Hypertension
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Nupur Smit Shah, Rishika Babburu and Areeba Raja
Introduction[edit | edit source]
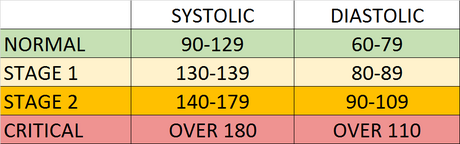
The current definition of hypertension (HTN) is systolic blood pressure (SBP) values of 130mmHg or more and/or diastolic blood pressure (DBP) more than 80 mmHg. Persistent BP readings of 140/90mmHg or more should undergo treatment with the usual therapeutic target of 130/80mmHg or less.[1]
Salient Facts
- HTN is a serious medical condition that significantly increases the risks of heart, brain, kidney and other diseases.
- An estimated 1.13 billion people worldwide have HTN, most (two-thirds) living in low- and middle-income countries.
- In 2015, 1 in 4 men and 1 in 5 women had hypertension.
- Fewer than 1 in 5 people with hypertension have the problem under control.
- HTN accounts for more than 9.3 million deaths per year, surpassing tobacco with around 8 million deaths per year[2].[1]
- One of the global targets for noncommunicable diseases is to reduce the prevalence of hypertension by 25% by 2025 (baseline 2010)[3].
Etiology[edit | edit source]
Most cases of hypertension are idiopathic which is also known as essential hypertension.
- It has long been suggested that an increase in salt intake increases the risk of developing hypertension.
- One of the described factors for the development of essential hypertension is the patient genetic ability to salt response. Salt sensitivity is a measure of how blood pressure responds to salt intake. People are either salt-sensitive or salt-resistant. Those who are sensitive to salt are more likely to have high blood pressure than those who are resistant to salt.[4][1]
- Poor sleep quality or sleep apnoea, excess alcohol intake and mental stress could also contribute to the development of hypertension.[5][6][7]
Risk Factors[edit | edit source]
Divided into 2 categories
- Modifiable risk factors: unhealthy diets eg excessive salt consumption, a diet high in saturated fat and trans fats, low intake of fruits and vegetables); physical inactivity, consumption of tobacco and alcohol; being overweight or obese.
- Non-modifiable risk factors include: a family history of hypertension; age over 65 years; co-existing diseases eg diabetes or kidney disease[3].
Signs and Symptoms[edit | edit source]
Hypertension is called a "silent killer". Most people with hypertension are unaware of the problem because it may have no warning signs or symptoms.
- When symptoms do occur they include: early morning headaches; nosebleeds; irregular heart rhythms; vision changes; buzzing in the ears.
- Severe hypertension can cause: fatigue; nausea; vomiting; confusion; anxiety; chest pain; muscle tremors.
An evaluation of BP by a health professional is important for assessment of risk and associated conditions[3].
Epidemiology[edit | edit source]
An estimated 1.28 billion adults aged 30-79 years worldwide have hypertension, most (two-thirds) living in low- and middle-income countries.[8]
- Less than half of adults (42%) with hypertension are diagnosed and treated.
- One of the global targets for noncommunicable diseases is to reduce the prevalence of hypertension by 33% between 2010 and 2030.[8]
Pathophysiology[edit | edit source]
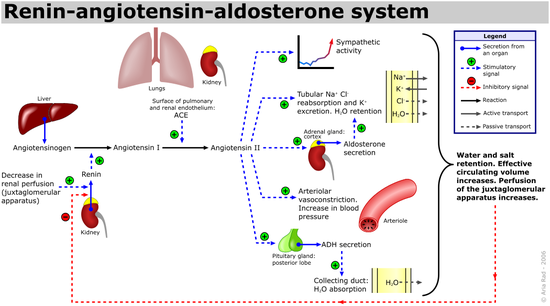
There are various mechanisms described for the development of hypertension which includes:
- Increased salt absorption resulting in volume expansion,
- An impaired response of the renin-angiotensin-aldosterone system (RAAS),
- Increased activation of the sympathetic nervous system.
These changes lead to the development of increased total peripheral resistance and increased afterload which in turn leads to the development of hypertension[1].
Measurement and Diagnosis[edit | edit source]
Identifying patients with abnormal blood pressure and accurately diagnosing hypertension is extremely important for both health care providers and patients.
