Cesarean Section: Difference between revisions
Nicole Hills (talk | contribs) mNo edit summary |
Nicole Hills (talk | contribs) mNo edit summary |
||
| Line 73: | Line 73: | ||
# '''Uterine incision.''' | # '''Uterine incision.''' | ||
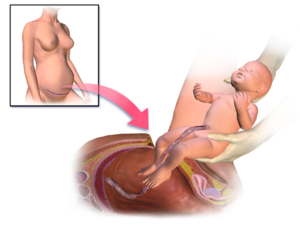
# '''Delivery of head:'''The membranes are ruptured if it is still intact. The blood mixed amniotic fluid is sucked out by continuous suction. The Doyen’s retractor is removed. The head is delivered by hooking the head with the fingers which are carefully insinuated between the lower uterine flap and the head until the palm is placed below the head. The head is delivered by elevation and flexion using the palm to act as fulcrum. As the head is drawn to incision line, the assistant is to apply pressure on the fundus. If the head is jammed, an assistant may push up the head by sterile gloved fingers introduced into the vagina. The head can also be delivered using either Wringley’s or Barton’s forceps. Delivery of the trunk: As soon as the head is delivered, the mucus from the mouth, pharynx and nostrils are sucked out using rubber catheter attached to an electric suction machine. After the delivery of the shoulders, intravenous oxytocin 20 units or methergine 0.2 mg has to be administered. The rest of the body should be delivered slowly and the baby should be placed in a tray placed in between the mother’s thighs with the head tilted down for gravitational drainage. The cord should be cut in between two clamps and the baby should be handed over to the paediatrician. The Doyen’s retractor is reintroduced. '''The optimum interval between uterine incision and delivery should be less than 90 seconds.''' | # '''Delivery of head:'''The membranes are ruptured if it is still intact. The blood mixed amniotic fluid is sucked out by continuous suction. The Doyen’s retractor is removed. The head is delivered by hooking the head with the fingers which are carefully insinuated between the lower uterine flap and the head until the palm is placed below the head. The head is delivered by elevation and flexion using the palm to act as fulcrum. As the head is drawn to incision line, the assistant is to apply pressure on the fundus. If the head is jammed, an assistant may push up the head by sterile gloved fingers introduced into the vagina. The head can also be delivered using either Wringley’s or Barton’s forceps. Delivery of the trunk: As soon as the head is delivered, the mucus from the mouth, pharynx and nostrils are sucked out using rubber catheter attached to an electric suction machine. After the delivery of the shoulders, intravenous oxytocin 20 units or methergine 0.2 mg has to be administered. The rest of the body should be delivered slowly and the baby should be placed in a tray placed in between the mother’s thighs with the head tilted down for gravitational drainage. The cord should be cut in between two clamps and the baby should be handed over to the paediatrician. The Doyen’s retractor is reintroduced. '''The optimum interval between uterine incision and delivery should be less than 90 seconds.''' | ||
# '''Removal of the placenta and membranes:'''By this time, the placenta is separated spontaneously. The placenta has to be extracted by traction on the cord with simultaneous pushing of | # '''Removal of the placenta and membranes:'''By this time, the placenta is separated spontaneously. The placenta has to be extracted by traction on the cord with simultaneous pushing of the uterus towards the umbilicus per abdomen using the left hand(controlled cord traction). Routine manual removal should not be done. Dilation of internal os is not required. Exploration of the uterine cavity is desirable. | ||
# '''Suture of the uterine wound.''' | # '''Suture of the uterine wound.''' | ||
# '''Non-closure of visceral and parietal peritoneum is preferred.''' | # '''Non-closure of visceral and parietal peritoneum is preferred.''' | ||
| Line 85: | Line 85: | ||
=== Incisional pain and adhesion-related signs and symptoms === | === Incisional pain and adhesion-related signs and symptoms === | ||
The same study mentioned previously by Karakaya and colleagues (2012)<ref name=":1" /> also included transcutaneous electrical nerve stimulation (TENS). The TENS pads were placed on either side of the incision and it was set to the following parameters: frequency of 120 Hz, pulse width of 60 us, and intensity evoking a strong tingling sensation for 30 minutes.<ref name=":1" /> The researchers found that pain and difficulty performing functional activities decreased significantly as measured by [[Visual Analogue Scale|visual analogue scales]] at rest and during movement.<ref name=":1" /> This study supports other research that has indicated TENS to be effective in decreasing post- | The same study mentioned previously by Karakaya and colleagues (2012)<ref name=":1" /> also included transcutaneous electrical nerve stimulation (TENS). The TENS pads were placed on either side of the incision and it was set to the following parameters: frequency of 120 Hz, pulse width of 60 us, and intensity evoking a strong tingling sensation for 30 minutes.<ref name=":1" /> The researchers found that pain and difficulty performing functional activities decreased significantly as measured by [[Visual Analogue Scale|visual analogue scales]] at rest and during movement.<ref name=":1" /> This study supports other research that has indicated TENS to be effective in decreasing post-cesarean incisional pain.<ref>Hollinger JL. Transcutaneous electrical nerve stimulation after cesarean birth. Physical therapy. 1986 Jan 1;66(1):36-8.</ref><ref>Kayman-Kose S, Arioz DT, Toktas H, Koken G, Kanat-Pektas M, Kose M, Yilmazer M. Transcutaneous electrical nerve stimulation (TENS) for pain control after vaginal delivery and cesarean section. The Journal of Maternal-Fetal & Neonatal Medicine. 2014 Oct 1;27(15):1572-5.</ref><ref>Navarro CN, Pacheco MC. Transcutaneous electric stimulation (TENS) to reduce pain after cesarean section. Ginecologia y obstetricia de Mexico. 2000 Feb;68:60-3.</ref><ref>Smith CM, Guralnick MS, Gelfand MM, Jeans ME. The effects of transcutaneous electrical nerve stimulation on post-cesarean pain. Pain. 1986 Nov 1;27(2):181-93.</ref> A meta-analysis calculated the mean formation rate of adhesions to be 41% amongst women undergoing cesarean section procedures.<ref name=":2">Okabayashi K, Ashrafian H, Zacharakis E, Hasegawa H, Kitagawa Y, Athanasiou T, Darzi A. Adhesions after abdominal surgery: a systematic review of the incidence, distribution and severity. Surgery today. 2014 Mar 1;44(3):405-20.</ref> and postoperative adhesions have been found to be a culprit in chronic pain.<ref name=":2" /><ref>Nikolajsen L, Sørensen HC, Jensen TS, Kehlet H. Chronic pain following Caesarean section. Acta Anaesthesiologica Scandinavica. 2004 Jan;48(1):111-6.</ref> Nonsurgical management has included various soft tissue interventions. In a pilot study, Comesana and colleagues (2017)<ref name=":4">Comesaña AC, Vicente MD, Ferreira TD, del Mar Pérez-La Fuente M, Quintáns MM, Pilat A. Effect of myofascial induction therapy on post-c-section scars, more than one and a half years old. Pilot study. Journal of bodywork and movement therapies. 2017 Jan 1;21(1):197-204.</ref> performed myofascial induction therapy sessions on 10 women with cesarean section scars older than 1.5 years. Results were similar, in that they showed improved structure of the scar and improved function and quality of life as measured by ultrasound, Schober’s Test, and the [[36-Item Short Form Survey (SF-36)|36-Item Short Form Survey]] (SF-36).<ref name=":4" /> A randomized controlled trial was done more recently by Wasserman and colleagues (2018).<ref name=":5">Wasserman JB, Abraham K, Massery M, Chu J, Farrow A, Marcoux BC. Soft Tissue Mobilization Techniques Are Effective in Treating Chronic Pain Following Cesarean Section: A Multicenter Randomized Clinical Trial. Journal of Women’s Health Physical Therapy. 2018 Sep 1;42(3):111-9.</ref> Participants were split into 2 groups who received 4 treatments. Group 1 received superficial massage and scar rolling; Group 2 received the same treatment in addition to abdominal myofascial release and deep scar mobilization.<ref name=":5" /> Results for both groups showed significant improvements in pain, pressure pain threshold, scar mobility, and the [[Oswestry Disability Index]].<ref name=":5" /> Furthermore, this study supports the effectiveness of deep and superficial interventions.<ref name=":5" /> | ||
=== Gastrointestinal Complications === | === Gastrointestinal Complications === | ||
Post-operative illeus (POI) is a common gastro-intestinal complication experienced following | Post-operative illeus (POI) is a common gastro-intestinal complication experienced following cesarean sections.<ref name=":7">Abadi F, Shahabinejad M, Abadi F, Kazemi M. Effect of acupressure on symptoms of postoperative ileus after cesarean section. Journal of acupuncture and meridian studies. 2017 Apr 1;10(2):114-9.</ref> Post-operative ileus occurs when there is blockage of the intestines and is associated with failure of peristalsis (or the involuntary contractions of the digestive tract).<ref name=":7" /> During a cesarean section, excessive accumulation of blood and amniotic fluid can occur in the peritoneum cavity, increasing risk of POI.<ref name=":7" /><ref>Stewart D, Waxman K. Management of postoperative ileus. American journal of therapeutics. 2007 Nov 1;14(6):561-6.</ref><ref>Farideh A, Monayere P, Atiyeh M, Fateme TS, Mohamad V. The effect of chewing gum in prevention of ileus after cesarean. Hayat. 2007;2:35-40.</ref>. Symptoms of POI include accumulation of gastrointestinal secretions and gas, distension of the abdomen, constipation, vomiting and nausea.<ref name=":7" /> | ||
