Cervicogenic Headache: Difference between revisions
No edit summary |
No edit summary |
||
| Line 318: | Line 318: | ||
[[Category:Cervical]] [[Category:EIM_Residency_Project]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Texas_State_University_EBP_Project]] | [[Category:Cervical]] [[Category:EIM_Residency_Project]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Texas_State_University_EBP_Project]] | ||
22. Bogduk N., The anatomical basis for cervicogenic headache, J Manipulative Physiol Ther p.67-70, 1992. Level of evidence: 1 | |||
Revision as of 20:22, 20 June 2013
Original Editor - Christopher Covert, Jeremy Brady, Mary Harris, Thomas Lawlor and Rick Wetherald as part of the Texas State University Evidence-based Practice Project
Top Contributors - Jeremy Brady, Admin, Sofie Van Cutsem, Kim Jackson, Nicolas D'Hondt, Mary Harris, Rick Wetherald, Rani Vetsuypens, Sanne Vanderhoeven, Joshua Samuel, Rachael Lowe, Tony Lowe, Laura Ritchie, Evan Thomas, 127.0.0.1, Simisola Ajeyalemi, Christopher Covert, Bram Sorel, Lucinda hampton, Jess Bell, Chelsea Mclene, Scott Buxton, Mathieu Van Durme1, WikiSysop, Vidya Acharya, Rucha Gadgil, Olajumoke Ogunleye and Rishika Babburu
Definition/Description[edit | edit source]
A chronic headache that arises from the atlanto-occipital and upper cervical joints and perceived in one or more regions of the head and/or face.[1] These occur due to a neck disorder or lesion and feature the converging of trigeminal and cervical afferents in the trigeminocervical nucleus within the upper cervical spinal cord.[2] By definition the headache should be abolished following a diagnostic blockade of a cervical structure or its nerve supply.[3]
The International Headache Society (IHS) has validated cervicogenic headache as a headache type that is hypothesized to originate due to nociception in the cervical area. [4]
Clinical relevant anatomy[edit | edit source]
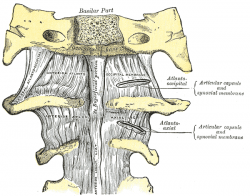
The cervical spine consists of 7 vertebrae, C1 to C7. The cervical nerves from C1 to C8. The first two vertebrae have a unique shape and function.3 The upper vertebrae supports the skull, articulates superiorly with the occiput (the atlanto-occipital joint) and is named the atlas (C1). This joint is responsible for 50% of flexion and extension.5 The design of the atlas allows forward and backward movement of the head. Among the atlas is the axis (C2) that allows rotation.3 The atlantoaxial joint is responsible for 50% of all cervical rotation. Both form the upper cervical spine. The 5 cervical vertebrae that make up the lower cervical spine, C3-C7, are similar to each other but very different from C1 and C2.5 (Figure 1)
Intervertebral discs are located between the vertebral bodies of C2-C7. These disks are composed of 4 parts: the nucleus pulposus in the middle, the annulus fibrosis surrounding the nucleus, and 2 end plates that are attached to the adjacent vertebral bodies. They serve as force dissipators, transmitting compressive loads throughout a range of motion. The disks are thicker anteriorly and therefore contribute to normal cervical lordosis. The intervertebral disks are involved in cervical spine motion, stability, and weight-bearing.5
The most important muscles that are totally or partially located cervical are:4 (figure3)
Erector spinae, upper Extension, rotation C1–T1
Longus capitis Flexion C1–C3
Longus colli Flexion C2–C6
Rectus capitis anterior Flexion C1–C2
Rectus capitis lateral Flexion C1–C2
Scalenes Flexion, rotation C4–C8
Semispinalis capitis Extension, rotation C1–T1
Semispinalis cervicis Extension, rotation C1–T1
Splenius capitis Extension, rotation C1–C8
Splenius cervicis Extension, rotation C1–C8
Sternocleidomastoid Flexion, rotation C2, XI
Trapezius, upper Extension, rotation C3-C4
Levator scapula Elevatie scapula C3-C5
Rhomboideus minor Retrotractie scapula + fixation C4-C5
The most important ligaments that are totally or partially located cervical are:4,5 (figure 2)
Alar Axis-skull head rotation & lateral flexion
Anterior atlantoaxial Axis & atlas extension
Posterior atlantoaxial Axis & atlas flexion
Ligamentum nuchae cervical flexion
Anterior longitudinal Axis-sacrum Extension
Posterior Longitudinal Axis-sacrum Flexion
Ligament flavum Axis-sacrum flexion
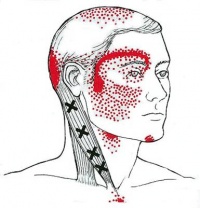
