Cartilage: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) (Reformatted text and corrected grammatical errors) |
||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
Cartilage is a type of supporting connective tissue . It is a firm tissue but softer and more flexible than bone .<ref>http://www.news-medical.net/health/What-is-Cartilage.aspx</ref> | Cartilage is a non-vascular type of supporting connective tissue that is found throughout the body . It is a firm tissue but softer and more flexible than bone .<ref>http://www.news-medical.net/health/What-is-Cartilage.aspx</ref> It can be found in the larynx, respiratory tract, external ear, and in the articulating surfaces of joints. In babies many of the bones that form the skeleton are made primarily of cartilage, as children develop this cartilage will be replaced by bone. | ||
{{#ev:youtube|mr5JI8Q8dc8}}<ref>https://www.youtube.com/watch?v=mr5JI8Q8dc8</ref | {{#ev:youtube|mr5JI8Q8dc8}}<ref>https://www.youtube.com/watch?v=mr5JI8Q8dc8</ref> | ||
== Cartilage Structure | == Cartilage Structure == | ||
Cartilage is a dense structure, that resembles a firm gel, made up of collagen and elastic fibres. It contains polysacchride derivaites called chondroitin sulfates which complex with protein in the ground substance forming proteoglycan. The matrix is produced by cells call chrondroblasts which form chrondocytes and can be found in small chambers called lacuna<br> | |||
<span style="font-size: 16.6px;">Cartilage separated from the surrounding tissues by perichondrium which consist of two layers:</span> | |||
# <span style="font-size: 16.6px;">Outer Fibrous Layer : Which provide protection , mechanical support and attaches the cartilage to other structures.</span> | |||
# <span style="font-size: 16.6px;">Inner Cellular : It Is Important in the growth and maintenance of cartilage .</span><ref name="fredric">Fredric H.Martini ,Judi Nath ,Edwen Bartholomew , Charles M.Seiger ,Damian Hill . Fundamentals of Anatomy and Physiology .9th ed , 2011 .</ref> | |||
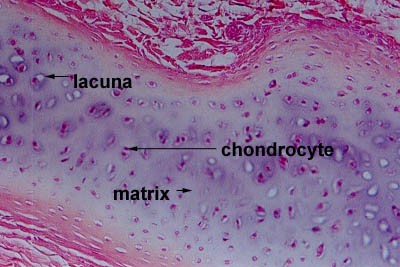
[[Image:Hyalinelabel.jpg|center]] | [[Image:Hyalinelabel.jpg|center]] | ||
<br> | <br> | ||
== Cartilage | == Types of Cartilage == | ||
There are three types of cartilage and they all have slightly different structures and function | |||
=== Hyaline Cartilage === | |||
Hyaline Cartilage has a smooth surface and is the most common of the three types of cartilage. It has a matrix that contains closely packed collagen fibers, making it tough but slightly flexible. It consists of a bluish-white, shiny ground elastic material, whose matrix contains chondtoitin sulphate, with many fine collagen fibrils and chrondrocytes. Because of its smooth surfaces it allows tissues to slide/glide more easily, as well as providing flexibility and support | |||
Example : Connection between ribs and sternum, nasal cartilage and articular cartilage (which covers opposing bone surfaces in many joints). | |||
<br> | === Fibrocartilage === | ||
Fibrocartilage is the toughest of the three types of cartilage. It has no perichondrium and has a matrix that contains dense bundles of collagen fibers embedded with chrondrocytes, making it durable and tough. This makes it perfect to provide support and rigidity<br><br>Example : Intervertebral discs (between spinal vertebrae), Menisci (cartilage pads of the knee joint), the callus (formed at the ends of bones at the site of a fracture), between the Pubic Symphysis and at the junction where tendons insert into bone. | |||
=== Elastic Cartilage === | |||
Elastic cartilage provides support. It has a yellowish colour and is surrounded by a perichnodrium. Chrondrocytes are located between a network of threadlike elastic fibres, the abundance of elastic fibres makes it flexible and resilient. | |||
<br>Example : the auricle of the outer ear . | |||
<br> | |||
[[Image:Three-types-of-cartilage-hyaline-elastic-and-fibrocartilage.png|center|500x350px]]<span style="font-size: 16.6px;"> <ref name="fredric" /></span> | |||
== Cartilage Growth == | |||
The growth of cartilage is a slow process and occurs by the division of cells. Both intersitial and appositional growth occur during development but neither of them occur in normal adult but under unusual circumstances appositional growth may occur as in cartilage damage (minor damage) .<ref name="fredric" /> | |||
=== Interstitial Growth === | |||
Chondrocytes responsible for cell division and daughter cells produce the matrix. This occurs during embryonic level and continues until adolescence. | |||
=== Appostional Growth === | |||
Cells of inner layer of perichondrium undergo division and inner most cells differentiate into immature chondrocytes which produce the matrix, they then mature into mature chondrocytes . | |||
