Cervical Instability: Difference between revisions
Pieter Piron (talk | contribs) No edit summary |
Pieter Piron (talk | contribs) No edit summary |
||
| Line 17: | Line 17: | ||
Cervical instability describes a wide range of conditions from neck pain and deformation without any clear proof over little malformations too complete failure of intervertebral connection<sup>15</sup>. White et al (1975)<sup>16 </sup>described cervical stability as: Cervical spine instability is defined as the loss of ability of cervical spine under physiological loads to maintain relationships between vertebrae in such a way, that spinal cord or nerve roots are not damaged or irritated and deformity or pain does not develop.<br> | Cervical instability describes a wide range of conditions from neck pain and deformation without any clear proof over little malformations too complete failure of intervertebral connection<sup>15</sup>. White et al (1975)<sup>16 </sup>described cervical stability as: Cervical spine instability is defined as the loss of ability of cervical spine under physiological loads to maintain relationships between vertebrae in such a way, that spinal cord or nerve roots are not damaged or irritated and deformity or pain does not develop.<br> | ||
== Clinically Relevant Anatomy | == Clinically Relevant Anatomy<br> == | ||
The cervical spine consist of 7 separate vertebrae. The first two vertebrae (referred as upper cervical spine) are highly specialized and differ from the other 5 cervical vertebrae (lower cervical) regarding anatomical structure and function.<br>The upper cervical spine is made of the atlas (C1) and the axis (C2). It comprises of two joint structures: one in between os occipital and atlas (atlanto-occipital joint), the other one between atlas and axis, which forms the atlanto-axial joint. The atlantoaxial joint is responsible for 50% of all cervical rotation; the atlanto-occipital joint is responsible for 50% of flexion and extension. <sup>8</sup><br>The craniocervical junction (atlanto-occipital joint), the lower atlanto-axial joint and other cervical segments are reinforced by internal as well as external ligaments. They secure the spinal stability of the cervical spine as a whole, together with surrounding postural muscles and allow cervical motion. They also provide proprioceptive information throughout the spinal nerve system to the brain. <br>Articulations include disk-vertebral body articulations, uncovertebral joints, and facet joints. The disk is thicker anteriorly as wel as its nearby ligamentous structures, contributing to normal cervical lordosis. The facet joints are oriented at a 45º angle to the axial plane, allowing a sliding motion; the joint capsule is weakest posteriorly. Supporting ligamentum flavum, posterior, and interspinous ligaments strengthen the posterior column but are thinner and therefore more fragile. <sup>9,10</sup><br>The remaining 5 vertebrae form the lower cervical spine, C3-C7, are similar to each other but differ from the upper cervical spine as mentioned before. <sup>11</sup><br><br> | |||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Revision as of 18:54, 26 June 2013
Original Editor - Mary-Kate McCoy and Heather Lampe as part of the Temple University EBP Project
Top Contributors - Vanbeylen Antoine, Mary-Kate McCoy, Rachael Lowe, Admin, Pieter Piron, Sara Evenepoel, David Herteleer, Kim Jackson, Lucinda hampton, Heather Lampe, Laura Ritchie, Nick Van Doorsselaer, Daniele Barilla, Simisola Ajeyalemi, Tony Lowe, Scott A Burns, WikiSysop, 127.0.0.1, Jess Bell, Olajumoke Ogunleye, Beth Potter and Evan Thomas
Original Editors
Top Contributors - Vanbeylen Antoine, Mary-Kate McCoy, Rachael Lowe, Admin, Pieter Piron, Sara Evenepoel, David Herteleer, Kim Jackson, Lucinda hampton, Heather Lampe, Laura Ritchie, Nick Van Doorsselaer, Daniele Barilla, Simisola Ajeyalemi, Tony Lowe, Scott A Burns, WikiSysop, 127.0.0.1, Jess Bell, Olajumoke Ogunleye, Beth Potter and Evan Thomas
Search Strategy[edit | edit source]
cervical stabilization exercises, cervical instability, physical therapy, physiotherapy, treatment, anatomy, definition cervical instability
Definition/Description[edit | edit source]
Cervical instability describes a wide range of conditions from neck pain and deformation without any clear proof over little malformations too complete failure of intervertebral connection15. White et al (1975)16 described cervical stability as: Cervical spine instability is defined as the loss of ability of cervical spine under physiological loads to maintain relationships between vertebrae in such a way, that spinal cord or nerve roots are not damaged or irritated and deformity or pain does not develop.