The mechanism which is responsible for the pain consists of a merger of the spinal nerves C1, C2 and C3, and a branch of the 5th cranial nerve, the n. trigeminal. This merger of nerves makes it possible that upper cervical pain radiate to regions of the head which are innervated by the cervical nerve (auricular and occipital). The merger with the trigeminal afferents allows the pain to radiate to the parietal, frontal and orbital regions.22,2,11
Epidemiology/Etiology[edit | edit source]
Of all chronic headaches, the incidence of cervicogenic headache has been estimated to be 14-18%,[5] though in a recent population-based study a 2.2% prevalence was found[6]. As such, it is important we can distinguish cervicogenic headache from the other headaches like migraine, tension type headache.
The term cervicogenic headache (CGH) was coined almost 3 decades ago, and the general condition of pain located in the head but originating in the cervical spine was described over 100 years ago. It is similar to other non-specific spinal conditions in its relative lack of high level evidence regarding pathoanatomical etiology. Since there is no objective test set for diffinitive diagnosis of CGH, the condition is ruled in, and treatment chosen, based on the patient's subjective report of pain patterns. [7]
There is some evidence that multiple structures in the upper cervical spine can be the source that is referring pain into the head. The implicated structures are generally centered around C1, C2, and C3 spinal levels. This may include the joints, disc, ligaments, and musculature.[8] The lower cervical spine may play an indirect role in pain production if dysfunctional, but there is no evidence of a direct referral pattern.[8] Through controlled nerve blocking of various structures in the cervical spine, it appears that the zygoapophyseal joints, especially those of C2/C3, are the most common sources of CGH pain. This finding is even more common in patients with a history of whiplash. [8]
Characteristics/Clinical Presentation[edit | edit source]
Challenging to diagnose clinically, but often includes the below:
- Unilateral “ram’s horn” or unilateral dominant headache[9]
- Excluding those with bilateral headache or symptoms that typify migrane headaches
- Exacerbated by neck movement or posture[9]
- Tenderness of the upper 3 cervical spine joints[9]
- Association with neck pain or dysfunction[10]
- Definitive diagnosis made through selective nerve blocking through injection of specific sites[8]
- Compared to migraine headache and control groups, cervicogenic headache group patients tend to have increased tightness of upper trapezius, levator scapulae, scales and suboccipital extensors[1]
Differential Diagnosis[edit | edit source]
| Type | Location | Intensity | Frequency | Duration | Additional Symptoms |
| Cluster | Unilateral: (orbital, supraorbital, temporal) | Severe | 1x every other day -> 8x day | 15-180 minutes | Associated with ipsilateral: conjunctival injection, lacrimation, nasal congestion, rhinorrhoea, forehead and facial sweating, miosis, ptosis, eyelid edema. Restlessness or agitation. |
| Tension | Bilateral | Mild-Moderate | >15day/mo, >3 mo | Hours-continuous |
Pressing, tightening <1 of photophobia, phonophobia or mild nausea |
| Migraine without aura | Unilateral: Frontotemporal in adults, Occipital in children | Moderate-Severe | >14 days/month |
4-72 hours | Flickering lights/spots in vision, pulsating quality, nausea, photophobia, phonophobia |
For more detailed classification information
| Cluster | Tension | Migrane |

|

|

|
Cybex Dynamometry[edit | edit source]
Another possibility to distinguish cervicogenic headache from migraine and tension headache is the use of a Cybex dynamometry.[11] Testing using Cybex dynamometry has shown that the ranges of cervical flexion, extension and rotation are significantly less in patients with cervicogenic than in patients with migraine and tension type headache (p < 0.001). Investigators also found that tenderness is a factor that varies between patients with CGH and patients with migraine or tension type headaches. Bovim measured pressure pain thresholds at ten points on the head and suboccipital region in patients with CGH, tension type headache and migraine.[12] Lower scores were found in patient with cervicogenic headaches than without.