<br> {{#ev:youtube|tS5S8BoVN-4}}<ref>https://www.youtube.com/watch?v=tS5S8BoVN-4</ref> | === Remodelling of Cartilage === | ||
This occurs predominantly by changes and the rearrangement of the collagen matrix in response to load.<br>{{#ev:youtube|tS5S8BoVN-4}}<ref>https://www.youtube.com/watch?v=tS5S8BoVN-4</ref> | |||
== Mechanical Behaviour of Articular Cartilage == | == Mechanical Behaviour of Articular Cartilage == | ||
The mechanical behaviour depend on interaction of its component : proteoglycan , collagen and interstitial fluid . | The mechanical behaviour depend on interaction of its component : proteoglycan , collagen and interstitial fluid. In an aqoues environment , proteogylcans are polyanionic which means the molecule has negatively charged sites that arise from sulfate and carboxyl. In solution, the mutual repulsion of these negative charges causes the aggregated proteogylcan to spread out and occupy a large volume . | ||
In the cartilage matrix, the volume occupied by proteogylcan aggregates is limited by the network of collagen fibres. when the cartilage is commpressed the negatively charged sites are pushed together increasing the mutual repulsion force adding to the compressive stiffness of the cartilage. During this process non-aggregated protoegylcans are not affected by the compressive load since they are not easily trapped in the cartilage matrix .Damage to the collagen framework reduces compressive stiffness . | |||
The mechanical response of the cartilage is strongly tied to the application of pressure differences and the flow of fluid through the tissue as, when deformed, the fluid flows across the cartilage and articular surface . | |||
=== Biphasic model of cartilage === | |||
All of the solid components of the cartilage (lipid, proteogylcans,cells and collagen ) are grouped together to form the solid component of the matrix and the interstitial fluid, that moves freely, forms the fluid component. | |||
<ref name="Carol">Carol A.Oatis . kinesiology the mechanics and pathomechanics of human movement , 2003 .</ref> | <ref name="Carol">Carol A.Oatis . kinesiology the mechanics and pathomechanics of human movement , 2003 .</ref> | ||
== Exercise and | == Exercise and Cartilage Health == | ||
Participation in certain sports appear to increase risk of osteoarthritis (result from breakdown of joint cartilage). Activities that involve torsional loading , fast acceleration and deceleration , repetitive high impact and high level of participation increase risk of osteoarthritis. Increased risks of osteoarthritis are related to excessive exercise or abnormal joint loading But some levels of loading and exercise are beneficial for joint health as exercise enhances production of matrix molecules, which can have a positive effect on joint health. Therefore exercise has both beneficial and detrimental effects on cartilage. Exercise can promote positive biomechanical changes, reduce pain and increase function of people with arthritis but it must be noted that sports injuries can be a contributing factor to developing osteoarthritis .<ref name="Carol" /><br> | |||
== References == | == References == | ||
References will automatically be added here, see [[Adding References|adding references tutorial]]. <references /> | References will automatically be added here, see [[Adding References|adding references tutorial]]. <references /> | ||
Revision as of 17:45, 17 May 2019
Top Contributors - Esraa Mohamed Abdullzaher, Lucinda hampton, Kim Jackson, George Prudden, Joao Costa and Sai Kripa
Introduction[edit | edit source]
Cartilage is a non-vascular type of supporting connective tissue that is found throughout the body . It is a firm tissue but softer and more flexible than bone .[1] It can be found in the larynx, respiratory tract, external ear, and in the articulating surfaces of joints. In babies many of the bones that form the skeleton are made primarily of cartilage, as children develop this cartilage will be replaced by bone.
Cartilage Structure [edit | edit source]
Cartilage is a dense structure, that resembles a firm gel, made up of collagen and elastic fibres. It contains polysacchride derivaites called chondroitin sulfates which complex with protein in the ground substance forming proteoglycan. The matrix is produced by cells call chrondroblasts which form chrondocytes and can be found in small chambers called lacuna
Cartilage separated from the surrounding tissues by perichondrium which consist of two layers:
- Outer Fibrous Layer : Which provide protection , mechanical support and attaches the cartilage to other structures.