Acupressure provides a safe, non-invasive and convenient technique to manage POI symptoms post cesarean section. During acupressure, an individual’s fingers or a sharp object can be used to apply pressure to various | Acupressure provides a safe, non-invasive and convenient technique to manage POI symptoms post-cesarean section. During acupressure, an individual’s fingers or a sharp object can be used to apply pressure to various acupoints to achieve different therapeutic effects.<ref>Kaviani M, Ashoori M, Azima S, Rajaei Fard AR, Hadian Fard MJ. Comparing the effect of two methods of acupressure and ice massage on the pain, anxiety levels and labor length in the point LI-4. SSU_Journals. 2012 Jun 10;20(2):220-8.</ref> Abadi and colleagues (2017),<ref name=":7" /> who conducted a randomized control trial evaluating the efficacy of acupressure in restoring peristalsis after cesarean section, stated that acupressure shortens the time to the first passage of flatus and time to the first presence of bowel sounds.<ref name=":7" /> The acupoints used were Zusanli (stomach meridian ST-36) and Hegu (large intestine meridian IL-4).<ref name=":7" /> The acupressure sessions lasted 20 minutes, where moderate pressure was applied in a non-clockwise direction using the thumb.<ref name=":7" /> Additionally, other studies have demonstrated a therapeutic effect for the acupoint P6 at reducing the incidence of nausea and vomiting post-cesarean sections. <ref>Ho CM, Hseu SS, Tsai SK, Lee TY. Effect of P‐6 acupressure on prevention of nausea and vomiting after epidural morphine for post‐Cesarean section pain relief. Acta anaesthesiologica scandinavica. 1996 Mar;40(3):372-5.</ref><ref>Harmon D, Ryan M, Kelly A, Bowen M. Acupressure and prevention of nausea and vomiting during and after spinal anaesthesia for caesarean section. British journal of anaesthesia. 2000 Apr 1;84(4):463-7.</ref>Although there are some studies highlighting the effectiveness of acupressure, it is important to consider that other studies have had less conclusive results and further research is still needed.<ref name=":7" /><ref>Yin J, Chen JD. Gastrointestinal motility disorders and acupuncture. Autonomic Neuroscience. 2010 Oct 28;157(1-2):31-7.</ref> | ||
Similar to acupressure, the use of acupuncture on the acupoint PC6 has been effective in treating nausea and vomiting | Similar to acupressure, the use of acupuncture on the acupoint PC6 has been effective in treating nausea and vomiting postoperatively, during pregnancy and following chemotherapy.<ref>Dundee JW, McMillan CM. Clinical uses of P6 acupuncture antiemesis. Acupuncture & electro-therapeutics research. 1990 Jan 1;15(3-4):211-5.</ref><ref>Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. Journal of the Royal Society of Medicine. 1996 Jun;89(6):303-11.</ref><ref>Parfitt A. Acupuncture as an antiemetic treatment. The Journal of Alternative and Complementary Medicine. 1996 Feb 1;2(1):167-74.</ref><ref>Jewell D, Young G. Interventions for nausea and vomiting in early pregnancy. Cochrane Database of Systematic Reviews. 2003(4).</ref><ref>Shi HZ. Application of traditional Chinese medicine in space medical research. Hang tian yi xue yu yi xue gong cheng= Space medicine & medical engineering. 2001 Feb;14(1):75-8.</ref><ref>Flake ZA, Scalley R, Bailey AG. Practical selection of antiemetics. American family physician. 2004 Mar 1;69(5):1169-74.</ref> Although the benefits of acupuncture to accelerate gastrointestinal recovery post-cesarean has been reported in a few studies<ref>Sun W, Li M, Lin T, Sun Z, Zhuang Z, Wen J, Ji S, Xie Y, Lu J, Luo C, Wu W. Effectiveness of acupuncture for recovery of flatulence after cesarean section: A case report. Medicine. 2018 Dec;97(50).</ref><ref>Zhou D, Hu B, He S, Li X, Gong H, Li F, Wang Q. Transcutaneous Electrical Acupoint Stimulation Accelerates the Recovery of Gastrointestinal Function after Cesarean Section: A Randomized Controlled Trial. Evidence-Based Complementary and Alternative Medicine. 2018;2018.</ref> evidence is still limited. | ||
Other techniques proposed in the literature include connective tissue manipulation or massage (CTM) and exercise. CTM is a type of reflex therapy that involves applying a shear force to the different fascial interfaces of the skin to stimulate autonomic nerve endings.<ref name=":8">Holey LA. Connective tissue manipulation: towards a scientific rationale. Physiotherapy. 1995 Dec 1;81(12):730-9.</ref><ref name=":9">Holey EA. Connective tissue massage: a bridge between complementary and orthodox approaches. Journal of bodywork and movement therapies. 2000 Jan 1;4(1):72-80.</ref> Through stimulation of the segmental and supra-segmental reflexes, CTM can help to decrease pain and visceral dysfunction.<ref name=":8" /><ref name=":9" /><ref name=":10">Goats GC, Keir KA. Connective tissue massage. British journal of sports medicine. 1991 Sep 1;25(3):131-3.</ref><ref>Tappan FM. Healing massage techniques: Holistic, classic, and emerging methods. Appleton & Lange; 1988.</ref>Karakaya and colleagues (2012)<ref name=":1" /> reported benefits of CTM in conjunction with posterior pelvic tilt exercises in the early return of intestinal function post-cesarean section. In this study, CTM was applied daily to the sacral and lumbar regions, including strokes to the sacrum, iliac crests, and SI joints, in sessions lasting 5 minutes.<ref name=":1" /> The pelvic exercises were performed at 10 | Other techniques proposed in the literature include connective tissue manipulation or massage (CTM) and exercise. CTM is a type of reflex therapy that involves applying a shear force to the different fascial interfaces of the skin to stimulate autonomic nerve endings.<ref name=":8">Holey LA. Connective tissue manipulation: towards a scientific rationale. Physiotherapy. 1995 Dec 1;81(12):730-9.</ref><ref name=":9">Holey EA. Connective tissue massage: a bridge between complementary and orthodox approaches. Journal of bodywork and movement therapies. 2000 Jan 1;4(1):72-80.</ref> Through stimulation of the segmental and supra-segmental reflexes, CTM can help to decrease pain and visceral dysfunction.<ref name=":8" /><ref name=":9" /><ref name=":10">Goats GC, Keir KA. Connective tissue massage. British journal of sports medicine. 1991 Sep 1;25(3):131-3.</ref><ref>Tappan FM. Healing massage techniques: Holistic, classic, and emerging methods. Appleton & Lange; 1988.</ref>Karakaya and colleagues (2012)<ref name=":1" /> reported benefits of CTM in conjunction with posterior pelvic tilt exercises in the early return of intestinal function post-cesarean section. In this study, CTM was applied daily to the sacral and lumbar regions, including strokes to the sacrum, iliac crests, and SI joints, in sessions lasting 5 minutes.<ref name=":1" /> The pelvic exercises were performed at 10 repetitions, 3 times per day.<ref name=":1" /> The use of pelvic exercises to create passive movement within the intestines and CTM to stimulate the segmental reflexes and restore bowel function has also been supported by the research of Noble (2003)<ref name=":11">Noble E. Essential exercises for the childbearing year: a guide to health and comfort before and after your baby is born. New Life Images; 2003.</ref> and Holey and Lawler (1995).<ref name=":12">Holey LA, Lawler H. The effects of classical massage and connective tissue manipulation on bowel function. British Journal of Therapy and Rehabilitation. 1995 Nov 2;2(11):627-31.</ref> Although some literature exists showcasing the benefits of CTM, it is not commonly used in practice due to the lack of scientific theory behind the technique.<ref name=":12" /><ref name=":10" /> | ||
=== Vascular Complications === | === Vascular Complications === | ||
During pregnancy, the risk of venous thromboembolism is 5 times higher than non-pregnant individuals,<ref name=":13">Bagaria SJ, Bagaria VB. Strategies for diagnosis and prevention of venous thromboembolism during pregnancy. Journal of pregnancy. 2011;2011.</ref><ref>James AH. Venous thromboembolism in pregnancy. Arteriosclerosis, Thrombosis, and Vascular Biology. 2009 Mar 1;29(3):326-31</ref><ref>Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Annals of internal medicine. 2005 Nov 15;143(10):697-706.</ref> with the risk increasing to 20 times higher during the postpartum period.<ref name=":13" /> Delivery by cesarean, especially an emergency cesarean section, can increase this risk further.<ref name=":13" /> Pulmonary edema occurs in 80% of pregnancies, half of which are experienced in the lower extremities.<ref>Cho S, Atwood JE. Peripheral edema. The American journal of medicine. 2002 Nov 1;113(7):580-6.</ref> | During pregnancy, the risk of venous thromboembolism is 5 times higher than non-pregnant individuals,<ref name=":13">Bagaria SJ, Bagaria VB. Strategies for diagnosis and prevention of venous thromboembolism during pregnancy. Journal of pregnancy. 2011;2011.</ref><ref>James AH. Venous thromboembolism in pregnancy. Arteriosclerosis, Thrombosis, and Vascular Biology. 2009 Mar 1;29(3):326-31</ref><ref>Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Annals of internal medicine. 2005 Nov 15;143(10):697-706.</ref> with the risk increasing to 20 times higher during the postpartum period.<ref name=":13" /> Delivery by cesarean, especially an emergency cesarean section, can increase this risk further.<ref name=":13" /> Pulmonary edema occurs in 80% of pregnancies, half of which are experienced in the lower extremities.<ref>Cho S, Atwood JE. Peripheral edema. The American journal of medicine. 2002 Nov 1;113(7):580-6.</ref> | ||