Outcomes measures[edit | edit source]
-Neck_Disability_Index
-Headache Disability Index
-Northwick Park Neck Pain Questionnaire
-Numeric Pain Rating Scale
-Pain visual analog scale
-Headache frequency and duration
-Quantification of changes in headache pain intensity[12]
-Headache frequency[12]
-Self-reported function[12]
-Cervical ROM[13]
-Algometric pain thresholds[13]
Increased age, provocation or relief of headache with movement, employment status, and potentially duration of symptoms were associated with improved physical and functional outcomes after a standardized physical therapy intervention that included spinal mobilization and manipulation, as well as a home exercise program.[12]
Examination[edit | edit source]
Diagnostic Criteria (as described by the IHS)[3]:[edit | edit source]
- Pain localized in the neck and occiput, which can spread to other areas in the head, such as forehead, orbital region, temples,vertex, or ears, usually unilateral.
- Pain is precipitated or aggravated by specific neck movements or sustained postures.
- At least one of the following:
- Resistance to or limitation of passive neck movements
- Changes in neck muscle contour, texture, tone, or response to active and passive stretching and contraction
- Abnormal tenderness of neck musculature
- Radiological examination reveals at least one of the following:
- Movement abnormalities in flexion/extension
- Abnormal posture
- Fractures, congenital abnormalities, bone tumors, rheumatoid arthritis, or other distinct pathology (not spondylosis orosteochondrosis)
Flexion-Rotation Test Sn = 0.91, Sp = 0.90[13]
[edit | edit source]
The inverse relationship between headache severity of CGH and ROM towards the most restricted side for the Cervical Flexion-Rotation Test (FRT) was statistically significant for all patients with cervicogenic headaches.[13] The patient should feel no pain at the time of the test. During this test, the neck of the patient is passively held in end range flexion. The therapist rotates the neck to each side until they feel resistance or until the patient says they are in pain. At this end point, the therapist makes a visual estimate of the rotation range and says on which side the FRT was positive or negative. The test was positive when the estimated range was reduced by more than 10° from the anticipated normal range (44°).
"Red flags"[edit | edit source]
- Sudden onset of a new severe headache;
- A worsening pattern of a pre-existing headache in the absence of obvious predisposing factors;
- Headache associated with fever, neck stiff ness, skin rash, and with a history of cancer, HIV, or other systemic illness;
- Headache associated with focal neurologic signs other than typical aura;
- Moderate or severe headache triggered by cough, exertion, or bearing down; and
- New onset of a headache during or following pregnancy.
Patients with one or more red flags should be referred for an immediate medical consultation and further investigation.[13]
Medical Management (current best evidence)[edit | edit source]
The failure to conclusively demonstrate a specific disease or dysfunction of the neck in relation to cervicogenic headache has been an impediment to specific treatment for individuals with the diagnosis.
Cervical epidural steroid injections: Indicated for multilevel disc or spine degeneration
Nerve Blocks: Disrupting the cascade of signals leading to sensitization to central mechanisms via:
- Nerve blocks
- Trigger point injections
- Radiofrequency thermal neurolysis
Current best evidence suggests that there is not sufficient evidence meeting the EBM criteria to support the use of RF facet denervation for cervicogenic headaches.[14]
Surgical interventions: Often only provide temporary relief with the possibility of longer intensification of pain.[1] Procedures Include:
- Neurotomy
- Dorsal rhizotomy
- Microvascular decompression of nerve roots
Other Medications:
Tricyclic antidepressants - Used at lower dosage than required for pts diagnosed with depression
Muscle relaxants - Related to the CNS, may be beneficial, evidence is still pending
Botulinum toxin - A neurotoxin injected into tender muscles to reduce hypertonia
Physical Therapy Management (current best evidence)[edit | edit source]
The preferred practice pattern for cervicogenic headache is 5D: Impaired Motor Function and Sensory Integrity Associated with Nonprogressive Disorders of the Central Nervous System-Acquired in Adolescence or Adulthood. Goodman states that "Although this type of headache is responsive to therapy oriented at treating the soft tissue restrictions, the method of examination, assessment, and treatment needs to be specific to the neck and occiput."[1]
Treatment[edit | edit source]
- Cervical spine manipulation or mobilization[15]
- Strengthening exercises[15]
- Deep neck flexors
- Upper quarter muscles
- Thoracic spine thrust manipulation & exercise[16]
- C1-C2 Self-sustained Natural Apophyseal Glide (SNAG)[17]
- shown to be effective for reducing cervicogenic headache symptoms
- shown to be effective for reducing cervicogenic headache symptoms
Jull et al[9] reported that a six week physiotherapy program including manual therapy and exercise interventions was an effective treatment option for reduction of cervicogenic headache symptoms and decreasing medication intake in both the short term and at one-year follow-up.