Clinically Relevant Anatomy
[edit | edit source]
The cervical spine consist of 7 separate vertebrae. The first two vertebrae (referred as upper cervical spine) are highly specialized and differ from the other 5 cervical vertebrae (lower cervical) regarding anatomical structure and function.
The upper cervical spine is made of the atlas (C1) and the axis (C2). It comprises of two joint structures: one in between os occipital and atlas (atlanto-occipital joint), the other one between atlas and axis, which forms the atlanto-axial joint. The atlantoaxial joint is responsible for 50% of all cervical rotation; the atlanto-occipital joint is responsible for 50% of flexion and extension. 8
The craniocervical junction (atlanto-occipital joint), the lower atlanto-axial joint and other cervical segments are reinforced by internal as well as external ligaments. They secure the spinal stability of the cervical spine as a whole, together with surrounding postural muscles and allow cervical motion. They also provide proprioceptive information throughout the spinal nerve system to the brain.
Articulations include disk-vertebral body articulations, uncovertebral joints, and facet joints. The disk is thicker anteriorly as wel as its nearby ligamentous structures, contributing to normal cervical lordosis. The facet joints are oriented at a 45º angle to the axial plane, allowing a sliding motion; the joint capsule is weakest posteriorly. Supporting ligamentum flavum, posterior, and interspinous ligaments strengthen the posterior column but are thinner and therefore more fragile. 9,10
The remaining 5 vertebrae form the lower cervical spine, C3-C7, are similar to each other but differ from the upper cervical spine as mentioned before. 11
Epidemiology /Etiology[edit | edit source]
add text here
Characteristics/Clinical Presentation[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Diagnostic Procedures[edit | edit source]
add text here related to medical diagnostic procedures
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
add text here related to physical examination and assessment
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
add text here
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
Clinically Relevant Anatomy[edit | edit source]
The cervical spine is structurally distinguished by differences between the upper cervical spine (C1 and C2) and the lower cervical spine (C3-C7) segments. Anatomical and functional distinctions allow for differences in segmental mobility and movement direction. The upper cervical spine allows for a greater degree of rotation with some frontal and sagittal movement. In contrast, the lower cervical spine moves in flexion-extension and inclination-rotation.[1]
Upper Cervical Spine (C1-C2)
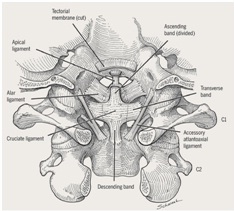
Figure 1:Posterior view of upper cervical
spine ligaments.[2]
Cervical instability is commonly associated with the upper cervical spine. Ghanem[1] proposes that the anatomical nature of the upper cervical spine creates an inherent instability. The alar and transverse ligaments provide the primary source of stability for the upper cervical spine. The transverse ligament is located across the arch of the atlas and positions the dens against the anterior arch of the atlas. Functionally, the transverse ligament limits flexion and provides support from anterior translation of C1.[3] If the transverse ligament is disrupted by injury or is congenitally lax, neural or vascular compromise could occur. This is due to the proximity of the spinal cord and vertebral arteries.[1] The alar ligaments connect the cranium to C1 from the sides of the dens to the lateral borders of the foramen magnum. The alar ligaments function to prevent excessive rotation at the atlanto-occipital joint.[4] The alar ligament is most commonly injured in motor vehicle accidents. However disruption of the alar ligament is less likely to lead to neurological or vascular injury.
Lower Cervical Spine (C3-C7)
In contrast to the upper cervical spine, the frontal plane orientation of facet joints of the lower cervical spine serves as the primary source of stability. In addition, spinal ligaments including ligamentum nuchae, anterior longitudinal ligament, posterior longitudinal ligament, and ligamentum flavum contribute to stability in the lower cervical spine.
Mechanism of Injury / Pathological Process[edit | edit source]
| [5] |
Traumatic:
- Whiplash
- Motor vehicle accident
- Head/neck surgery
Systemic:
- Recent upper respiratory infection
Congenital:
- Down syndrome
- Juvenile rheumatoid arthritis
- Ankylosing spondylosis
- Cerebral palsy
- Neurofibromatosis
- Os odontoideum
- Klippel-Feil syndrome (KFS)
Clinical Presentation[edit | edit source]
Mintken et al[2] described the cardinal symptoms of clinical instability: drop attacks, facial or lip paresthesias, bilateral or quadrilateral limb paresthesias, or nystagmus. These signs and symptoms are usually provoked with active or passive movement of the head or neck. Furthermore, in their case study, they address other secondary impairments such as dizziness and bilateral blurred vision.