Physical therapists can play a role in managing vascular complications by providing patients with an exercise plan that includes both active and passive exercise and is targeted towards the lower extremities.<ref name=":13" /><ref name=":14">Sochart DH, Hardinge K. The relationship of foot and ankle movements to venous return in the lower limb. The Journal of bone and joint surgery. British volume. 1999 Jul;81(4):700-4.</ref> Such exercises can include range of motion of the ankle and flexion and extension of the hip and knee.<ref name=":11" /><ref name=":13" /> These exercises improve circulation, reduce edema, aid in the prevention of post-operative circulatory complications, and prepare the individual for ambulation following surgery. <ref name=":1" /><ref name=":11" /><ref name=":15">Polden M, Mantle J. Physiotherapy in Obstetrics and Gynecology. Oxford: Butterworth – Heinemann; 1994.</ref> Following their study, Karakaya and colleagues (2012)<ref name=":1" /> stated lower extremity exercise in combination with respiratory exercise improved blood circulation, allowed for early ambulation and reduced the side-effects experienced from the anesthesia post-op. <ref name=":1" /><ref name=":11" /><ref name=":14" /><ref name=":15" /> The exercises in this study were completed at 10 | Physical therapists can play a role in managing vascular complications by providing patients with an exercise plan that includes both active and passive exercise and is targeted towards the lower extremities.<ref name=":13" /><ref name=":14">Sochart DH, Hardinge K. The relationship of foot and ankle movements to venous return in the lower limb. The Journal of bone and joint surgery. British volume. 1999 Jul;81(4):700-4.</ref> Such exercises can include range of motion of the ankle and flexion and extension of the hip and knee.<ref name=":11" /><ref name=":13" /> These exercises improve circulation, reduce edema, aid in the prevention of post-operative circulatory complications, and prepare the individual for ambulation following surgery. <ref name=":1" /><ref name=":11" /><ref name=":15">Polden M, Mantle J. Physiotherapy in Obstetrics and Gynecology. Oxford: Butterworth – Heinemann; 1994.</ref> Following their study, Karakaya and colleagues (2012)<ref name=":1" /> stated lower extremity exercise in combination with respiratory exercise improved blood circulation, allowed for early ambulation and reduced the side-effects experienced from the anesthesia post-op. <ref name=":1" /><ref name=":11" /><ref name=":14" /><ref name=":15" /> The exercises in this study were completed at 10 repetitions, 3 times per day and included circumflexion of the ankles, knee flexion and extension, and leg bracing.<ref name=":1" /> | ||
Other management strategies include early ambulation, if not contraindicated, and the use of gradual compression stockings that reach thigh height to promote venous return in the proximal veins.<ref name=":13" /> | Other management strategies include early ambulation, if not contraindicated, and the use of gradual compression stockings that reach thigh height to promote venous return in the proximal veins.<ref name=":13" /> | ||
| Line 106: | Line 106: | ||
Lower extremity exercises have been linked to earlier mobilization and decreased pain.<ref name=":1" /> Studies support early mobilization, sometime between 6 and 24 hours post-operatively, to improve pulmonary function, reduce the risk of embolism, and decrease the length of hospital stay.<ref>Jacobsen AF, Skjeldestad FE, Sandset PM. Ante‐and postnatal risk factors of venous thrombosis: a hospital‐based case–control study. Journal of thrombosis and haemostasis. 2008 Jun;6(6):905-12.</ref><ref>Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. Cmaj. 2007 Feb 13;176(4):455-60.</ref><ref>Deniau B, Bouhadjari N, Faitot V, Mortazavi A, Kayem G, Mandelbrot L, Keita H. Evaluation of a continuous improvement programme of enhanced recovery after caesarean delivery under neuraxial anaesthesia. Anaesthesia Critical Care & Pain Medicine. 2016 Dec 1;35(6):395-9.</ref> | Lower extremity exercises have been linked to earlier mobilization and decreased pain.<ref name=":1" /> Studies support early mobilization, sometime between 6 and 24 hours post-operatively, to improve pulmonary function, reduce the risk of embolism, and decrease the length of hospital stay.<ref>Jacobsen AF, Skjeldestad FE, Sandset PM. Ante‐and postnatal risk factors of venous thrombosis: a hospital‐based case–control study. Journal of thrombosis and haemostasis. 2008 Jun;6(6):905-12.</ref><ref>Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. Cmaj. 2007 Feb 13;176(4):455-60.</ref><ref>Deniau B, Bouhadjari N, Faitot V, Mortazavi A, Kayem G, Mandelbrot L, Keita H. Evaluation of a continuous improvement programme of enhanced recovery after caesarean delivery under neuraxial anaesthesia. Anaesthesia Critical Care & Pain Medicine. 2016 Dec 1;35(6):395-9.</ref> | ||
In their study, Karakaya and colleagues (2012)<ref name=":1" /> also incorporated exercises to retrain posture. Study participants performed 5-10 repetitions, 3x/day, especially after breastfeeding. | In their study, Karakaya and colleagues (2012)<ref name=":1" /> also incorporated exercises to retrain posture. Study participants performed 5-10 repetitions, 3x/day, especially after breastfeeding. Participants were also encouraged to contract their pelvic floor during activities that required an increase in intra-abdominal pressure.<ref name=":1" /> Unfortunately, they did not investigate the lasting effects of these interventions because there was no long-term follow-up. Some evidence has found that there is a higher incidence of pelvic floor muscle dysfunction following a vaginal birth<ref>Bortolini MA, Drutz HP, Lovatsis D, Alarab M. Vaginal delivery and pelvic floor dysfunction: current evidence and implications for future research. International urogynecology journal. 2010 Aug 1;21(8):1025-30.</ref><ref>de Souza Caroci A, Riesco ML, Da Silva Sousa W, Cotrim AC, Sena EM, Rocha NL, Fontes CN. Analysis of pelvic floor musculature function during pregnancy and postpartum: a cohort study: (A prospective cohort study to assess the PFMS by perineometry and digital vaginal palpation during pregnancy and following vaginal or caesarean childbirth). Journal of clinical nursing. 2010 Sep;19(17‐18):2424-33.</ref> but other studies have not shown a significant difference in the incidence following a vaginal or cesarean birth.<ref>Barbosa AM, Marini G, Piculo F, Rudge CV, Calderon IM, Rudge MV. Prevalence of urinary incontinence and pelvic floor muscle dysfunction in primiparae two years after cesarean section: cross-sectional study. Sao Paulo Medical Journal. 2013;131(2):95-9.</ref><ref>Hilde G, Stær-Jensen J, Siafarikas F, Engh ME, Brækken IH, Bø K. Impact of childbirth and mode of delivery on vaginal resting pressure and on pelvic floor muscle strength and endurance. American journal of obstetrics and gynecology. 2013 Jan 1;208(1):50-e1.</ref> | ||
A study by Gursen and colleagues (2016)<ref>Gürşen C, İnanoğlu D, Kaya S, Akbayrak T, Baltacı G. Effects of exercise and Kinesio taping on abdominal recovery in women with cesarean section: a pilot randomized controlled trial. Archives of gynecology and obstetrics. 2016 Mar 1;293(3):557-65.</ref> looked at the effects of Kinesio taping (KT) combined with exercise compared to exercise alone on abdominal rehabilitation after cesarean sections. KT application on the rectus abdominal muscles, oblique abdominal muscles and cesarean incision 2x/week for 4 weeks | A study by Gursen and colleagues (2016)<ref>Gürşen C, İnanoğlu D, Kaya S, Akbayrak T, Baltacı G. Effects of exercise and Kinesio taping on abdominal recovery in women with cesarean section: a pilot randomized controlled trial. Archives of gynecology and obstetrics. 2016 Mar 1;293(3):557-65.</ref> looked at the effects of Kinesio taping (KT) combined with exercise compared to exercise alone on abdominal rehabilitation after cesarean sections. KT application on the rectus abdominal muscles, oblique abdominal muscles and cesarean incision 2x/week for 4 weeks led to more significant improvements in abdominal strength, pain, and self-reported disability as measured by manual muscle testing and sit-up tests, the [[Visual Analogue Scale|Visual Analog Scale (VAS)]], and the [[Roland‐Morris Disability Questionnaire|Roland Morris Disability Questionnaire]].<ref>Gürşen C, İnanoğlu D, Kaya S, Akbayrak T, Baltacı G. Effects of exercise and Kinesio taping on abdominal recovery in women with cesarean section: a pilot randomized controlled trial. Archives of gynecology and obstetrics. 2016 Mar 1;293(3):557-65.</ref> | ||
It is known that there is an increased likelihood of the development of [[diastasis recti abdominis]] (DRA) during pregnancy and following abdominal surgery. More information on DRA and core training exercises can be found [[Diastasis recti abdominis|here]]. Women are at an increased risk of developing pelvic-floor dysfunction during pregnancy,<ref>Herbert J. Pregnancy and childbirth: the effects on pelvic floor muscles. Nurs Times. 2009 Mar 24;105(7):38-41.</ref> and pelvic floor rehabilitation may be required post-cesarean section. More information about [[Pelvic Floor Dysfunction|pelvic floor conditions]] can be found [[Pelvic Floor Dysfunction|here]]. | It is known that there is an increased likelihood of the development of [[diastasis recti abdominis]] (DRA) during pregnancy and following abdominal surgery. More information on DRA and core training exercises can be found [[Diastasis recti abdominis|here]]. Women are at an increased risk of developing pelvic-floor dysfunction during pregnancy,<ref>Herbert J. Pregnancy and childbirth: the effects on pelvic floor muscles. Nurs Times. 2009 Mar 24;105(7):38-41.</ref> and pelvic floor rehabilitation may be required post-cesarean section. More information about [[Pelvic Floor Dysfunction|pelvic floor conditions]] can be found [[Pelvic Floor Dysfunction|here]]. | ||