Measure blood pressure when client is relaxed and sitting. A sphygmomanometer is used to measure BP and an inflatable pressure cuff around the upper arm. Blood pressure is recorded as two numbers, eg 120/80. The larger number indicates the pressure in the arteries as the heart pumps out blood during each beat (systolic blood pressure). The lower number indicates the pressure as the heart relaxes before the next beat (diastolic blood pressure). Both are measured in units called millimetres of mercury (mmHg)[9].
Relying on precise BP readings is important, ambulatory BP monitoring is currently regarded as the gold standard technique for clinical decision making and is a better predictor of outcomes than office and home BP monitoring[2].
Non Pharmacological management[edit | edit source]
Education regarding the importance of:
- Reducing salt intake (to less than 5g daily).
- Eating more fruit and vegetables.
- Being physically active on a regular basis.
- Avoiding use of tobacco.
- Reducing alcohol consumption.
- Limiting the intake of foods high in saturated fats.
- Eliminating/reducing trans fats in diet.
- Reducing and managing mental stress
- Regularly checking blood pressure
- Managing other medical conditions[1][8][3]
Pharmacological Management of Hypertension[edit | edit source]
Pharmacological management of HTN consists of angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARBs), diuretics (usually thiazides), calcium channel blockers (CCBs) and beta-blockers (BBs), which are instituted taking into account age, race and comorbidities such as presence of renal dysfunction, LV dysfunction, heart failure and cerebrovascular disease. See link.
Complications[edit | edit source]
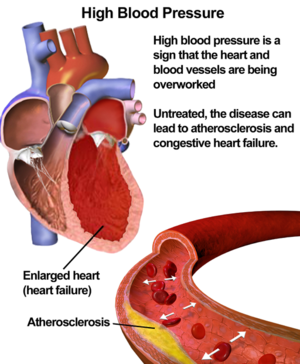
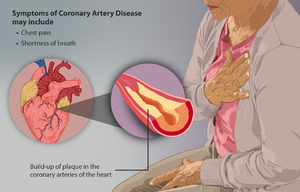
There is a clear link between high blood pressure and an increased risk of heart disease, in particular having a heart attack or stroke[10]. Complications also include:
- Coronary Artery disease (CAD)
- Hypertensive encephalopathy
- Renal failure, acute versus chronic
- Peripheral arterial disease
- Atrial fibrillation
- Aortic aneurysm
- Death (usually due to coronary heart disease, vascular disease, stroke-related)
Resistant Hypertension (RHTN) and Refractory Hypertension[edit | edit source]
1.RHTN
Defined as uncontrolled blood pressure despite the use of ≥3 antihypertensive agents of different classes, including a diuretic, a long-acting calcium channel blocker, and a blocker of the renin- angiotensin system, at maximal or maximally tolerated doses.
- Antihypertensive medication nonadherence and the white coat effect must be excluded to make the diagnosis.
- RHTN is a high-risk phenotype, leading to increased all-cause mortality and cardiovascular disease outcomes.
- Healthy lifestyle habits are associated with reduced cardiovascular risk in patients with RHTN.
- Aldosterone excess is common in patients with RHTN, and addition of spironolactone or amiloride to the standard 3-drug antihypertensive regimen is effective at getting the blood pressure to goal in most of these patients.
2. Refractory hypertension
Defined as uncontrolled blood pressure despite use of ≥5 antihypertensive agents of different classes, including a long-acting thiazide-like diuretic and an MR (mineralocorticoid receptor) antagonist, at maximal or maximally tolerated doses. Fluid retention, mediated largely by aldosterone excess, is the predominant mechanism underlying RHTN, while patients with refractory hypertension typically exhibit increased sympathetic nervous system activity.[11]
Differential Diagnosis[edit | edit source]
- Secondary hypertension should always be sought for as the differential especially if the patient is at extremes of age (young or elderly).
- Hyperaldosteronism, coarctation of the aorta, renal artery stenosis, chronic kidney disease, and aortic valve disease should always be kept in the differential.[1]
Patient Education Recommendations[edit | edit source]
Physical therapists should contribute to educating patients to monitor and manage their blood pressure, as early as childhood, before it becomes a serious health problem. The incidence of pediatric hypertension is increasing as a result of the obesity epidemic. Diet and exercise implemented at a young age are crucial in the prevention of hypertension.[12] When medications are implicated, adherence is crucial in long-term management. It has been shown that approximately 50% of patients don’t take medications as prescribed.[13] According to the WHO, “lack of adherence is the most important cause of failure to achieve BP control”.[10] While medication adherence is important, physical activity should be equally emphasized, especially because it’s a primary prevention technique. Aerobic exercise is universally implemented for hypertensive treatment because it lowers BP 5-7 mmHg among adults. Thirty minutes or more per day of moderate-intensity exercise combined with resistance exercise 2-3 days per week is recommended.[14]
Management[edit | edit source]
- Jacobson's method of progressive relaxation is proven to be effective in treating hypertension. In this method, the group of muscles is contracted and relaxed, each contraction is coordinated with deep breathing and it is done in a supine lying position for 30 minutes.[15]
- Land base and water-based aerobic exercise program are beneficial in females having post-menopausal hypertension.