In a Delphi survey study, Cook et al[6] reported that physical therapists attribute the following symptoms with cervical instability:
- “intolerance to prolonged static postures”
- “fatigue and inability to hold head up”
- "better with external support, including hands or collar"
- "frequent need for self-manipulation"
- "feeling of instability, shaking, or lack of control"
- "frequent episodes of acute attacks"
- "sharp pain, possibly with sudden movements"
Since there is little evidence supportive of clinical tests for cervical spine instability, recognition of these symptoms along with clinical judgment could warrant referral. During examination, it is important to collect a thorough history from the patient to understand the patient’s chief complaint, signs and symptoms - neural or vascular compromise, duration and pain level.
Diagnostic Procedures[edit | edit source]
| [7] |
Clinical Testing
In the literature, cervical spine instability consistently is described as being difficult to diagnose. Clinically, ligamentous tests to assess the stability of the upper cervical spine are limited by reliability, validity, and no consensus for sequencing of such tests. It is recommended to first assess with the Sharp-Pursor test, and then, only if it is negative, to proceed with other ligamentous tests in order of provocation (alar ligamentous stress then anterior shear test). Research remains inconclusive in what order it should be performed. Some authors feel as though if the Sharp-Pursor test is performed first, it can elicit a false negative response. Thus, if the patient does not experience a provocative test first, there would be a chance the patient’s symptoms would not be relieved by the Sharp-Pursor test. More research is required in this area to clarify the order and diagnostic accuracy for upper cervical spine instability testing.[2]
| Test |
Description |
Positive Test |
Diagnostic Accuracy |
| Sharp-Pursor Test |
|
Reduction in symptoms with and/or no sliding or “clunking” noted with PA movement. |
Sensitivity= 0.69 Specificity= 0.96 +LR= 17.3 -LR=0.32 |
| Alar Ligament Stress Test |
|
With passive movement of the head there is a lag or delay of C2 spinous process movement |
No available research |
| Anterior Shear Test ( Transverse Ligament Test) |
|
Sensation of lump in the throat or the presence of cardinal signs. |
No available research |
Diagnostic Imaging
Radiography is the primary diagnostic tool for cervical instability. Whenever possible, radiographs should be taken in sitting or standing to account for the effect of gravity and to capture an accurate picture of the normal curvature of the patient’s spine under physiological loading.[1] Radiographs should be taken in 3 views: anteroposterior, open-mouth anteroposterior, and lateral.[8]
Figure 2: Lateral cervical
radiograph with increased ADI.[9]
Standard anteroposterior radiographs provide visualization of the lower cervical spine, while open-mouth radiographs provide visualization of the upper cervical spine. Lateral radiographs allow for the measurement of the atlantodens interval (ADI), the space between the posterior surface of the anterior ring of the atlas and the anterior surface of the dens. An ADI greater than 3mm in adults or 5mm in children is indicative of atlantoaxial instability. In adults, an ADI of greater than 5mm typically indicates a rupture of the transverse ligament. However, in patient populations with chronic ligamentous laxity such as Rheumatoid Arthritis, Down Syndrome, or congenital abnormalties, the ADI measurement may not be as useful for diagnosing laxity of the transverse ligament. Such patients may present as asymptomatic. It is important to consider the increased risk associated with ligamentous laxity in these populations and to exercise caution in treatment.[10],[11]
Figure 3:Cervical MRI shows
increased ADI (13mm) displacing
dens and increasing pressure on
the spinal cord.[9]
Imaging procedures such as magnetic resonance imaging (MRI), functional MRI, computed tomography (CT) scanning, and dynamic fluoroscopy may be used when radiograph images are unclear or incomplete and/or for complex cases that require a detailed analysis of pathoanatomical structures or involve significant neurological deficits.[1],[12]
Outcome Measures[edit | edit source]
There are no patient reported outcome measures to specifically address cervical instability. However clinicians can address the patient’s reported impairments by administering the Numeric Pain Rating Scale (NPRS) and Neck Disability Index (NDI).