It is also important to consider the symptoms that arise during pregnancy. Back pain is common and can result in functional limitations.<ref>MacEvilly M, Buggy D. Back pain and pregnancy: a review. Pain. 1996 Mar 1;64(3):405-14.</ref><ref>Liddle SD, Pennick V. Interventions for preventing and treating low‐back and pelvic pain during pregnancy. Cochrane Database of Systematic Reviews. 2015(9).</ref> Okanishi and colleagues (2012)<ref>Okanishi N, Kito N, Akiyama M, Yamamoto M. Spinal curvature and characteristics of postural change in pregnant women. Acta obstetricia et gynecologica Scandinavica. 2012 Jul;91(7):856-61.</ref> also found that a decrease in muscle tone during pregnancy may contribute to poor posture. Additionally, the diaphragm must elevate during pregnancy while the fetus is developing, which may lead to dyspnea.<ref>Stephenson RG, O'Connor LJ. Obstetric and gynecologic care in physical therapy. Slack Incorporated; 2000.</ref> Furthermore, exercises for pelvic pain,<ref>Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal. 2008 Jun 1;17(6):794-819.</ref> body mechanics, postural correction, and breathing may be of benefit. A single-subject design case report by Kilmartin (2017)<ref name=":6">Kilmartin L. Physical Therapy Management of Thoracic Pain, Lumbar Pain, and Vasovagal Response During Pregnancy. Journal of Women's Health Physical Therapy. 2017 Jan 1;41(1):28-41.</ref> carried out a physical therapy management program on a 37-year-old primigravida, 24 weeks' gestation, comprised of exercises (relaxation, improving posture, trunk mobility and flexibility, etc), manual therapy, and education. The program was found to be successful in treating thoracic and lumbar pain and abolishing the recurrence of vasovagal symptoms as measured by the [[Numeric Pain Rating Scale]] and Functional Rating Index.<ref name=":6" /> | It is also important to consider the musculoskeletal symptoms that may arise during pregnancy. Back pain is common and can result in functional limitations.<ref>MacEvilly M, Buggy D. Back pain and pregnancy: a review. Pain. 1996 Mar 1;64(3):405-14.</ref><ref>Liddle SD, Pennick V. Interventions for preventing and treating low‐back and pelvic pain during pregnancy. Cochrane Database of Systematic Reviews. 2015(9).</ref> Okanishi and colleagues (2012)<ref>Okanishi N, Kito N, Akiyama M, Yamamoto M. Spinal curvature and characteristics of postural change in pregnant women. Acta obstetricia et gynecologica Scandinavica. 2012 Jul;91(7):856-61.</ref> also found that a decrease in muscle tone during pregnancy may contribute to poor posture. Additionally, the diaphragm must elevate during pregnancy while the fetus is developing, which may lead to dyspnea.<ref>Stephenson RG, O'Connor LJ. Obstetric and gynecologic care in physical therapy. Slack Incorporated; 2000.</ref> Furthermore, exercises for pelvic pain,<ref>Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal. 2008 Jun 1;17(6):794-819.</ref> body mechanics, postural correction, and breathing may be of benefit. A single-subject design case report by Kilmartin (2017)<ref name=":6">Kilmartin L. Physical Therapy Management of Thoracic Pain, Lumbar Pain, and Vasovagal Response During Pregnancy. Journal of Women's Health Physical Therapy. 2017 Jan 1;41(1):28-41.</ref> carried out a physical therapy management program on a 37-year-old primigravida, 24 weeks' gestation, comprised of exercises (relaxation, improving posture, trunk mobility and flexibility, etc), manual therapy, and education. The program was found to be successful in treating thoracic and lumbar pain and abolishing the recurrence of vasovagal symptoms as measured by the [[Numeric Pain Rating Scale]] and Functional Rating Index.<ref name=":6" /> | ||
=== Abdominal Support === | === Abdominal Support === | ||
Ghana and colleagues (2017)<ref name=":16">Ghana S, Hakimi S, Mirghafourvand M, Abbasalizadeh F, Behnampour N. Randomized controlled trial of abdominal binders for postoperative pain, distress, and blood loss after cesarean delivery. International Journal of Gynecology & Obstetrics. 2017 Jun;137(3):271-6.</ref> | Ghana and colleagues (2017)<ref name=":16">Ghana S, Hakimi S, Mirghafourvand M, Abbasalizadeh F, Behnampour N. Randomized controlled trial of abdominal binders for postoperative pain, distress, and blood loss after cesarean delivery. International Journal of Gynecology & Obstetrics. 2017 Jun;137(3):271-6.</ref> found that the use of abdominal binders can reduce post-operative pain (measured via the [[Visual Analogue Scale|VAS]]) and symptom distress (measured via the symptom distress scale (SDS)) following cesarean delivery. It was also noted that mothers who received abdominal binders had higher hemoglobin and hematocrit levels following cesarean delivery.<ref name=":16" /> This would have implications in preventing haemorrhage postoperatively.<ref name=":16" /> Similarly, a study by Gustafson and colleagues (2018),<ref name=":17">Gustafson JL, Dong F, Duong J, Kuhlmann ZC. Elastic abdominal binders reduce cesarean pain postoperatively: A randomized controlled pilot trial. Kansas Journal of Medicine. 2018 May;11(2):48.</ref> reported benefits of elastic abdominal binders in lowering postoperative pain scores, however these researchers did not find a similar effect on hemoglobin concentrations.<ref name=":17" /> | ||
Tussey and colleagues (2019)<ref name=":18">Tussey C, Kelly LA, Oja KJ, Bay RC, Makarova N. Reducing Discomfort After Cesarean Birth Using Abdominal Binders. MCN: The American Journal of Maternal/Child Nursing. 2019 Nov 1;44(6):310-6.</ref> found abdominal binders to be beneficial in reducing post-ambulation pain. Additionally, this study reported that mothers who wore abdominal binders reported slightly reduced discomfort during coughing, sneezing and breathing, as well reported feeling more abdominal support wearing the binder during these activities.<ref name=":18" /> Given that standard nursing care teaches post-operative patients to splint their abdomen with a pillow during coughing and sneezing, using an abdominal binder post | Tussey and colleagues (2019)<ref name=":18">Tussey C, Kelly LA, Oja KJ, Bay RC, Makarova N. Reducing Discomfort After Cesarean Birth Using Abdominal Binders. MCN: The American Journal of Maternal/Child Nursing. 2019 Nov 1;44(6):310-6.</ref> found abdominal binders to be beneficial in reducing post-ambulation pain. Additionally, this study reported that mothers who wore abdominal binders reported slightly reduced discomfort during coughing, sneezing and breathing, as well reported feeling more abdominal support wearing the binder during these activities.<ref name=":18" /> Given that standard nursing care teaches post-operative patients to splint their abdomen with a pillow during coughing and sneezing, using an abdominal binder post-cesarean could provide mothers with the ability to care for their baby using both hands and not worry about holding a pillow for splinting.<ref name=":18" /> | ||
Furthermore, the use of abdominal binders has implications for enhancing a mother's bonding with their baby.<ref name=":17" /> | Furthermore, the use of abdominal binders has implications for enhancing a mother's bonding with their baby.<ref name=":17" /> It has been found in the literature that mothers with higher levels of post-operative pain less likely to breast-feed and engage in early infant care.<ref>Karlström A, Engström‐Olofsson R, Norbergh KG, Sjöling M, Hildingsson I. Postoperative pain after cesarean birth affects breastfeeding and infant care. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2007 Sep 1;36(5):430-40.</ref><ref>Woods AB, Crist B, Kowalewski S, Carroll J, Warren J, Robertson J. A cross‐sectional analysis of the effect of patient‐controlled epidural analgesia versus patient controlled analgesia on postcesarean pain and breastfeeding. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2012 May 1;41(3):339-46.</ref> Currently, there is no literature that explores breastfeeding as an outcome while using an abdominal binder, abdominal binders have the potential to reduce post-operative pain which may have a positive impact on the mother's ability to breastfeed and engage with their newborns more easily.<ref name=":17" /> It is important to note that Tussey and colleagues (2019)<ref name=":18" /> recommend that abdominal binders should be loosened while breastfeeding.<ref name=":18" /> | ||
Although | Although the studies mentioned above have reported benefits with abdominal binders post-cesarean section, it is important to note that evidence is still limited and some studies have reported no benefits.<ref>Gillier CM, Sparks JR, Kriner R, Anasti JN. A randomized controlled trial of abdominal binders for the management of postoperative pain and distress after cesarean delivery. International Journal of Gynecology & Obstetrics. 2016 May;133(2):188-91.</ref> | ||
=== Patient Education === | === Patient Education === | ||