| [18] | [19] |
| [20] | [21] |
In individuals with CGH:
- weakness in the deep neck flexors6,7,8
- increased activity in the superficial flexors
- atrophy in the suboccipital extensors and so the deep muscle sleeve which is important for active support of the cervical segments becomes impaired
- muscle tightness and trigger points
- upper trapezius, sternocleidomastoid, scalenes, levator scapulae, pectoralis major and minor, and short sub-occipital extensors have been implicated 6,7,10
Elements of exercise program:
- Re-educating craniocervical spine flexor muscles
• Re-education of CCF (craniocervical flexion) movement6
The neck flexor muscle synergy is tested with the CCF test (link to Cranio‐cervical Flexion Test on physiopedia). The patient palpates the superficial flexors to avoid their inappropriate use. An emphasis on precision and control is essential.
• Training the low level endurance capacity of the deep neck flexors6
Begins as soon as the patient can perform the CCF movement correctly. This phase tests the patient’s ability to hold (approximately 10 seconds) the cranio-cervical flexion position in each stage of the test on repeated occasions.9 Pressure biofeedback is used to guide training (link to biofeedback on physiopedia). Training begins at the pressure level that the patient can achieve and hold steady with a good pattern, without dominant use or substitution by the superficial flexor muscles. The patient performs the formal exercise at least twice daily. For each pressure level, the holding time is built up to 10 seconds and 10 repetitions are performed, eventually to the desired level of 30 mm Hg.
• Retraining the cervical flexors for antigravity function in sitting position6
The exercise is a controlled eccentric action of the flexors into cervical extension range followed by a concentric action of these muscles to return the head to the neutral upright position. The return to the upright position must be initiated by CCF, rather than a dominant action of sternocleidomastoid. The exercise is progressed by gradually increasing the range to which the head is moved into extension as control improves, and introducing isometric holds through range.
- Extensors of the craniocervical spine6
The patient practices eccentric control of the head into flexion followed by concentric control back to the neutral position in a 4 point kneeling position to train the coordination of the deep and superficial cervical extensors. These exercises are incorporated with re-education of the scapular muscles in these positions and are commenced early in the program. The exercise is progressed by performing alternating small ranges of craniocervical extension and flexion while maintaining the cervical spine in a neutral position.
- Co-contraction of the neck flexors and extensors6
The co-contraction is facilitated with rotation and the exercises are introduced once the patient can activate the deep muscles. The patient uses self resisted isometric rotation in a correct upright sitting posture. They look into the palm of the hand, providing the resistance to facilitate the muscles and perform the alternating rhythmic stabilisation exercises with an emphasis on slow onset and slow release holding contractions, using resistance to match about a 10–20% effort.
- Retraining the strength of the superficial and deep flexor synergy6
The head lift must be preceded with CCF followed by cervical flexion to just lift the head from the bed. Gravity and head load provide the resistance. Care must be taken that high load exercise is not introduced too early, as it may be provocative of symptoms.
- Retraining the scapular muscles
• Retraining scapular orientation in posture6
A correction strategy is to have the patient move the coracoids upward and the acromion backwards, which results in a slight retraction and external rotation of the scapula. The aim is to facilitate the coordinated action of all parts of trapezius and serratus anterior, allowing lower trapezius to slightly depress the medial border of the scapula, consequently lengthening (and relaxing) the levator scapulae. Once the patient learns correct scapular orientation, he repeats the correction and maintains the position regularly throughout the day so that it becomes a habit.
