Cervical Stenosis: Difference between revisions
Rachael Lowe (talk | contribs) mNo edit summary |
Rachael Lowe (talk | contribs) mNo edit summary |
||
| Line 16: | Line 16: | ||
| [[Image:Cervica-Stenosis.jpg|thumb|center|Cervical stenosis]] | | [[Image:Cervica-Stenosis.jpg|thumb|center|Cervical stenosis]] | ||
|} | |} | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Epidemiological data give an incidence of 1:100 000 cervical spine stenosis cases<br><br>Cervical spine stenosis most commonly causes cervical myelopathy in 50+ aged patients<ref name=":5">João Levy M., António Fernandes F., João Lobo A. “Neurologic aspects of systemic disease part I.” Handbook of clinical neurology: Chapter 35- Spinal Stenosis (2014) Volume 119; pg 541-549</ref> | |||
<br>Cervical stenosis can be defined as 1. Functional stenosis or 2. Organic stenosis. <br> | |||
=== Functional Stenoses'''<ref name=":6">Denaro V. “Stenosis of the cervical spine: causes, diagnosis, treatment” (1991) Springer- verlag Berlin Heidelberg. Pg. 6-26.</ref>''' === | |||
(There will be a kinetic change. The stenosis causes a change in function, physiological and or biomechanical.)<br>- Degenerative pseudospondylollisthesis with arthrosis<br>- Mild post-traumatic laxity<br>- Ligamentous laxity <br>- kinetic overload of a segment<br>- loss of appropriate lordosis<br>- … | (There will be a kinetic change. The stenosis causes a change in function, physiological and or biomechanical.)<br>- Degenerative pseudospondylollisthesis with arthrosis<br>- Mild post-traumatic laxity<br>- Ligamentous laxity <br>- kinetic overload of a segment<br>- loss of appropriate lordosis<br>- … | ||
=== Organic Stenoses === | |||
(There will be a morphological and/ or anatomical change. The stenoses can be classified into congenital and more frequently, acquired stenoses.) <br>Classification of symptomatic spinal narrowing (organic stenosis):<br><u>A. Congenital</u><ref name=":5" /><ref name=":6" /> <br>(idiopathic)<br>o Malformations involving severe morphological deformity of the canal in the occipitocervical plane<br>o Malformations without serious structural distortion of the cervical canal<br>o Stenoses which result from systemic congenital disease which become manifest during growth and development.<br>o … | (There will be a morphological and/ or anatomical change. The stenoses can be classified into congenital and more frequently, acquired stenoses.) <br>Classification of symptomatic spinal narrowing (organic stenosis):<br><u>A. Congenital</u><ref name=":5" /><ref name=":6" /> <br>(idiopathic)<br>o Malformations involving severe morphological deformity of the canal in the occipitocervical plane<br>o Malformations without serious structural distortion of the cervical canal<br>o Stenoses which result from systemic congenital disease which become manifest during growth and development.<br>o … | ||
<u>B. Acquired</u><ref name=":6" /><br>There are multiple etiological factors:<br>o Degenerative processes<br>o Destructive processes<br>o Traumatic processes<br>o Arthritic conditions<br>o Iatrogenic causes | <u>B. Acquired</u><ref name=":6" /><br>There are multiple etiological factors:<br>o Degenerative processes<br>o Destructive processes<br>o Traumatic processes<br>o Arthritic conditions<br>o Iatrogenic causes | ||
Degenerative stenosis<br>Spinal arthrosis (degenerative disk disease)<br>- Destructive stenosis<br>Stenosis associated with neoplasm<br>- Inflammatory stenosis<br>- Traumatic stenosis<br>This clinical situation is a result of a trauma to the cervical spine. <br>It can progress to an imbalance between the cord and the cervical spinal canal.<br>- Iatrogenic stenosis<br>= cervical stenosis as a complication of surgery in the neck or/and spine.<br> -> Instability resulting from extensive laminectomy<br> -> Peridural postoperative fibrosis <br> -> …<br><br> | |||
== Characteristics/Clinical Presentation == | |||
Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated [[Cervical Radiculopathy|cervical radiculopathy]] or [[Cervical Myelopathy|cervical myelopathy]]. <br> | Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated [[Cervical Radiculopathy|cervical radiculopathy]] or [[Cervical Myelopathy|cervical myelopathy]]. <br> | ||
| Line 67: | Line 47: | ||
*Diminished proprioception | *Diminished proprioception | ||
The progression of the symptoms may also vary: | The progression of the symptoms may also vary in the following ways: | ||
*A slow and steady decline | *A slow and steady decline | ||