Although cesarean sections are one of the most common surgical procedures worldwide, | Although cesarean sections are one of the most common surgical procedures worldwide, women have reported feeling unprepared for this surgery and they are not provided with the necessary education regarding the risks and benefits to this mode of delivery. <ref name=":19">Daly B, Young S, Marla R, Riddell L, Junkin R, Weidenhammer N, et al. Persistent Pain After Caesarean Section and its Association With Maternal Anxiety and Socioeconomic Background. Obstetric Anesthesia Digest. 2017;37(4):184–5.</ref><ref>Lee YM, Dalton ME. Cesarean Delivery on Maternal Request: The Impact on Mother and Newborn. Clinics in Perinatology. 2008;35(3):505–18.</ref> The National Collaborating Centre for Women’s and Children’s Health and the National Institute for Clinical Excellence (2004) suggest that evidence-based information should be provided to women by their healthcare practitioners to enable women to make informed decisions and act as active members in their care.<ref name=":20">Farnworth A, Robson S, Thomson R, Watson DB, Murtagh M. Decision support for women choosing mode of delivery after a previous caesarean section: A developmental study. Patient Education and Counseling. 2008;71(1):116–24.</ref><ref name=":21">Bick D. Caesarean Section. Clinical Guideline. National Collaborating Centre for Womens and Childrens Health: Worldviews on Evidence-Based Nursing. 2004;1(3):198–9</ref> Effective communication and education while building a strong therapeutic alliance with the patient can increase their confidence and competence to make autonomous decisions.<ref>Roter D. The medical visit context of treatment decision-making and the therapeutic relationship. Health Expectations. 2000;3(1):17–25.</ref> Women value the ability to be involved and make decisions regarding their maternity care,<ref name=":20" /> therefore, healthcare practitioners are required to provide their patients with the information they need to feel empowered and capable of making informed choices about their care.<ref name=":21" /> | ||
Explaining some of the risks of cesarean sections when compared with vaginal delivery can be anxiety-provoking, however, Farnworth and colleagues suggest that there is a general consensus among women that it is necessary.<ref name=":20" /> Although the first mentions of any risks can be stressful for women, some relief is gained when women understand the relative rarity of some of the more serious complications as well as management strategies or prevention techniques for some of the more common complications.<ref name=":20" /> Women find it difficult to understand what information they need and where to gather it,<ref name=":20" /> therefore, physiotherapists should play a key role in providing this information and educating their patients on the risks and benefits of the modes of delivery. In all patient interactions, appropriate language should be considered and used to provide positive emotional support to patients undergoing the stressful and sometimes traumatic decision-making process about mode of delivery, labour preparation, and the post-partum recovery period. For example, some clinical experts suggest avoiding terms such as “natural” or “normal” delivery when referring to vaginal delivery. Furthermore, clinical experts also encourage practitioners to consider and address that | Explaining some of the risks of cesarean sections when compared with vaginal delivery can be anxiety-provoking, however, Farnworth and colleagues (2008) suggest that there is a general consensus among women that it is necessary.<ref name=":20" /> Although the first mentions of any risks can be stressful for women, some relief is gained when women understand the relative rarity of some of the more serious complications as well as management strategies or prevention techniques for some of the more common complications.<ref name=":20" /> Women find it difficult to understand what information they need and where to gather it,<ref name=":20" /> therefore, physiotherapists should play a key role in providing this information and educating their patients on the risks and benefits of the modes of delivery. In all patient interactions, appropriate language should be considered and used to provide positive emotional support to patients undergoing the stressful and sometimes traumatic decision-making process about mode of delivery, labour preparation, and the post-partum recovery period. For example, some clinical experts suggest avoiding terms such as “natural” or “normal” delivery when referring to vaginal delivery. Furthermore, clinical experts also encourage practitioners to consider and address the emotions and feelings that their patients who have undergone both planned and unplanned cesarean sections experience. | ||
Prior to delivery, it is important to empower women and provide them with the | Prior to delivery, it is important to empower women and provide them with education on the cesarean delivery process, acute post-operative management, and precautions and contraindication in the early post-partum period. Clinical experts suggest providing handouts and/or videos to pregnant patients with cesarean section information, including pre-delivery preparation, the delivery process, and how to address rehabilitation. Physiotherapists should perform individualized assessments and cater to each patients’ learning style. For example, patient-friendly videos describing the cesarean section are accessible online for visual learners, a handout or podcast can be recommended for auditory learners, and practice in the clinic can reach kinesthetic learners. Physiotherapists should prepare their patients with information about the operation and what it will look like, such as how long the surgery will last, when they can expect the baby to be born, and what options are available to them once the baby is born such as, skin to skin contact and light dimming in the operating room. In order to ensure patients feel confident and prepared going into their cesarean section, it would be beneficial to practice certain exercises and adjustments in movements so patients can maintain function while minimizing pain and discomfort in the early postoperative days. Patients who have cesarean sections will remain in the hospital for 2-3 days post-delivery without access to a physiotherapist, therefore, in order to ensure moms are well-prepared to care for their babies, physiotherapists should teach and practice bed mobility, splinting, wound management, abdominal supports, positions of comfort, and the importance of early mobilization with all expecting mothers. Immediately post-cesarean section and throughout the first few months of the 4<sup>th</sup> trimester, women who undergo cesarean sections should expect to experience incision or wound-site pain and sensitivity.<ref name=":19" /> Preparing patients for incision pain, managing expectations, and providing techniques to avoid or control pain can limit anxiety and fear associated with postoperative outcomes.<ref name=":19" /> For example, the waistline on women’s pants tend to fit directly over the line of incision of a cesarean section, so it may be relevant to suggest to patients that they bring large sweatpants to pull them up over the incision site in order to avoid pain and sensitivity while in hospital. Additionally, physiotherapists should prepare their patients with bedside exercises and exercise progressions for the immediate postoperative and early post-partum periods while they await their post-delivery 6-week checkup. | ||
Women who undergo cesarean sections are more likely to experience difficulties with breastfeeding | Women who undergo cesarean sections are more likely to experience difficulties with breastfeeding.<ref name=":22">Hobbs AJ, Mannion CA, Mcdonald SW, Brockway M, Tough SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy and Childbirth. 2016;16(1).</ref> Because of this, physiotherapists should provide education and manage expectations surrounding potential breastfeeding complications and pain management techniques as well as breastfeeding resources such as lactation support from lactation consultants. Healthcare professionals working with pregnant women should be aware that women who have cesarean sections have an increased likelihood of experiencing breastfeeding complications and may require extra support during the post-operative and early post-partum periods. There are many hypotheses as to why cesarean sections may be associated with breastfeeding difficulties such as, the maternal and fetal stress response related to cesarean sections, the physiologic and abdominal surgery influence on lactogenesis (the onset of milk secretion), and incision pain.<ref name=":22" /><ref>Evans KC. Effect of caesarean section on breast milk transfer to the normal term newborn over the first week of life. Archives of Disease in Childhood - Fetal and Neonatal Edition. 2003;88(5).</ref> Mothers should be provided with breastfeeding encouragement and support prior to and immediately post-birth to anticipate and mitigate difficulties.<ref name=":22" /> For example, a physiotherapist could provide supportive resources to seek out, discuss immediate skin-to-skin contact, make referrals, and suggest a breastfeeding baby support to decrease the friction and pressure on the incision. | ||
== References == | == References == | ||
Revision as of 02:51, 25 June 2020
Definition[edit | edit source]
- A cesarean section can be defined as the procedure in which the delivery of a baby is through an incision in the abdominal wall and uterus rather than through the pelvis and vagina.[2][3][4][5][6] General, spinal or epidural anesthesia is used.[7]
- The incision used during a cesarean section can be vertical (up-and-down) or transverse (side-to-side). However, the condition of the mother and the fetus determines which type of incision will be used.
Transverse Incision[edit | edit source]
- Its extension lies across the pubic hairline.
- It is most commonly used because it heals faster and there is minimal bleeding.
- It also increases the chance for normal delivery in future pregnancies.
Vertical Incision[edit | edit source]
Its extension is from navel to pubic hairline.