- Aquatic exercises like walking in the swimming pool, lower limb stretching, deep water running techniques and land-based exercises like walking, lower limb stretching and stationary biking were proven to be effective. [16]
- Slow loading breathing technique is useful in reducing isolated systolic hypertension(resting blood pressure).
Resources[edit | edit source]
Exercise for the Prevention and Treatment of Hypertension - Implications and Application
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Iqbal AM, Jamal SF. Essential Hypertension. InStatPearls [Internet] 2019 Dec 1. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK539859/?report=reader (last accessed 11.12.2020)
- ↑ 2.0 2.1 Pena-Hernandez C, Nugent K, Tuncel M. Twenty-four-hour ambulatory blood pressure monitoring. Journal of Primary Care & Community Health. 2020 Jul;11:2150132720940519. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7356999/(accessed 28.3.2022)
- ↑ 3.0 3.1 3.2 3.3 WHO Hypertension Available from:https://www.who.int/news-room/fact-sheets/detail/hypertension (last accessed 11.12.2020)
- ↑ GB Watch Health Trait salt sensitivity Available: https://www.gbhealthwatch.com/Trait-Salt-Sensitivity.php(accessed 28.3.2022)
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229731/
- ↑ https://www.researchgate.net/profile/Dieter-Riemann/publication/233749083_Sleep_Loss_and_Hypertension_A_Systematic_Review/links/0fcfd50b9d9236bbfd000000/Sleep-Loss-and-Hypertension-A-Systematic-Review.pdf
- ↑ https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0129163
- ↑ 8.0 8.1 8.2 WHO Hypertension Available: https://www.who.int/news-room/fact-sheets/detail/hypertension(accessed 28.3.2022)
- ↑ Heart Foundation Blood Pressure Available from:https://www.heartfoundation.org.au/heart-health-education/blood-pressure-and-your-heart (last accessed 12.12.2020)
- ↑ Oh GC, Cho HJ. Blood pressure and heart failure. Clinical Hypertension. 2020 Dec 1;26(1):1.Available from:https://clinicalhypertension.biomedcentral.com/articles/10.1186/s40885-019-0132-x (last accessed 12.12.2020)
- ↑ Acelajado MC, Hughes ZH, Oparil S, Calhoun DA. Treatment of resistant and refractory hypertension. Circulation research. 2019 Mar 29;124(7):1061-70.Available from:https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.118.312156 (accessed 12.12.2020)
- ↑ Misurac, J, Nichols, KR, Wilson, AC. Pharmacologic management of pediatric hypertension. Pediatric Drugs. February, 2016; 18(1), 31-43. doi:http://dx.doi.org/10.1007/s40272-015-0151-3. Accessed November 29, 2018.
- ↑ Brown, MT, Bussell, JK. Medication Adherence: WHO Cares? Mayo Clinic Proceedings. April, 2011; 86(4), 304–314. http://doi.org/10.4065/mcp.2010.0575. Available from: https://pubmed.ncbi.nlm.nih.gov/21389250/ Accesed November 12.12.2020
- ↑ Pescatello, LS, MacDonald, HV, Lamberti, L, Johnson, BT. Exercise for Hypertension: A Prescription Update Integrating Existing Recommendations with Emerging Research. Current Hypertension Reports. November, 2015; 17(11), 87.Available from:https://link.springer.com/article/10.1007/s11906-015-0600-y (last accessed 12.12.2020)
- ↑ Shinde N, Shinde KJ, Khatri SM, Hande D. Immediate effect of Jacobson's progressive muscular relaxation in hypertension. Indian Journal of Physiotherapy and Occupational Therapy. 2013 Jul 1;7(3):234.
- ↑ Arca EA, Martinelli B, Martin LC, Waisberg CB, Franco RJ. Aquatic exercise is as effective as dry land training to blood pressure reduction in postmenopausal hypertensive women. Physiotherapy Research International. 2014 Jun;19(2):93-8.