Cervical Stenosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 69: | Line 69: | ||
*Cervical vertebral compression fracture | *Cervical vertebral compression fracture | ||
*Cervical spine facet syndrome | *Cervical spine facet syndrome | ||
*[[Cervical Osteoarthritis|Osteoarthritis]] of intervertebral joints in cervical spine<br> | *[[Cervical Osteoarthritis|Osteoarthritis]] of intervertebral joints in cervical spine<br> | ||
*Cervical spondylotic myelopathy <sup>[8]Level of evidence 5 [2]Level of evidence 5</sup><br> | *Cervical spondylotic myelopathy <sup>[8]Level of evidence 5 [2]Level of evidence 5</sup><br> | ||
*Osteophytes<br> | *Osteophytes<br> | ||
*Buckled, thickened, or ossified ligamentum flavum<br> | *Buckled, thickened, or ossified ligamentum flavum<br> | ||
*Hypertrophy or ossification of the posterior longitudinal ligament<sup>[3]Level of Evidence 2B [17] Level of evidence 2B</sup><br><br> | *Hypertrophy or ossification of the posterior longitudinal ligament<sup>[3]Level of Evidence 2B [17] Level of evidence 2B</sup><br><br> | ||
| Line 99: | Line 99: | ||
== Medical Management <br> == | == Medical Management <br> == | ||
For patients presenting with increasing weakness, pain or instability with walking, surgical management of cervical spine stenosis may be considered. | For patients presenting with increasing weakness, pain or instability with walking, surgical management of cervical spine stenosis may be considered. | ||
Options for decompressing multilevel stenosis involve: | Options for decompressing multilevel stenosis involve: | ||
Anterior approaches: <br | Anterior approaches: <br> | ||
*Anterior cervical discectomy with fusion | |||
*Anterior cervical corpectomy with fusion | |||
*Combination of both<sup>[3]Level of Evidence 2B</sup> | |||
Posterior approaches:<br> | The disc or bone material( or both) that are causing spinal cord compression are removed from the anterior aspect and the spine is stabilized. The stabilizing of the spine, which is called fusion, involves placing an implant between the two cervical segments to support the spine and compensate for the bone and the disc that has been removed. | ||
Posterior approaches:<br> | |||
*Laminectomy without fusion or with instrumented fusion: This is a procedure where the bone and ligaments that are pressing against the spinal cord are removed. In this treatment the surgeon might add also a fusion to stabilize the spine.<sup>[3]Level of Evidence 2B</sup> | |||
*Laminoplasty <sup>[3] Level of Evidence 2B[5]Level of Evidence 2B</sup> | |||
The posterior approach relies on the decompression by both the direct removal of offending posterior structures and indirect posterior translation of the spinal cord; thus, patients should undergo maintenance of lordosis or correctable kyphosis to permit adequate indirect decompression. | The posterior approach relies on the decompression by both the direct removal of offending posterior structures and indirect posterior translation of the spinal cord; thus, patients should undergo maintenance of lordosis or correctable kyphosis to permit adequate indirect decompression. | ||
| Line 113: | Line 120: | ||
<br>The distinction between these two types operations, depends on the location of the cord compression, number of levels involved, sagittal alignment, instability, associated axial neck pain, and risk factors for pseudarthrosis. | <br>The distinction between these two types operations, depends on the location of the cord compression, number of levels involved, sagittal alignment, instability, associated axial neck pain, and risk factors for pseudarthrosis. | ||
Laminoplasty is more effective to laminectomy without fusion because it decreases perineural adhesion and late kyphosis. The anterior techniques as well as the laminectomy with fusion are less effective than the laminoplasty. The laminoplasty preserves motion segments and prevents fusion-related complications, including bone graft dislodgement, pseudarthrosis, and adjacent segment disease. <sup>[3]Level of Evidence 2B, | Laminoplasty is more effective to laminectomy without fusion because it decreases perineural adhesion and late kyphosis. The anterior techniques as well as the laminectomy with fusion are less effective than the laminoplasty. The laminoplasty preserves motion segments and prevents fusion-related complications, including bone graft dislodgement, pseudarthrosis, and adjacent segment disease. <sup>[3]Level of Evidence 2B, [4]Level of Evidence 1B</sup><br> | ||