Reasons for the Procedure[edit | edit source]
Some cesarean deliveries are planned and scheduled, while others are performed as a result of complication that occurs during labour. There are several conditions in which cesarean delivery is more likely to occur. These include:
- Fetal distress, indicated by abnormal fetal heart rate
- Abnormal position of the fetus breech presentation (breech or transverse positioning)
- Labour that fails to progress
- Size of a baby is too large to be delivered vaginally
- Placental complications like placenta previa
- Maternal medical conditions such as diabetes, high blood pressure, HIV infection
- Active herpes infection in the mother’s vagina or cervix
- Carrying multiples
- Previous history of cesarean delivery.[8][9] Initially, clinicians were concerned about the scar from the previous birth rupturing. However, growing evidence is supporting safe vaginal birth after caesarean (VBAC).[10][11][12][13]
Procedure[edit | edit source]
Preoperative Preparation[edit | edit source]
Informed written permission from the patient for the procedure, anesthesia and blood transfusion is obtained.
- The abdomen is scrubbed with soap and nonorganic iodide lotion. Hair is usually clipped.
- Premedication sedatives should not be given.
- Nonparticulate antacid (0.3 molar sodium citrate, 30 ml) is given orally before transferring the patient to the operation theatre. This is given to neutralize the existing gastric acid.
- Ranitidine 150 mg may be given orally the night before and it is repeated 1 hour before the surgery to raise the gastric pH.
- The stomach should be emptied, If needed, it can be emptied by a stomach tube also.
- Metoclopramide (10 mg) is given to increase the tone of the lower esophageal sphincter as well as to reduce the stomach contents. It is administered after 3 minutes of preoxygenation in the operation theatre.
- Bladder has to be emptied by a Foley catheter which is kept in place in the perioperative period.
- Fetal heart sound should be evaluated again at this stage.
- Neonatologist should be available at this stage.
- Cross-match blood when above-average blood loss (placenta previa, prior multiple cesarean deliveries) is expected.
- Prophylactic antibiotics should be given (IV) before cesarean section.
Important Consideration:[edit | edit source]
IV cannula: Placed to administer fluids.
Procedure[edit | edit source]
- Position of the patient: The patient should be placed in the dorsal position. In susceptible cases, to minimize any harmful effects of venacaval compression, a 15 degree tilt to her left using a wedge till delivery of the baby should be done.
- Anesthesia- can be spinal, epidural or general. However, the choice of the patient and the urgency of delivery is also considered.
- Antiseptic painting- the abdomen should be painted with 7.5% povidone-iodine solution or savlon lotion and should be properly draped with sterile towels.
- Incision on the abdomen.
- Packing:The Doyen’s retractor is introduced in this stage.
- Uterine incision.
- Delivery of head:The membranes are ruptured if it is still intact. The blood mixed amniotic fluid is sucked out by continuous suction. The Doyen’s retractor is removed. The head is delivered by hooking the head with the fingers which are carefully insinuated between the lower uterine flap and the head until the palm is placed below the head. The head is delivered by elevation and flexion using the palm to act as fulcrum. As the head is drawn to incision line, the assistant is to apply pressure on the fundus. If the head is jammed, an assistant may push up the head by sterile gloved fingers introduced into the vagina. The head can also be delivered using either Wringley’s or Barton’s forceps. Delivery of the trunk: As soon as the head is delivered, the mucus from the mouth, pharynx and nostrils are sucked out using rubber catheter attached to an electric suction machine. After the delivery of the shoulders, intravenous oxytocin 20 units or methergine 0.2 mg has to be administered. The rest of the body should be delivered slowly and the baby should be placed in a tray placed in between the mother’s thighs with the head tilted down for gravitational drainage. The cord should be cut in between two clamps and the baby should be handed over to the paediatrician. The Doyen’s retractor is reintroduced. The optimum interval between uterine incision and delivery should be less than 90 seconds.
- Removal of the placenta and membranes:By this time, the placenta is separated spontaneously. The placenta has to be extracted by traction on the cord with simultaneous pushing of the uterus towards the umbilicus per abdomen using the left hand(controlled cord traction). Routine manual removal should not be done. Dilation of internal os is not required. Exploration of the uterine cavity is desirable.
- Suture of the uterine wound.
- Non-closure of visceral and parietal peritoneum is preferred.
- Concluding Part:The mops placed inside are removed and the number is checked. Peritoneal toileting should be done and blood clots are to be removed carefully and precisely. The tubes and ovaries are examined. Doyen’s retractor is removed. After being satisfied the uterus is well contracted, the abdomen is closed in layers. The vagina is cleansed of blood clots and a sterile vulval pad is placed.[14]
Physiotherapy Management after Caesarean Section[edit | edit source]
Mothers who give birth via cesarean delivery still require the same postpartum intervention as mothers who undergo vaginal delivery. Additionally, since a cesarean section is a major abdominal surgery, mothers may also require general post-surgical rehabilitation.
Pulmonary complications[edit | edit source]
Karakaya and colleagues (2012)[15] investigated the effectiveness of a physiotherapy program on pain and function acutely after a cesarean section. The treatment program incorporated thoracic expansion and huffing exercises to help with respiratory function, ambulation and circulation. Unfortunately, since the program consisted of numerous components it is difficult to determine if these exercises specifically impacted the improved function of the women in this study. However, the researchers did conclude that physiotherapy care in the early post-caesarian period may help to improve function after childbirth and further research is needed in this area[15]. While respiratory therapy after cesarean sections has not been adequately explored in the literature, there has been studies done on various abdominal surgeries[16][17][18]. A systematic review by Pasquina and colleagues (2006)[17] concluded that the available evidence is older and has limitations, so it is not enough to justify the routine use of respiratory physiotherapy after abdominal surgeries[17]. However, more recently, the postoperative period has been found to put patients at an increased risk of pulmonary complications. [18] Patients often present with decreased peak cough flow after upper abdominal surgery (incision extending above the umbilicus)[16] secondary to postoperative restrictive lung dysfunction.[16] To help mobilize secretions and maximize cough effectiveness, especially in high-risk patients, thoracic expansion/deep breathing may allow for lung inflation and gas exchange. It is important to educate and teach women how to huff and splint a cough after a major abdominal surgery such as a cesarean section.
[edit | edit source]
The same study mentioned previously by Karakaya and colleagues (2012)[15] also included transcutaneous electrical nerve stimulation (TENS). The TENS pads were placed on either side of the incision and it was set to the following parameters: frequency of 120 Hz, pulse width of 60 us, and intensity evoking a strong tingling sensation for 30 minutes.[15] The researchers found that pain and difficulty performing functional activities decreased significantly as measured by visual analogue scales at rest and during movement.[15] This study supports other research that has indicated TENS to be effective in decreasing post-cesarean incisional pain.[19][20][21][22] A meta-analysis calculated the mean formation rate of adhesions to be 41% amongst women undergoing cesarean section procedures.[23] and postoperative adhesions have been found to be a culprit in chronic pain.[23][24] Nonsurgical management has included various soft tissue interventions. In a pilot study, Comesana and colleagues (2017)[25] performed myofascial induction therapy sessions on 10 women with cesarean section scars older than 1.5 years. Results were similar, in that they showed improved structure of the scar and improved function and quality of life as measured by ultrasound, Schober’s Test, and the 36-Item Short Form Survey (SF-36).[25] A randomized controlled trial was done more recently by Wasserman and colleagues (2018).[26] Participants were split into 2 groups who received 4 treatments. Group 1 received superficial massage and scar rolling; Group 2 received the same treatment in addition to abdominal myofascial release and deep scar mobilization.[26] Results for both groups showed significant improvements in pain, pressure pain threshold, scar mobility, and the Oswestry Disability Index.[26] Furthermore, this study supports the effectiveness of deep and superficial interventions.[26]
Gastrointestinal Complications[edit | edit source]
Post-operative illeus (POI) is a common gastro-intestinal complication experienced following cesarean sections.[27] Post-operative ileus occurs when there is blockage of the intestines and is associated with failure of peristalsis (or the involuntary contractions of the digestive tract).[27] During a cesarean section, excessive accumulation of blood and amniotic fluid can occur in the peritoneum cavity, increasing risk of POI.[27][28][29]. Symptoms of POI include accumulation of gastrointestinal secretions and gas, distension of the abdomen, constipation, vomiting and nausea.[27]
Acupressure provides a safe, non-invasive and convenient technique to manage POI symptoms post-cesarean section. During acupressure, an individual’s fingers or a sharp object can be used to apply pressure to various acupoints to achieve different therapeutic effects.[30] Abadi and colleagues (2017),[27] who conducted a randomized control trial evaluating the efficacy of acupressure in restoring peristalsis after cesarean section, stated that acupressure shortens the time to the first passage of flatus and time to the first presence of bowel sounds.[27] The acupoints used were Zusanli (stomach meridian ST-36) and Hegu (large intestine meridian IL-4).[27] The acupressure sessions lasted 20 minutes, where moderate pressure was applied in a non-clockwise direction using the thumb.[27] Additionally, other studies have demonstrated a therapeutic effect for the acupoint P6 at reducing the incidence of nausea and vomiting post-cesarean sections. [31][32]Although there are some studies highlighting the effectiveness of acupressure, it is important to consider that other studies have had less conclusive results and further research is still needed.[27][33]
Similar to acupressure, the use of acupuncture on the acupoint PC6 has been effective in treating nausea and vomiting postoperatively, during pregnancy and following chemotherapy.[34][35][36][37][38][39] Although the benefits of acupuncture to accelerate gastrointestinal recovery post-cesarean has been reported in a few studies[40][41] evidence is still limited.