*Progression to a certain point and stabilizing | *Progression to a certain point and stabilizing | ||
*Rapidly declining | *Rapidly declining | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* | * Diabetes | ||
* | * Inflammatory spondyloarthropathy (e.g., ankylosing spondylitis) | ||
* | * Paget's disease of the bone | ||
* | * Peripheral neuropathy (paralysis) | ||
* | * Peripheral vascular disease | ||
* | * Single level lumbar disc herniation | ||
* | * Spinal cord tumor | ||
* | * Vascular insufficiency (atherosclerosis of the aorta and/or leg arteries) | ||
* Vertebral disc disease | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 126: | Line 107: | ||
Posterior approaches:<br> | Posterior approaches:<br> | ||
*Laminectomy without fusion or with instrumented fusion: This is a procedure where the bone and ligaments that are pressing against the spinal cord are removed. In this treatment the surgeon might add also a fusion to stabilize the spine<ref name=":0" />. | *Laminectomy without fusion or with instrumented fusion: This is a procedure where the bone and ligaments that are pressing against the spinal cord are removed. In this treatment the surgeon might add also a fusion to stabilize the spine<ref name=":0">L.Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fort he Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132</ref>. | ||
*Laminoplasty<ref name=":0" /><ref name=":1">.Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014</ref> | *Laminoplasty<ref name=":0" /><ref name=":1">.Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014</ref> | ||
Revision as of 11:52, 10 September 2017
Original Editors - Demol Yves as part of the Vrije Universiteit Brussel Evidence-based Practice Project
Top Contributors - Demol Yves, Rachael Lowe, Lucinda hampton, Sara Evenepoel, Kim Jackson, WikiSysop, Nicolas Casier, Simisola Ajeyalemi, Rucha Gadgil, Admin, Daphne Jackson, David Herteleer, Jess Bell, Olajumoke Ogunleye, Tony Lowe and Evan Thomas
Definition/Description[edit | edit source]
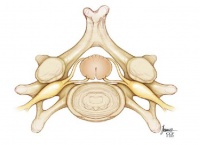
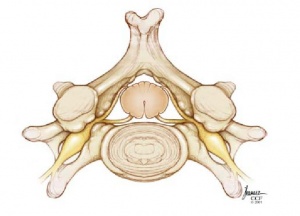
Cervical stenosis is a narrowing of the cervical spinal canal. This narrowing of the spinal canal may result in compression of the spinal cord and/or the nerve roots and affect the function of the spinal cord or the nerve, which may cause symptoms associated with cervical radiculopathy or cervical myelopathy.
Spinal stenosis may occur as a result of spondylosis (degenerative changes in the cervical spine) but can also be the result of traumatic (fractures and instability) and inflammatory conditions or caused by herniated discs or tumours.
Clinically Relevant Anatomy[edit | edit source]
Epidemiology /Etiology[edit | edit source]
Epidemiological data give an incidence of 1:100 000 cervical spine stenosis cases
Cervical spine stenosis most commonly causes cervical myelopathy in 50+ aged patients[1]
Cervical stenosis can be defined as 1. Functional stenosis or 2. Organic stenosis.
Functional Stenoses[2][edit | edit source]
(There will be a kinetic change. The stenosis causes a change in function, physiological and or biomechanical.)
- Degenerative pseudospondylollisthesis with arthrosis
- Mild post-traumatic laxity
- Ligamentous laxity
- kinetic overload of a segment
- loss of appropriate lordosis
- …
Organic Stenoses[edit | edit source]
(There will be a morphological and/ or anatomical change. The stenoses can be classified into congenital and more frequently, acquired stenoses.)
Classification of symptomatic spinal narrowing (organic stenosis):
A. Congenital[1][2]
(idiopathic)
o Malformations involving severe morphological deformity of the canal in the occipitocervical plane
o Malformations without serious structural distortion of the cervical canal
o Stenoses which result from systemic congenital disease which become manifest during growth and development.
o …
B. Acquired[2]
There are multiple etiological factors:
o Degenerative processes
o Destructive processes
o Traumatic processes
o Arthritic conditions
o Iatrogenic causes
Degenerative stenosis
Spinal arthrosis (degenerative disk disease)
- Destructive stenosis
Stenosis associated with neoplasm
- Inflammatory stenosis
- Traumatic stenosis
This clinical situation is a result of a trauma to the cervical spine.
It can progress to an imbalance between the cord and the cervical spinal canal.
- Iatrogenic stenosis
= cervical stenosis as a complication of surgery in the neck or/and spine.