After the surgery, the patient has to remain in the hospital for several days. A postoperative rehabilitation program may be provided, so that the patient can return to his activities and his typical daily function. This program consisted of an early post-operative ROM exercise, with or without a neck-collar. <sup>[17]Level of Evidence 2B</sup><br><br> | After the surgery, the patient has to remain in the hospital for several days. A postoperative rehabilitation program may be provided, so that the patient can return to his activities and his typical daily function. This program consisted of an early post-operative ROM exercise, with or without a neck-collar. <sup>[17]Level of Evidence 2B</sup><br><br> | ||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
| Line 131: | Line 138: | ||
*Training of activity of daily living (ADL) and functional movements. | *Training of activity of daily living (ADL) and functional movements. | ||
== Recent Related Research (from | == Key Research<br> == | ||
* L.Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fort he Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132.<sup>Level of Evidence 2B</sup><br> | |||
== Recourses<br> == | |||
* H. Chikuda et Al., Optimal treatment for Spinal Cord Injury associated with Cervical canal Stenosis( OSCIS): a study protocol for a randomized controlled trial comparing early verus delayed surgery, BioMed Central, 2013.[4]Level of Evidence 1B | |||
*May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20. (Level of Evidence 1A)<br><br> | |||
== Recent Related Research (from Pubmed)<br> == | |||
*The morphological and clinical significance of developmental cervical stenosis. (http://www.ncbi.nlm.nih.gov/pubmed/25813007?dopt=Abstract)<br> | |||
<div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1Ts-QavLxpnuWsp1ZwRckafOkjAdJlQ47-FHBQNQJU4WQ2OYiq|charset=UTF8|short|max=10</rss>
</div> | <div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1Ts-QavLxpnuWsp1ZwRckafOkjAdJlQ47-FHBQNQJU4WQ2OYiq|charset=UTF8|short|max=10</rss>
</div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
1) M.J. Lee et Al., Prevalence of Cervical Spine Stenosis, The journal of bone and joint surgery, 2007.<sup>[1]Level of Evidence 2C</sup><br>2) M. McDonnell et Al., Cervical Spondylosis, stenosis, and Rheumatoid Arthritis, Medicine & Health/Rhode Island, Vol.95, No.4, April 2012. <sup>[2]Level of Evidence 5</sup><br>3) L.Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fort he Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132.<sup>[3]Level of Evidence 2B</sup><br>4) H. Chikuda et Al., Optimal treatment for Spinal Cord Injury associated with Cervical canal Stenosis( OSCIS): a study protocol for a randomized controlled trial comparing early verus delayed surgery, BioMed Central, 2013.<sup>[4]Level of Evidence 1B</sup><br>5) K.Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014.<sup>[5]Level of Evidence 2B</sup><br>6) May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20. <sup>(Level of Evidence 1A)</sup><br>7) Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443:198. <sup>(level of evidence: 5)</sup><br>8) Hu SS, et al. Cervical spondylosis section of Disorders, diseases, and injuries of the spine. In HB Skinner, ed., Current Diagnosis and Treatment in Orthopedics, 4th ed., pp. 238–242. New York: McGraw-Hill.,2006 <sup>(level of evidence: 5)</sup><br>9) Li X, Li J, Wu X. “Incidence, risk factors and treatment of cervical stenosis after radical trachelectomy: A systematic review.” European Journal of Cancer (2015) Sep;51(13):1751-9. <sup>LoE: 1A</sup><br>10) Desai SK, et al. “Isolated cervical spinal canal stenosis at C-1 in the pediatric population and in Williams syndrome.” J Neurosurg Spine. 2013 Jun;18(6):558-63. LoE: <br>11) Aboulker J, Metzger J, David M., Engel P., Ballivet J. (1965) Les myèlopathies cervicales d’origine rachidienne. Neurochirurgie 11: 89-198. LoE:<br>12) Payne E., Spillane J. (1957) The cervical spine. An Anatomicopathological study of 70 specimens (using a special technique) with particular reference to the problem of cervical spondylosis. Brain 80: 571. LoE:<br>13) João Levy M., António Fernandes F., João Lobo A. “Neurologic aspects of systemic disease part I.” Handbook of clinical neurology: Chapter 35- Spinal Stenosis (2014) Volume 119; pg 541-549.