the glossopharyngeal nerve (CN IX).
- The aortic arch baroreceptor responds only to increases in blood pressure, sending its signals through the vagus nerve (CN X).
- Low-Pressure Baroreceptors
Antidiuretic Hormone[edit | edit source]
Antidiuretic hormone (ADH) is a hormone synthesized in the hypothalamus. ADH is synthesized and released in response to multiple triggers which are:
- High serum osmolarity, which acts on osmoreceptors in the hypothalamus
- Low blood volume causes a decreased stretch in the low-pressure baroreceptors, leading to the production of ADH
- Decreased blood pressure causes decreased stretch in the high-pressure baroreceptors, also leading to the production of ADH
- Angiotensin II
ADH mainly functions to increase free water reabsorption in the collecting duct of the nephrons within the kidney, causing an increase in plasma volume and arterial pressure. ADH in high concentrations also causes moderate vasoconstriction, increasing peripheral resistance, and arterial pressure.
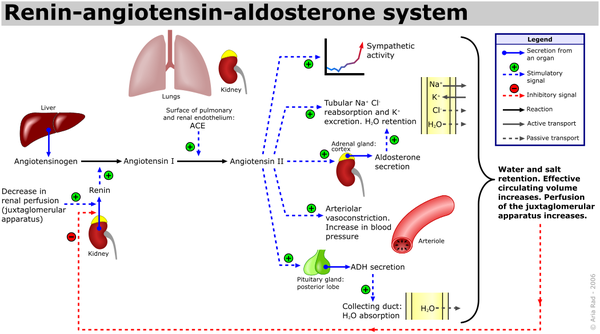
Renin-Angiotensin-Aldosterone System (RAAS)[edit | edit source]
The renin-angiotensin-aldosterone system (RAAS) is a critical regulator of blood volume and systemic vascular resistance.
- While the baroreceptor reflex responds in a short-term manner to decreased arterial pressure, the RAAS is responsible for more chronic alterations.
- It does this by increasing sodium reabsorption, water reabsorption, and vascular tone.
- It is composed of three major compounds: renin, angiotensin II, and aldosterone.
- These three act to elevate arterial pressure in response to decreased renal blood pressure, decreased salt delivery to the distal convoluted tubule, and/or beta-agonism.
Through these mechanisms, the body can elevate the blood pressure in a prolonged manner.[3] See image on the right.
Though the RAAS serves a critical function, it can be activated inappropriately in several conditions that may then lead to the development of hypertension. For example, renal artery stenosis results in a decreased volume of blood reaching one (or both) kidneys resulting in the juxtaglomerular cells sensing a decrease in blood volume, activating the RAAS. This can lead to an inappropriate elevation of circulating blood volume and arteriolar tone due to poor renal perfusion.[3]
Hypertension[edit | edit source]
Hypertension ranks among the most common chronic medical conditions, characterized by a persistent elevation in the arterial pressure.
Raised blood pressure is a major risk factor for chronic heart disease, stroke, and coronary heart disease. Elevated BP is positively correlated to the risk of stroke and coronary heart disease. Other complications include heart failure, peripheral vascular disease, renal impairment, retinal hemorrhage, and visual impairment.[4]
Most cases of hypertension are idiopathic which is also known as essential hypertension.
- An increase in salt intake increases the risk of developing hypertension.
- A factor for the development of essential hypertension is the patient genetic ability to salt response. About 50 to 60% of the patients are salt sensitive and therefore tend to develop hypertension.
More than one billion adults worldwide have hypertension with up to 45% of the adult populace being affected with the disease. The high prevalence of hypertension is consistent across all socio-economic and income strata, and the prevalence rises with age accounting for up to 60% of the population above 60 years of age.
In the year 2010, the global health survey report, published in Lancet (67 countries included), reported Hypertension as the leading cause of death and disability-adjusted life years worldwide since the year 1990.[5]
How to control high blood pressure
- Following a healthy diet; reducing salt and fat intake and eating plenty of fruit and vegetables
- Regular physical activity
- Maintaining a healthy weight
- Limiting your alcohol intake
- Stopping smoking
- Taking BP medications if prescribed
Hypotension[edit | edit source]
Hypotension is a decrease in systemic blood pressure below accepted low values.
- While there is not an accepted standard hypotensive value, pressures less than 90/60 are recognized as hypotensive.
- Hypotension is a relatively benign condition that is under-recognized mainly because it is typically asymptomatic.
- It only becomes a concern once pumping pressure is not sufficient to perfuse key organs with oxygenated blood.[6]
Clinical Significance[edit | edit source]
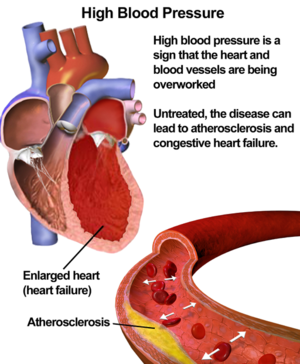
Blood pressure is important because the higher blood pressure is, the higher the risk of health problems in the future.
If blood pressure is high, it is putting extra strain on arteries and on the heart. Over time, this strain can cause the arteries to become thicker and less flexible, or to become weaker.
It is important to keep an eye on clients' blood pressure and make sure it’s not getting too high.
- High blood pressure (HBP) can be deadly. It’s sometimes called "the silent killer" because it has no symptoms. BP is easily monitored by eg a health professional.
- HBP is the single biggest risk factor for heart disease, stroke, and other cardiovascular problems.
- If it’s left untreated it could lead to heart attack, heart disease, congestive heart failure, atherosclerosis, stroke, kidney damage, vision loss, erectile dysfunction, memory loss, fluid in the lungs, chest pain or discomfort and peripheral artery disease.
- Hypertension is a chronic disorder and requires long-term care and management. Detailed education regarding lifestyle modification and pharmacological therapy is the key to success for better control of blood pressure and to prevent complications. Weight management, healthy eating, physical activity, limiting alcohol/tobacco/smoking is a critical strategy to decrease cardiovascular risk.[5] A systematic review and meta-analysis suggested that the spinal manipulations and mobilizations significantly decreased systolic and diastolic blood pressure[7].
References[edit | edit source]
- ↑ 1.0 1.1 Shahoud JS, Aeddula NR. Physiology, Arterial Pressure Regulation. InStatPearls [Internet] 2019 Feb 11. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK538509/ (last accessed 4.3.2020)
- ↑ Magder S. The meaning of blood pressure. Critical Care. 2018 Dec 1;22(1):257. Available from:https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2171-1 (last accessed 4.3,2020)
- ↑ 3.0 3.1 Fountain JH, Lappin SL. Physiology, Renin Angiotensin System. InStatPearls [Internet] 2019 May 5. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK470410/ (last accessed 4.3.2020)
- ↑ Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. International journal of hypertension. 2017;2017. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5733954/ (last accessed 4.3.2020)
- ↑ 5.0 5.1 Iqbal AM, Jamal SF. Essential Hypertension. InStatPearls [Internet] 2019 Apr 3. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK539859/ (last accessed 4.3.2020)
- ↑ Sharma S, Bhattacharya PT. Hypotension. InStatPearls [Internet] 2019 Mar 8. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK499961/ (last accessed 4.3.2020)
- ↑ Gera C, Malik M, Kaur J, Saini M. A systematic review and meta-analysis on effect of spinal mobilization and manipulation on cardiovascular responses. Hong Kong Physiotherapy Journal. 2020 Dec 6;40(02):75-87.