• Training the endurance capacity of the scapular stabilisers6
Repeated repetitions of 10 second holds of the corrected scapular position encourages early endurance retraining. Endurance of the middle and lower trapezius muscles is also trained by performing exercise in the prone lying position against the effects of gravity.
• Retraining scapular control with arm movement and load6
This is important when activities such as computer or deskwork aggravate pain. The patient is encouraged to maintain their newly learnt scapular position while performing small range (+/- 60 degrees) arm movements, or during, for example, work at a computer. Scapular control in association with control of cervicothoracic postural position is also trained for functional activities such as lifting and carrying.
- Upper quarter strengthening exercises7
Adding upper quarter exercises for patients with cervical dysfunction is important in order to integrate ‘global’ muscles that have connections to the cervical spine through anatomical chains (most notably those connecting the axial and appendicular skeletons).
These exercises include:
• Shoulder abduction
• Shoulder retraction
• Lat pull-down
• Push-up
• Chest press
• Shrug
• Arm curl
• Bent-over row
• Chest flies
- Re-education of posture6
Posture is an indirect measure of the functional status of the neuromuscular system.10 Postural position is trained in sitting and is corrected from the pelvis. The second aspect of re-education of postural position is correction of scapular position. Maintenance of a correct scapular position with appropriate muscle coordination has the added benefit of inducing reciprocal relaxation in muscles such as levator scapulae, which reduces muscular pain in the area.
- Sensorimotor training because CGHs are thought to be a dysfynction of the sensorimotor system7
Sensorimotor exercises include progressive exercise on unstable surfaces to promote reflexive stabilization and postural stability. Unstable surfaces such as exercise balls or foam pads can be used to add challenge to the cervical spine as well as the whole-body for stabilization exercises. These final stages of the rehabilitation program for CGH patients can be progressed toward functional activities to return the patient to full participation.
[edit | edit source]
Treatment Examples[edit | edit source]
| Seated CT Manipulation | Seated Mid Thoracic Manipulation |
| Deep Neck Flexor Exercises | |
| Middle Trapezius Strengthening | Lower Trapezius Strengthening |

|

|
Key Research[edit | edit source]
- Jull G, Stanton W. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101-108.[9]
- Hall T et all. Clinical Evaluation of Cervicogenic Headache: A Clinical Perspective. Journal of Manual and Manipulative Therapy. 2008;16:73-80.[13]
Resources[edit | edit source]
- International Headache Society
- Diagnosis and management of cervicogenic headache. Sizer PS Jr, Phelps V, Azevedo E, Haye A, Vaught M. Pain Pract. 2005 Sep;5(3):255-74.
- The diagnostic validity of the cervical flexion-rotation test in C1/2-related cervicogenic headache. Ogince M, Hall T, Robinson K, Blackmore AM. Man Ther. 2007 Aug;12(3):256-62.
- Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. Hall T, Chan HT, Christensen L, Odenthal B, Wells C, Robinson K. J. Orthop Sports Phys Ther. 2007 Mar;37(3):100-7.
- Clinical evaluation of cervicogenic headache: a clinical perspective. Fernández-de-Las-Peñas C. J Man Manip Ther. 2008;16(2):81.
Recent Case Studies[edit | edit source]
- J Man Manip Ther. 2007;15(1):10-24.
- van Duijn J, van Duijn AJ, Nitsch W. Orthopaedic manual physical therapy including thrust manipulation and exercise in the management of a patient with cervicogenic headache: a case report.
Clinical Bottom Line[edit | edit source]
Cervicogenic headaches are brought on by neck dysfunction and present in a unilateral "ram’s horn" pattern. The flexion-rotation test is a diagnostic method with high sensitivity and specificity that assists in differentiating it from other types, such as migraines, tension, and cluster headaches. PT treatment should include cervical mobilization, cervical or thoracic thrust manipulation, and deep neck flexor and upper quarter strengthening.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1LC7_OBLVE9Hc3UrOAdwx9miGAMRquG4Mg6-pr5u6uky_VMIMD|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Goodman, C, Fuller, K. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier, 2009.