-> Instability resulting from extensive laminectomy
-> Peridural postoperative fibrosis
-> …
Characteristics/Clinical Presentation[edit | edit source]
Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated cervical radiculopathy or cervical myelopathy.
Potential symptoms may include:[3][4][5]
- Pain in neck or arms
- Arm and leg dysfunction
- Weakness, stiffness or clumsiness in the hands
- Leg weakness
- Difficulty walking
- Frequent falling
- The need to use a cane or walker
- Urinary urgency which may progress to bladder and bowel incontinence
- Diminished proprioception
The progression of the symptoms may also vary in the following ways:
- A slow and steady decline
- Progression to a certain point and stabilizing
- Rapidly declining
Differential Diagnosis[edit | edit source]
- Diabetes
- Inflammatory spondyloarthropathy (e.g., ankylosing spondylitis)
- Paget's disease of the bone
- Peripheral neuropathy (paralysis)
- Peripheral vascular disease
- Single level lumbar disc herniation
- Spinal cord tumor
- Vascular insufficiency (atherosclerosis of the aorta and/or leg arteries)
- Vertebral disc disease
Diagnostic Procedures[edit | edit source]
Physical examination: [3][4][5][6]
- Hyper-reflexia: Increased reflexes in the knee and ankle
- Changes in gait, such as clumsiness or loss of balance
- Loss of sensitivity in the hands or feet
- Rapid foot beating that is triggered by turning the ankle upward
- Babinski’s sign
- Hoffman’s sign
X-rays of the cervical spine do not provide enough information to confirm cervical stenosis, but can be used to rule out other conditions. Cervical stenosis can occur at one level or multiple levels of the spine, therefore an MRI is useful for looking at several levels at one time. A detailed MRI image may also be useful to show the tight spinal canal and pinching of the spinal cord. A CT scan can provide information about the bony invasion of the canal and can be combined with myelography. [3][4]
Outcome Measures[edit | edit source]
- CT and MRI
Computed tomography (CT) and magnetic resonance imaging (MRI) can give a better image and understanding of the cervical spine. Specific and accurate measurements of the canal are important. CT and MRI is used for much better visualization. Space between the meningoneural structures in the canal to the size of the canal= consequence of stenosis[7].
These techniques make it possible to study the canal in three dimensions, the diameter, volume, the peringeal space and the state of the cord (morphometric features) without biopsy or sampling [7]
With the CT, classification of acquired stenoses will be based on the pattern of protusion of the calcification of the ligament into the spinal canal[8].
- It is difficult to identify this pathology with physical examination.
See Outcome Measures Database for more
Medical Management
[edit | edit source]
For patients presenting with increasing weakness, pain or instability with walking, surgical management of cervical spine stenosis may be considered.
Options for decompressing multilevel stenosis involve:
Anterior approaches:
- Anterior cervical discectomy with fusion
- Anterior cervical corpectomy with fusion
- Combination of both[3]Level of Evidence 2B
The disc or bone material( or both) that are causing spinal cord compression are removed from the anterior aspect and the spine is stabilized. The stabilizing of the spine, which is called fusion, involves placing an implant between the two cervical segments to support the spine and compensate for the bone and the disc that has been removed.
Posterior approaches:
- Laminectomy without fusion or with instrumented fusion: This is a procedure where the bone and ligaments that are pressing against the spinal cord are removed. In this treatment the surgeon might add also a fusion to stabilize the spine[9].
- Laminoplasty[9][10]
The posterior approach relies on the decompression by both the direct removal of offending posterior structures and indirect posterior translation of the spinal cord; thus, patients should undergo maintenance of lordosis or correctable kyphosis to permit adequate indirect decompression.
The distinction between these two types operations, depends on the location of the cord compression, number of levels involved, sagittal alignment, instability, associated axial neck pain, and risk factors for pseudarthrosis.
Laminoplasty is more effective to laminectomy without fusion because it decreases perineural adhesion and late kyphosis. The anterior techniques as well as the laminectomy with fusion are less effective than the laminoplasty. The laminoplasty preserves motion segments and prevents fusion-related complications, including bone graft dislodgement, pseudarthrosis, and adjacent segment disease[11][9].
After the surgery, the patient has to remain in the hospital for several days. A postoperative rehabilitation program may be provided, so that the patient can return to his activities and his typical daily function. This program consisted of an early post-operative ROM exercise, with or without a neck-collar[12].