Other techniques proposed in the literature include connective tissue manipulation or massage (CTM) and exercise. CTM is a type of reflex therapy that involves applying a shear force to the different fascial interfaces of the skin to stimulate autonomic nerve endings.[42][43] Through stimulation of the segmental and supra-segmental reflexes, CTM can help to decrease pain and visceral dysfunction.[42][43][44][45]Karakaya and colleagues (2012)[15] reported benefits of CTM in conjunction with posterior pelvic tilt exercises in the early return of intestinal function post-cesarean section. In this study, CTM was applied daily to the sacral and lumbar regions, including strokes to the sacrum, iliac crests, and SI joints, in sessions lasting 5 minutes.[15] The pelvic exercises were performed at 10 repetitions, 3 times per day.[15] The use of pelvic exercises to create passive movement within the intestines and CTM to stimulate the segmental reflexes and restore bowel function has also been supported by the research of Noble (2003)[46] and Holey and Lawler (1995).[47] Although some literature exists showcasing the benefits of CTM, it is not commonly used in practice due to the lack of scientific theory behind the technique.[47][44]
Vascular Complications[edit | edit source]
During pregnancy, the risk of venous thromboembolism is 5 times higher than non-pregnant individuals,[48][49][50] with the risk increasing to 20 times higher during the postpartum period.[48] Delivery by cesarean, especially an emergency cesarean section, can increase this risk further.[48] Pulmonary edema occurs in 80% of pregnancies, half of which are experienced in the lower extremities.[51]
Physical therapists can play a role in managing vascular complications by providing patients with an exercise plan that includes both active and passive exercise and is targeted towards the lower extremities.[48][52] Such exercises can include range of motion of the ankle and flexion and extension of the hip and knee.[46][48] These exercises improve circulation, reduce edema, aid in the prevention of post-operative circulatory complications, and prepare the individual for ambulation following surgery. [15][46][53] Following their study, Karakaya and colleagues (2012)[15] stated lower extremity exercise in combination with respiratory exercise improved blood circulation, allowed for early ambulation and reduced the side-effects experienced from the anesthesia post-op. [15][46][52][53] The exercises in this study were completed at 10 repetitions, 3 times per day and included circumflexion of the ankles, knee flexion and extension, and leg bracing.[15]
Other management strategies include early ambulation, if not contraindicated, and the use of gradual compression stockings that reach thigh height to promote venous return in the proximal veins.[48]
Functional re-training[edit | edit source]
Lower extremity exercises have been linked to earlier mobilization and decreased pain.[15] Studies support early mobilization, sometime between 6 and 24 hours post-operatively, to improve pulmonary function, reduce the risk of embolism, and decrease the length of hospital stay.[54][55][56]
In their study, Karakaya and colleagues (2012)[15] also incorporated exercises to retrain posture. Study participants performed 5-10 repetitions, 3x/day, especially after breastfeeding. Participants were also encouraged to contract their pelvic floor during activities that required an increase in intra-abdominal pressure.[15] Unfortunately, they did not investigate the lasting effects of these interventions because there was no long-term follow-up. Some evidence has found that there is a higher incidence of pelvic floor muscle dysfunction following a vaginal birth[57][58] but other studies have not shown a significant difference in the incidence following a vaginal or cesarean birth.[59][60]
A study by Gursen and colleagues (2016)[61] looked at the effects of Kinesio taping (KT) combined with exercise compared to exercise alone on abdominal rehabilitation after cesarean sections. KT application on the rectus abdominal muscles, oblique abdominal muscles and cesarean incision 2x/week for 4 weeks led to more significant improvements in abdominal strength, pain, and self-reported disability as measured by manual muscle testing and sit-up tests, the Visual Analog Scale (VAS), and the Roland Morris Disability Questionnaire.[62]
It is known that there is an increased likelihood of the development of diastasis recti abdominis (DRA) during pregnancy and following abdominal surgery. More information on DRA and core training exercises can be found here. Women are at an increased risk of developing pelvic-floor dysfunction during pregnancy,[63] and pelvic floor rehabilitation may be required post-cesarean section. More information about pelvic floor conditions can be found here.
It is also important to consider the musculoskeletal symptoms that may arise during pregnancy. Back pain is common and can result in functional limitations.[64][65] Okanishi and colleagues (2012)[66] also found that a decrease in muscle tone during pregnancy may contribute to poor posture. Additionally, the diaphragm must elevate during pregnancy while the fetus is developing, which may lead to dyspnea.[67] Furthermore, exercises for pelvic pain,[68] body mechanics, postural correction, and breathing may be of benefit. A single-subject design case report by Kilmartin (2017)[69] carried out a physical therapy management program on a 37-year-old primigravida, 24 weeks' gestation, comprised of exercises (relaxation, improving posture, trunk mobility and flexibility, etc), manual therapy, and education. The program was found to be successful in treating thoracic and lumbar pain and abolishing the recurrence of vasovagal symptoms as measured by the Numeric Pain Rating Scale and Functional Rating Index.[69]
Abdominal Support[edit | edit source]
Ghana and colleagues (2017)[70] found that the use of abdominal binders can reduce post-operative pain (measured via the VAS) and symptom distress (measured via the symptom distress scale (SDS)) following cesarean delivery. It was also noted that mothers who received abdominal binders had higher hemoglobin and hematocrit levels following cesarean delivery.[70] This would have implications in preventing haemorrhage postoperatively.[70] Similarly, a study by Gustafson and colleagues (2018),[71] reported benefits of elastic abdominal binders in lowering postoperative pain scores, however these researchers did not find a similar effect on hemoglobin concentrations.[71]
Tussey and colleagues (2019)[72] found abdominal binders to be beneficial in reducing post-ambulation pain. Additionally, this study reported that mothers who wore abdominal binders reported slightly reduced discomfort during coughing, sneezing and breathing, as well reported feeling more abdominal support wearing the binder during these activities.[72] Given that standard nursing care teaches post-operative patients to splint their abdomen with a pillow during coughing and sneezing, using an abdominal binder post-cesarean could provide mothers with the ability to care for their baby using both hands and not worry about holding a pillow for splinting.[72]
Furthermore, the use of abdominal binders has implications for enhancing a mother's bonding with their baby.[71] It has been found in the literature that mothers with higher levels of post-operative pain less likely to breast-feed and engage in early infant care.[73][74] Currently, there is no literature that explores breastfeeding as an outcome while using an abdominal binder, abdominal binders have the potential to reduce post-operative pain which may have a positive impact on the mother's ability to breastfeed and engage with their newborns more easily.[71] It is important to note that Tussey and colleagues (2019)[72] recommend that abdominal binders should be loosened while breastfeeding.[72]
Although the studies mentioned above have reported benefits with abdominal binders post-cesarean section, it is important to note that evidence is still limited and some studies have reported no benefits.[75]
Patient Education[edit | edit source]
Although cesarean sections are one of the most common surgical procedures worldwide, women have reported feeling unprepared for this surgery and they are not provided with the necessary education regarding the risks and benefits to this mode of delivery. [76][77] The National Collaborating Centre for Women’s and Children’s Health and the National Institute for Clinical Excellence (2004) suggest that evidence-based information should be provided to women by their healthcare practitioners to enable women to make informed decisions and act as active members in their care.[78][79] Effective communication and education while building a strong therapeutic alliance with the patient can increase their confidence and competence to make autonomous decisions.[80] Women value the ability to be involved and make decisions regarding their maternity care,[78] therefore, healthcare practitioners are required to provide their patients with the information they need to feel empowered and capable of making informed choices about their care.[79]
Explaining some of the risks of cesarean sections when compared with vaginal delivery can be anxiety-provoking, however, Farnworth and colleagues (2008) suggest that there is a general consensus among women that it is necessary.[78] Although the first mentions of any risks can be stressful for women, some relief is gained when women understand the relative rarity of some of the more serious complications as well as management strategies or prevention techniques for some of the more common complications.[78] Women find it difficult to understand what information they need and where to gather it,[78] therefore, physiotherapists should play a key role in providing this information and educating their patients on the risks and benefits of the modes of delivery. In all patient interactions, appropriate language should be considered and used to provide positive emotional support to patients undergoing the stressful and sometimes traumatic decision-making process about mode of delivery, labour preparation, and the post-partum recovery period. For example, some clinical experts suggest avoiding terms such as “natural” or “normal” delivery when referring to vaginal delivery. Furthermore, clinical experts also encourage practitioners to consider and address the emotions and feelings that their patients who have undergone both planned and unplanned cesarean sections experience.