- Inner Cellular : It Is Important in the growth and maintenance of cartilage .[3]
Types of Cartilage[edit | edit source]
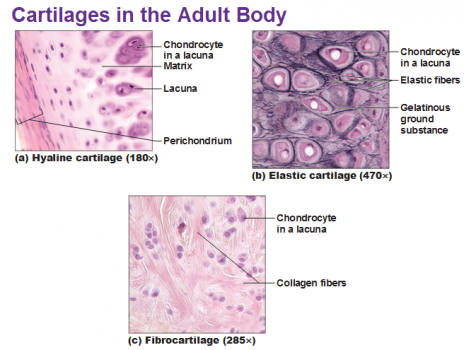
There are three types of cartilage and they all have slightly different structures and function
Hyaline Cartilage[edit | edit source]
Hyaline Cartilage has a smooth surface and is the most common of the three types of cartilage. It has a matrix that contains closely packed collagen fibers, making it tough but slightly flexible. It consists of a bluish-white, shiny ground elastic material, whose matrix contains chondtoitin sulphate, with many fine collagen fibrils and chrondrocytes. Because of its smooth surfaces it allows tissues to slide/glide more easily, as well as providing flexibility and support
Example : Connection between ribs and sternum, nasal cartilage and articular cartilage (which covers opposing bone surfaces in many joints).
Fibrocartilage[edit | edit source]
Fibrocartilage is the toughest of the three types of cartilage. It has no perichondrium and has a matrix that contains dense bundles of collagen fibers embedded with chrondrocytes, making it durable and tough. This makes it perfect to provide support and rigidity
Example : Intervertebral discs (between spinal vertebrae), Menisci (cartilage pads of the knee joint), the callus (formed at the ends of bones at the site of a fracture), between the Pubic Symphysis and at the junction where tendons insert into bone.
Elastic Cartilage[edit | edit source]
Elastic cartilage provides support. It has a yellowish colour and is surrounded by a perichnodrium. Chrondrocytes are located between a network of threadlike elastic fibres, the abundance of elastic fibres makes it flexible and resilient.
Example : the auricle of the outer ear .
Cartilage Growth [edit | edit source]
The growth of cartilage is a slow process and occurs by the division of cells. Both intersitial and appositional growth occur during development but neither of them occur in normal adult but under unusual circumstances appositional growth may occur as in cartilage damage (minor damage) .[3]
Interstitial Growth[edit | edit source]
Chondrocytes responsible for cell division and daughter cells produce the matrix. This occurs during embryonic level and continues until adolescence.
Appostional Growth[edit | edit source]
Cells of inner layer of perichondrium undergo division and inner most cells differentiate into immature chondrocytes which produce the matrix, they then mature into mature chondrocytes .
Remodelling of Cartilage[edit | edit source]
This occurs predominantly by changes and the rearrangement of the collagen matrix in response to load.
Mechanical Behaviour of Articular Cartilage[edit | edit source]
The mechanical behaviour depend on interaction of its component : proteoglycan , collagen and interstitial fluid. In an aqoues environment , proteogylcans are polyanionic which means the molecule has negatively charged sites that arise from sulfate and carboxyl. In solution, the mutual repulsion of these negative charges causes the aggregated proteogylcan to spread out and occupy a large volume .
In the cartilage matrix, the volume occupied by proteogylcan aggregates is limited by the network of collagen fibres. when the cartilage is commpressed the negatively charged sites are pushed together increasing the mutual repulsion force adding to the compressive stiffness of the cartilage. During this process non-aggregated protoegylcans are not affected by the compressive load since they are not easily trapped in the cartilage matrix .Damage to the collagen framework reduces compressive stiffness .
The mechanical response of the cartilage is strongly tied to the application of pressure differences and the flow of fluid through the tissue as, when deformed, the fluid flows across the cartilage and articular surface .
Biphasic model of cartilage[edit | edit source]
All of the solid components of the cartilage (lipid, proteogylcans,cells and collagen ) are grouped together to form the solid component of the matrix and the interstitial fluid, that moves freely, forms the fluid component.
Exercise and Cartilage Health[edit | edit source]
Participation in certain sports appear to increase risk of osteoarthritis (result from breakdown of joint cartilage). Activities that involve torsional loading , fast acceleration and deceleration , repetitive high impact and high level of participation increase risk of osteoarthritis. Increased risks of osteoarthritis are related to excessive exercise or abnormal joint loading But some levels of loading and exercise are beneficial for joint health as exercise enhances production of matrix molecules, which can have a positive effect on joint health. Therefore exercise has both beneficial and detrimental effects on cartilage. Exercise can promote positive biomechanical changes, reduce pain and increase function of people with arthritis but it must be noted that sports injuries can be a contributing factor to developing osteoarthritis .[5]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ http://www.news-medical.net/health/What-is-Cartilage.aspx
- ↑ https://www.youtube.com/watch?v=mr5JI8Q8dc8
- ↑ 3.0 3.1 3.2 Fredric H.Martini ,Judi Nath ,Edwen Bartholomew , Charles M.Seiger ,Damian Hill . Fundamentals of Anatomy and Physiology .9th ed , 2011 .
- ↑ https://www.youtube.com/watch?v=tS5S8BoVN-4
- ↑ 5.0 5.1 Carol A.Oatis . kinesiology the mechanics and pathomechanics of human movement , 2003 .