<sup>LoE:5</sup><br>14) Denaro V. “Stenosis of the cervical spine: causes, diagnosis, treatment” (1991) Springer- verlag Berlin Heidelberg. Pg. 6-26. <sup>LoE: 5</sup><br>15) Boni M, Denaro V. “The cervical stenosis syndrome.” Int Ortho (1982) p:185-195. LoE: <br>16) Hashizume Y, Lijima S, Kishimoto H, et al. “Pathology of spinal cord lesions caused by ossification of the posterior longitudinal ligament.” (1984) Acta neuropathol (Berlin) 63: 123-130. <br>17) Y. Yukawa et Al., Laminoplasty and Skip Laminoplasty for Cervical Compressive Myelopathy, Spine, 2007.<sup>[17]Level of Evidence 2B</sup><br><br> | |||
<br> | <br> | ||
[[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Cervical_Conditions]] [[Category:Condition]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Cervical]] | [[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Cervical_Conditions]] [[Category:Condition]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Cervical]] | ||
<br> | |||
Revision as of 19:55, 11 June 2016
Original Editors - Demol Yves as part of the Vrije Universiteit Brussel Evidence-based Practice Project
Top Contributors - Demol Yves, Rachael Lowe, Sara Evenepoel, Lucinda hampton, Kim Jackson, WikiSysop, Admin, Daphne Jackson, David Herteleer, Nicolas Casier, Simisola Ajeyalemi, Rucha Gadgil, Olajumoke Ogunleye, Tony Lowe, Evan Thomas and Jess Bell
Definition/Description[edit | edit source]
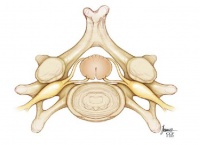
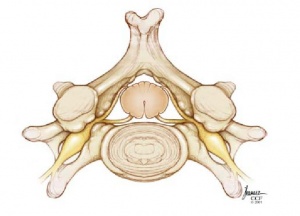
Cervical stenosis is defined by the narrowing of the vertebral canal, which may result in a compression on the spinal cord and/or the nerve roots. Especially narrowing of the sagittal diameter of the cervical spinal canal is of clinical importance in traumatic, degenerative and inflammatory conditions. Because of this narrowing, the function of the spinal cord or the nerve may be affected, which may cause symptoms associated with cervical radiculopathy or cervical myelopathy. Spinal stenosis, or narrowing of the spinal canal, may occur as a result of progression of spondylotic changes. [1]Level of Evidence 2C, [2]Level of Evidence 5
Clinically Relevant Anatomy[edit | edit source]
The cervical vertebrae are the smallest of the vertebrae, in comparison with the other spinal vertebrae. Their purpose is to contain and protect the spinal cord, support the skull, and enable diverse head movements. In general, the seven vertebrae of the vertebral spine are characterized by a large and triangular vertebral foramen and small foramina in the transverse processes (except C7) that allow vertebral arteries, veins and nerves to pass through.[1]
The ligaments of the cervical vertebrae guide the intra-articular movements in the most optimal directions in order to avoid cartilage damage and muscle hypertonicity. They also prevent excessive movements, which could otherwise lead to serious injuries. The ligamentum flavum is a broad, fibrous ligament that connects the laminae of adjacent vertebral arches. The elastic nature of the ligament helps to maintain the natural curvature of the spinal column and protects the intervertebral discs.[1]
The following muscles act on the cervical spine and help to maintain its balance and stability:
- Longus capitis
- Longus colli
- Spinalis cervicis
- Semispinalis capitis
There is also a group of muscles that acts to ensure that the head can move in all directions:
Epidemiology /Etiology[edit | edit source]
Cervical stenosis typically has an insidious onset. The condition is characterized by a narrowing of the spinal canal, nerve root canal, or foramen. Pathological changes to a range of tissues in the region could be at fault. Examples include soft tissue damage (such as disc protrusion or fibrotic scars), boney tissue damage (such as osteophyte formation or spondylolisthesis), or impaired postural mechanics. Narrowing of the canal causes compression of the spinal cord and nerves at the effected level, leading to neurological symptoms as the condition progresses.[2]
Characteristics/Clinical Presentation[edit | edit source]
Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated cervical radiculopathy or cervical myelopathy.