- Numeric Pain Rating Scale (NPRS)
- Neck Disability Index (NDI)
Management / Interventions
[edit | edit source]
Upon examination findings of positive ligamentous testing and clinically observable signs such as cardinal symptoms, a referral for imaging should be implemented. Depending on the mechanism of injury or the pathological origin of cervical spine instability, the mode for medical management varies. Ghanem[1] reports that treatments include surgical correction, immobilization or traction depending on the diagnosis of the patient’s case. Patients may benefit from conservative physical therapy interventions, especially those patients without severe ligamentous injury or neurovascular complications. Conservative therapy should focus on motor control retraining exercises for the cervical spine including the deep neck flexors. Manual therapy such as non-thrust manipulation and soft tissue mobilization could be considered to improve mobility of adjacent regions and for symptomatic relief. Aggressive manual techniques that would place strain through the compromised ligaments or cause neurovascular signs/symptoms are contraindicated.
| [13] | [14] |
| [15] | [16] |
Differential Diagnosis
[edit | edit source]
- Fracture
- Cervical myelopathy
- Vertebral basilar insufficiency
- Cervical spondylosis
- Torticollis
- Mechanical neck pain
- Headache
- TMJ dysfunction
Key Evidence
[edit | edit source]
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1jCKS3TQHK0hTn3Bsyq6VFHtRUtMFKIJ82pwIOvKx33U8QNsH4|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Ghanem I, El Hage S, Rachkidi R, Kharrat K, Dagher F, Kreichati G. Pediatric cervical spine instability. J Child Orthop. 2008 Mar;2(2):71-84.
- ↑ 2.0 2.1 2.2 2.3 Mintken PE, Metrick L, Flynn TW. Upper cervical ligament testing in a patient with os odontoideum presenting with headaches. J Orthop Sports Phys Ther. 2008 Aug;38(8):465-75.
- ↑ Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452-61.
- ↑ Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th ed. Baltimore: Lippincott Williams &amp;amp;amp;amp;amp;amp;amp;amp;amp; Wilkins;2005.
- ↑ CDRB90067. Mechanism of Injury Animation. Available from: http://www.youtube.com/watch?v=b5Bv_gtPu-8 [last accessed 09/03/13]
- ↑ Cook C, Brismée JM, Fleming R, Sizer PS Jr. Identifiers suggestive of clinical cervical spine instability: a Delphi study of physical therapists. Phys Ther. 2005 Sep;85(9):895-906.
- ↑ Kent Verdon. Ax 4 Special tests Cervical stability Sharp Purser, Alar, tectorial . Available from: http://www.youtube.com/watch?v=EfTLwlMqJfI [last accessed 09/03/13]
- ↑ Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR. 1990; 155:465-472.
- ↑ 9.0 9.1 Onerci M, Ogretmenoglu O, Ozcan OE. Atlantoaxial subluxation after tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg. 1997 Feb;116(2):271-3.
- ↑ Neva MH, Hakkinen A, Makinen H, Hannonen P, Kauppi M, Sokka T. High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann Rheum Dis. 2006;65:884-888.
- ↑ Ali FE, Al-Bustan MA, Al-Busairi WA, Al-Mulla FA, Esbaita EY. Cervical spine abnormalities associated with Down syndrome. International Orthopaedics (SICOT) 2006;30:284-289.
- ↑ Platzer P, Jaindl M, Thalhammer G, Dittrich S, Wieland T, Vecsel V, Gaebler C. Clearing the cervical spine in critically injured patients: a comprehensive c-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J. (2006); 15:1801-1810.
- ↑ OptimumCareProviders. 1.1 Deep Neck Flexor - Longus Colli Strengthening Level 1. Available from: http://www.youtube.com/watch?v=y4YTIhSBtxc [last accessed 09/03/13]
- ↑ OptimumCareProviders. 1.2 Deep Neck Flexor - Longus Colli Strengthening Level 2. Available from: http://www.youtube.com/watch?v=1smVSuQiQx8 [last accessed 09/03/13]
- ↑ OptimumCareProviders. 1.3 Deep Neck Flexor - Longus Colli Strengthening Level 3. Available from: http://www.youtube.com/watch?v=HHR6vi5uLDw [last accessed 09/03/13]
- ↑ OptimumCareProviders. 1.4 Deep Neck Flexor - Longus Colli Strengthening Level 4. Available from: http://www.youtube.com/watch?v=AAwPnN9BwSw [last accessed 09/03/13]