Physical Therapy Management
[edit | edit source]
Nonoperative treatments, such as physical therapy management, are aimed at reducing pain and increasing the patient's function. Nonoperative treatments do not change the narrowing of the spinal canal, but can provide the patient of a long-lasting pain control and improved function without surgery. A rehabilitation program may require 3 or more months of supervised treatment. [3]
The purpose of physical therapy is to decrease pain and allow you to. Non-operative treatments, such as physical therapy management, are aimed at reducing pain and increasing the patient's functioning by gradually returning to normal activities Non-operative treatments do not change the narrowing of the spinal canal but may reduce pain in the soft tissues (such as the muscles, ligaments, and tendons), improve function, and build muscle strength. but can provide the patient of a long-lasting pain control and improved function without surgery. A rehabilitation program may require 3 or more months of supervised treatment. Non-surgical treatement involves physical or mechanical means, such as through exercise or heat. A physical therapist provides these treatments and will also provide education, instruction, and support for recovery[14][15][16].
A physical therapy program may include:
• Stretching exercises: These exercises are aimed at restoring the flexibility of the muscles of the neck, trunk, arms and legs. To also reduce stress on joints
• Manual therapy: Cervical and thoracic joint manipulation to improve or keep range of motion
• Heat therapy : to improve blood circulation to the muscles and other soft tissues.
• Cryotherapy : to help relieve pain
• Cardiovascular exercises for arms and legs: This will improve blood circulation and enhance the patient's cardiovascular endurance and promote good physical conditioning
• Aquatic exercises: to allow your body to exercise without pressure on the spine
• Training of activity of daily living (ADL) and functional movements.
Exercises and techniques that may help relieve symptoms of spinal stenosis and prevent progression of the condition include[10][15][16]:
• Specific strengthening exercises for the arm, trunk and leg muscles.
• stretching
• Postural re-education
• Scapular stabilization
• Ergonomics and frequent changes of position, to avoid sustained postures that compress the spine
• Planning ahead so that you take breaks in between potentially back-stressing activities such as walking and yard work.
• Proper lifting, pushing, and pulling.
P.S. some of the exercises are similar to the other forms of spinal stenose such as lumbale stenosis : lumbar spinal stenose
www.physio-pedia.com/Lumbar_spinal_stenosis
References[edit | edit source]
- ↑ 1.0 1.1 João Levy M., António Fernandes F., João Lobo A. “Neurologic aspects of systemic disease part I.” Handbook of clinical neurology: Chapter 35- Spinal Stenosis (2014) Volume 119; pg 541-549
- ↑ 2.0 2.1 2.2 Denaro V. “Stenosis of the cervical spine: causes, diagnosis, treatment” (1991) Springer- verlag Berlin Heidelberg. Pg. 6-26.
- ↑ 3.0 3.1 3.2 3.3 3.4 North American Spine Society Public Education Series. Cervical stenosis and myelopathy. http://www.spine.org/Documents/cervical_stenosis_2006.pdf (Accessed 22 November 2011).
- ↑ 4.0 4.1 4.2 Williams SK, et al. Concomitant cervical and lumbar stenosis: Strategies for treatment and outcomes. Semin Spine Surg 2007;19(3):165-176.
- ↑ 5.0 5.1 Countee RW, et al. Congenital stenosis of the cervical spine: Diagnosis and management. J Natl Med Assoc 1979;71(3):257-264.
- ↑ Santhosh A, et al. Spinal stenosis: history and physical examination. Phys Med Rehabil Clin N Am 2003;14.
- ↑ 7.0 7.1 Aboulker J, Metzger J, David M., Engel P., Ballivet J. (1965) Les myèlopathies cervicales d’origine rachidienne. Neurochirurgie 11: 89-198.
- ↑ Hashizume Y, Lijima S, Kishimoto H, et al. “Pathology of spinal cord lesions caused by ossification of the posterior longitudinal ligament.” (1984) Acta neuropathol (Berlin) 63: 123-130.
- ↑ 9.0 9.1 9.2 L.Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fort he Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132
- ↑ 10.0 10.1 .Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014
- ↑ H. Chikuda et Al., Optimal treatment for Spinal Cord Injury associated with Cervical canal Stenosis( OSCIS): a study protocol for a randomized controlled trial comparing early verus delayed surgery, BioMed Central, 2013.
- ↑ Y. Yukawa et Al., Laminoplasty and Skip Laminoplasty for Cervical Compressive Myelopathy, Spine, 2007
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedp9 - ↑ May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20
- ↑ 15.0 15.1 Hu SS, et al. Cervical spondylosis section of Disorders, diseases, and injuries of the spine. In HB Skinner, ed., Current Diagnosis and Treatment in Orthopedics, 4th ed., pp. 238–242. New York: McGraw-Hill.,2006
- ↑ 16.0 16.1 Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443:198.