Potential symptoms may include:Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Pain in neck or arms
- Arm and leg dysfunction
- Weakness, stiffness or clumsiness in the hands
- Leg weakness
- Difficulty walking
- Frequent falling
- The need to use a cane or walker
- Urinary urgency which may progress to bladder and bowel incontinence
- Diminished proprioception
The progression of the symptoms may also vary:
- A slow and steady decline
- Progression to a certain point and stabilizing
- Rapidly declining
Differential Diagnosis[edit | edit source]
- Acute cervical disc herniation
- Cervical vertebral compression fracture
- Cervical spine facet syndrome
- Osteoarthritis of intervertebral joints in cervical spine
- Cervical spondylotic myelopathy [8]Level of evidence 5 [2]Level of evidence 5
- Osteophytes
- Buckled, thickened, or ossified ligamentum flavum
- Hypertrophy or ossification of the posterior longitudinal ligament[3]Level of Evidence 2B [17] Level of evidence 2B
Diagnostic Procedures[edit | edit source]
Physical examination: Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Hyper-reflexia: Increased reflexes in the knee and ankle
- Changes in gait, such as clumsiness or loss of balance
- Loss of sensitivity in the hands or feet
- Rapid foot beating that is triggered by turning the ankle upward
- Babinski’s sign
- Hoffman’s sign
X-rays of the cervical spine do not provide enough information to confirm cervical stenosis, but can be used to rule out other conditions. Cervical stenosis can occur at one level or multiple levels of the spine, therefore an MRI is useful for looking at several levels at one time. A detailed MRI image may also be useful to show the tight spinal canal and pinching of the spinal cord. A CT scan can provide information about the bony invasion of the canal and can be combined with myelography. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Outcome Measures[edit | edit source]
See Outcome Measures Database for more
Medical Management
[edit | edit source]
For patients presenting with increasing weakness, pain or instability with walking, surgical management of cervical spine stenosis may be considered.
Options for decompressing multilevel stenosis involve:
Anterior approaches:
- Anterior cervical discectomy with fusion
- Anterior cervical corpectomy with fusion
- Combination of both[3]Level of Evidence 2B
The disc or bone material( or both) that are causing spinal cord compression are removed from the anterior aspect and the spine is stabilized. The stabilizing of the spine, which is called fusion, involves placing an implant between the two cervical segments to support the spine and compensate for the bone and the disc that has been removed.
Posterior approaches:
- Laminectomy without fusion or with instrumented fusion: This is a procedure where the bone and ligaments that are pressing against the spinal cord are removed. In this treatment the surgeon might add also a fusion to stabilize the spine.[3]Level of Evidence 2B
- Laminoplasty [3] Level of Evidence 2B[5]Level of Evidence 2B
The posterior approach relies on the decompression by both the direct removal of offending posterior structures and indirect posterior translation of the spinal cord; thus, patients should undergo maintenance of lordosis or correctable kyphosis to permit adequate indirect decompression.
The distinction between these two types operations, depends on the location of the cord compression, number of levels involved, sagittal alignment, instability, associated axial neck pain, and risk factors for pseudarthrosis.
Laminoplasty is more effective to laminectomy without fusion because it decreases perineural adhesion and late kyphosis. The anterior techniques as well as the laminectomy with fusion are less effective than the laminoplasty. The laminoplasty preserves motion segments and prevents fusion-related complications, including bone graft dislodgement, pseudarthrosis, and adjacent segment disease. [3]Level of Evidence 2B, [4]Level of Evidence 1B
After the surgery, the patient has to remain in the hospital for several days. A postoperative rehabilitation program may be provided, so that the patient can return to his activities and his typical daily function. This program consisted of an early post-operative ROM exercise, with or without a neck-collar. [17]Level of Evidence 2B
Physical Therapy Management
[edit | edit source]
Nonoperative treatments, such as physical therapy management, are aimed at reducing pain and increasing the patient's function. Nonoperative treatments do not change the narrowing of the spinal canal, but can provide the patient of a long-lasting pain control and improved function without surgery. A rehabilitation program may require 3 or more months of supervised treatment. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A physical therapy or exercise program consists of the following exercises: Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Stretching exercises: These exercises are aimed at restoring the flexibility of the muscles of the neck, trunk, arms and legs.