- ↑ Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol 2009; 8: 959–68.
- ↑ 3.0 3.1 HIS Classification ICHD-II. Cervicogenic headache [M99]. http://ihs-classification.org/en/02_klassifikation/03_teil2/11.02.01_cranial.html (accessed 13 April 2011).
- ↑ Headache Classification Subcommittee of the International HeadacheSociety. The international classification of headache disorders.2nd edition. Cephalalgia 2004;24:suppl 1.
- ↑ Pfaffenrath and Kaube(1990); Nilsson (1995)
- ↑ Antonaci F, Sjaastad O. Cervicogenic headache: a real headache. Curr Neurol Neurosci Rep. 2011;4:149-155
- ↑ Haldeman S. Dagenais S. Choosing a treatment for cervicogenic headache: when? what? how much?. The Spine journal 2010;10 169-171
- ↑ 8.0 8.1 8.2 8.3 Becker WJ. Cervicogenic Headache: Evidence that the neck is a pain generator. Headache. 2010;4 699-705
- ↑ 9.0 9.1 9.2 9.3 9.4 Jull G, Stanton W. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101-108.
- ↑ Haas M, Spegman A, Peterson D, Aickin M, Vavrek D. Dose response and efficacy of spinal manipulation for chronic cervicogenic headache: a pilot randomized controlled trial. Spine Journal [serial on the Internet]. (2010, Feb), [cited May 1, 2011]; 10(2): 117-128.
- ↑ Zwart JA. Neck mobility in different headache disorders. Headache 1997;37:6–11.
- ↑ Bovim G. Cervicogenic headache, migraine, and tension-type headache. Pressure-pain threshold measurements. Pain 1992;51: 169–73.
- ↑ 13.0 13.1 13.2 13.3 Hall T et all. Clinical Evaluation of Cervicogenic Headache: A Clinical Perspective. Journal of Manual and Manipulative Therapy. 2008;16:73-80. Cite error: Invalid
<ref>tag; name "Hall" defined multiple times with different content - ↑ Boxem K, Erd M, Brinkhuize T, Patijn J, Kleef M, Zundert J. Radiofrequency and Pulsed Radiofrequency Treatment of Chronic Pain Syndromes: The Available Evidence. Pain Practice 2008;8:385-393.
- ↑ 15.0 15.1 Fritz JM, Brennan GP. Preliminary Examination of a Proposed Treatment-Based Classification System for Patients Receiving Physical Therapy Interventions for Neck Pain. Physical Therapy. 2007;87:513-524.
- ↑ Cleland et al. Examination of a Clinical Prediction Rule to Identify Patients with Neck Pain Likely to Benefit from Thoracic Spine Thrust Manipulation and a General Cervical Range of Motion Exercise: Muti-Center Randomized Clinical Trial. Physical Therapy. 2010;90:1239-1253.
- ↑ Hall T et al. Efficacy of a C1-C2 Self-sustained Natural Apophyseal Glide (SNAG) in the Management of Cervicogenic Headache JOSPT 2007;37:100-107.
- ↑ harrisonvaughanpt. C1-2 Rotatory HVLAT Chin-Hold Technique. Available from: http://www.youtube.com/watch?v=KdFUfVFEb4U [last accessed 24/11/12]
- ↑ OptimumCareProviders. 1.2 Deep Neck Flexor - Longus Colli Strengthening Level 2. Available from: http://www.youtube.com/watch?v=1smVSuQiQx8 [last accessed 09/03/13]
- ↑ ReligiosoPT. Supine Thoracic Thrust. Available from: http://www.youtube.com/watch?v=Rj4Y5JGNPZs[last accessed 09/03/13]|}
- ↑ TherExVids. Cervical Rotation Self Mobilization Using a Strap. Available from: http://www.youtube.com/watch?v=TNb2cLsgc6c[last accessed 09/03/13]|}
22. Bogduk N., The anatomical basis for cervicogenic headache, J Manipulative Physiol Ther p.67-70, 1992. Level of evidence: 1