- Cardiovascular exercises for arms and legs: This will improve blood circulation and enhance the patient's cardiovascular endurance.
- Specific strengthening exercises for the arm, trunk and leg muscles.
- Postural re-education
- Scapular stabilization
- Cervical and thoracic joint manipulation
- Training of activity of daily living (ADL) and functional movements.
Key Research
[edit | edit source]
- L.Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fort he Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132.Level of Evidence 2B
Recourses
[edit | edit source]
- H. Chikuda et Al., Optimal treatment for Spinal Cord Injury associated with Cervical canal Stenosis( OSCIS): a study protocol for a randomized controlled trial comparing early verus delayed surgery, BioMed Central, 2013.[4]Level of Evidence 1B
- May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20. (Level of Evidence 1A)
Recent Related Research (from Pubmed)
[edit | edit source]
- The morphological and clinical significance of developmental cervical stenosis. (http://www.ncbi.nlm.nih.gov/pubmed/25813007?dopt=Abstract)
References[edit | edit source]
1) M.J. Lee et Al., Prevalence of Cervical Spine Stenosis, The journal of bone and joint surgery, 2007.[1]Level of Evidence 2C
2) M. McDonnell et Al., Cervical Spondylosis, stenosis, and Rheumatoid Arthritis, Medicine & Health/Rhode Island, Vol.95, No.4, April 2012. [2]Level of Evidence 5
3) L.Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fort he Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132.[3]Level of Evidence 2B
4) H. Chikuda et Al., Optimal treatment for Spinal Cord Injury associated with Cervical canal Stenosis( OSCIS): a study protocol for a randomized controlled trial comparing early verus delayed surgery, BioMed Central, 2013.[4]Level of Evidence 1B
5) K.Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014.[5]Level of Evidence 2B
6) May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20. (Level of Evidence 1A)
7) Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443:198. (level of evidence: 5)
8) Hu SS, et al. Cervical spondylosis section of Disorders, diseases, and injuries of the spine. In HB Skinner, ed., Current Diagnosis and Treatment in Orthopedics, 4th ed., pp. 238–242. New York: McGraw-Hill.,2006 (level of evidence: 5)
9) Li X, Li J, Wu X. “Incidence, risk factors and treatment of cervical stenosis after radical trachelectomy: A systematic review.” European Journal of Cancer (2015) Sep;51(13):1751-9. LoE: 1A
10) Desai SK, et al. “Isolated cervical spinal canal stenosis at C-1 in the pediatric population and in Williams syndrome.” J Neurosurg Spine. 2013 Jun;18(6):558-63. LoE:
11) Aboulker J, Metzger J, David M., Engel P., Ballivet J. (1965) Les myèlopathies cervicales d’origine rachidienne. Neurochirurgie 11: 89-198. LoE:
12) Payne E., Spillane J. (1957) The cervical spine. An Anatomicopathological study of 70 specimens (using a special technique) with particular reference to the problem of cervical spondylosis. Brain 80: 571. LoE:
13) João Levy M., António Fernandes F., João Lobo A. “Neurologic aspects of systemic disease part I.” Handbook of clinical neurology: Chapter 35- Spinal Stenosis (2014) Volume 119; pg 541-549.LoE:5
14) Denaro V. “Stenosis of the cervical spine: causes, diagnosis, treatment” (1991) Springer- verlag Berlin Heidelberg. Pg. 6-26. LoE: 5
15) Boni M, Denaro V. “The cervical stenosis syndrome.” Int Ortho (1982) p:185-195. LoE:
16) Hashizume Y, Lijima S, Kishimoto H, et al. “Pathology of spinal cord lesions caused by ossification of the posterior longitudinal ligament.” (1984) Acta neuropathol (Berlin) 63: 123-130.
17) Y. Yukawa et Al., Laminoplasty and Skip Laminoplasty for Cervical Compressive Myelopathy, Spine, 2007.[17]Level of Evidence 2B