Prior to delivery, it is important to empower women and provide them with education on the cesarean delivery process, acute post-operative management, and precautions and contraindication in the early post-partum period. Clinical experts suggest providing handouts and/or videos to pregnant patients with cesarean section information, including pre-delivery preparation, the delivery process, and how to address rehabilitation. Physiotherapists should perform individualized assessments and cater to each patients’ learning style. For example, patient-friendly videos describing the cesarean section are accessible online for visual learners, a handout or podcast can be recommended for auditory learners, and practice in the clinic can reach kinesthetic learners. Physiotherapists should prepare their patients with information about the operation and what it will look like, such as how long the surgery will last, when they can expect the baby to be born, and what options are available to them once the baby is born such as, skin to skin contact and light dimming in the operating room. In order to ensure patients feel confident and prepared going into their cesarean section, it would be beneficial to practice certain exercises and adjustments in movements so patients can maintain function while minimizing pain and discomfort in the early postoperative days. Patients who have cesarean sections will remain in the hospital for 2-3 days post-delivery without access to a physiotherapist, therefore, in order to ensure moms are well-prepared to care for their babies, physiotherapists should teach and practice bed mobility, splinting, wound management, abdominal supports, positions of comfort, and the importance of early mobilization with all expecting mothers. Immediately post-cesarean section and throughout the first few months of the 4th trimester, women who undergo cesarean sections should expect to experience incision or wound-site pain and sensitivity.[76] Preparing patients for incision pain, managing expectations, and providing techniques to avoid or control pain can limit anxiety and fear associated with postoperative outcomes.[76] For example, the waistline on women’s pants tend to fit directly over the line of incision of a cesarean section, so it may be relevant to suggest to patients that they bring large sweatpants to pull them up over the incision site in order to avoid pain and sensitivity while in hospital. Additionally, physiotherapists should prepare their patients with bedside exercises and exercise progressions for the immediate postoperative and early post-partum periods while they await their post-delivery 6-week checkup.
Women who undergo cesarean sections are more likely to experience difficulties with breastfeeding.[81] Because of this, physiotherapists should provide education and manage expectations surrounding potential breastfeeding complications and pain management techniques as well as breastfeeding resources such as lactation support from lactation consultants. Healthcare professionals working with pregnant women should be aware that women who have cesarean sections have an increased likelihood of experiencing breastfeeding complications and may require extra support during the post-operative and early post-partum periods. There are many hypotheses as to why cesarean sections may be associated with breastfeeding difficulties such as, the maternal and fetal stress response related to cesarean sections, the physiologic and abdominal surgery influence on lactogenesis (the onset of milk secretion), and incision pain.[81][82] Mothers should be provided with breastfeeding encouragement and support prior to and immediately post-birth to anticipate and mitigate difficulties.[81] For example, a physiotherapist could provide supportive resources to seek out, discuss immediate skin-to-skin contact, make referrals, and suggest a breastfeeding baby support to decrease the friction and pressure on the incision.
References[edit | edit source]
- ↑ Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. [CC BY 3.0 (https://creativecommons.org/licenses/by/3.0)]
- ↑ Al-Ziraqi, I, et al: uterine rupture after previous caesarean section.BJOG 117(7):809-820,2010
- ↑ Gilbert,E, and Harman, J;High risk pregnancy and delivery, ed.1.St Louis:CV Mosby,1986
- ↑ Harrington,K, and Haskvitz, E:Managing a patient’s constipation with physical therapy.Phys Ther Nov 86:1511-1519;2006
- ↑ Jamieson,D, and Steege, J:The prevalence of dysmenorrhea,dyspareunia, pelvic pain and irritable bowel syndrome in primary care practices.Obstet Gynecol 87(1):55-58,1996
- ↑ Norwood,C:caesarean variations: Patients, facilities, or policies.Int J Childbirth Educ 1 :4,1986.
- ↑ Carolyn Kisner, Lynn Allen Colby :Therapeutic Exercise Foundations and techniques 6 th edition:Pg 952
- ↑ Pushpal K Mitra : Textbook of Physiotherapy in surgical conditions:Pg 235-238
- ↑ Notzon FC, Cnattingius S, Bergsjø P, Cole S, Taffel S, Irgens L, Daltveit AK. Cesarean section delivery in the 1980's: International comparison by indication. American journal of obstetrics and gynecology. 1994 Feb 1;170(2):495-504.
- ↑ Bangal VB, Giri PA, Shinde KK, Gavhane SP. Vaginal birth after cesarean section. North American journal of medical sciences. 2013 Feb;5(2):140.
- ↑ Cahill A, Tuuli M, Odibo AO, Stamilio DM, Macones GA. Vaginal birth after caesarean for women with three or more prior caesareans: assessing safety and success. BJOG: An International Journal of Obstetrics & Gynaecology. 2010 Mar;117(4):422-8.
- ↑ Flamm BL, Goings JR, Liu Y et al. Elective repeat caesarean section versus trial of labour: a prospective multicenter study. Obstetrics and Gynecology 1994; 83: 927-932.
- ↑ McMahon MJ, Luther ER, Bowes WA et al. Comparison of trial of labour with an elective second caesarean section. New England Journal of Medicine 1996; 335: 689-695.
- ↑ Hiralal Konar:DC Dutta’s textbook of obstetrics 8 th edition:Pg 671
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 15.12 15.13 15.14 Karakaya İÇ, Yüksel İ, Akbayrak T, Demirtürk F, Karakaya MG, Özyüncü Ö, Beksaç S. Effects of physiotherapy on pain and functional activities after cesarean delivery. Archives of gynecology and obstetrics. 2012 Mar 1;285(3):621-7.
- ↑ 16.0 16.1 16.2 Colucci DB, Fiore JF, Paisani DM, Risso TT, Colucci M, Chiavegato LD, Faresin SM. Cough impairment and risk of postoperative pulmonary complications after open upper abdominal surgery. Respiratory care. 2015 May 1;60(5):673-8.
- ↑ 17.0 17.1 17.2 Pasquina P, Tramer MR, Granier JM, Walder B. Respiratory physiotherapy to prevent pulmonary complications after abdominal surgery: a systematic review. Chest. 2006 Dec 1;130(6):1887-99.
- ↑ 18.0 18.1 Silva DR, Gazzana MB, Knorst MM. Merit of preoperative clinical findings and functional pulmonary evaluation as predictors of postoperative pulmonary complications. Rev Assoc Med Bras. 2010 Jan 1;56(5):551-7.
- ↑ Hollinger JL. Transcutaneous electrical nerve stimulation after cesarean birth. Physical therapy. 1986 Jan 1;66(1):36-8.
- ↑ Kayman-Kose S, Arioz DT, Toktas H, Koken G, Kanat-Pektas M, Kose M, Yilmazer M. Transcutaneous electrical nerve stimulation (TENS) for pain control after vaginal delivery and cesarean section. The Journal of Maternal-Fetal & Neonatal Medicine. 2014 Oct 1;27(15):1572-5.
- ↑ Navarro CN, Pacheco MC. Transcutaneous electric stimulation (TENS) to reduce pain after cesarean section. Ginecologia y obstetricia de Mexico. 2000 Feb;68:60-3.
- ↑ Smith CM, Guralnick MS, Gelfand MM, Jeans ME. The effects of transcutaneous electrical nerve stimulation on post-cesarean pain. Pain. 1986 Nov 1;27(2):181-93.
- ↑ 23.0 23.1 Okabayashi K, Ashrafian H, Zacharakis E, Hasegawa H, Kitagawa Y, Athanasiou T, Darzi A. Adhesions after abdominal surgery: a systematic review of the incidence, distribution and severity. Surgery today. 2014 Mar 1;44(3):405-20.
- ↑ Nikolajsen L, Sørensen HC, Jensen TS, Kehlet H. Chronic pain following Caesarean section. Acta Anaesthesiologica Scandinavica. 2004 Jan;48(1):111-6.
- ↑ 25.0 25.1 Comesaña AC, Vicente MD, Ferreira TD, del Mar Pérez-La Fuente M, Quintáns MM, Pilat A. Effect of myofascial induction therapy on post-c-section scars, more than one and a half years old. Pilot study. Journal of bodywork and movement therapies. 2017 Jan 1;21(1):197-204.
- ↑ 26.0 26.1 26.2 26.3 Wasserman JB, Abraham K, Massery M, Chu J, Farrow A, Marcoux BC. Soft Tissue Mobilization Techniques Are Effective in Treating Chronic Pain Following Cesarean Section: A Multicenter Randomized Clinical Trial. Journal of Women’s Health Physical Therapy. 2018 Sep 1;42(3):111-9.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 27.6 27.7 27.8 Abadi F, Shahabinejad M, Abadi F, Kazemi M. Effect of acupressure on symptoms of postoperative ileus after cesarean section. Journal of acupuncture and meridian studies. 2017 Apr 1;10(2):114-9.
- ↑ Stewart D, Waxman K. Management of postoperative ileus. American journal of therapeutics. 2007 Nov 1;14(6):561-6.
- ↑ Farideh A, Monayere P, Atiyeh M, Fateme TS, Mohamad V. The effect of chewing gum in prevention of ileus after cesarean. Hayat. 2007;2:35-40.
- ↑ Kaviani M, Ashoori M, Azima S, Rajaei Fard AR, Hadian Fard MJ. Comparing the effect of two methods of acupressure and ice massage on the pain, anxiety levels and labor length in the point LI-4. SSU_Journals. 2012 Jun 10;20(2):220-8.
- ↑ Ho CM, Hseu SS, Tsai SK, Lee TY. Effect of P‐6 acupressure on prevention of nausea and vomiting after epidural morphine for post‐Cesarean section pain relief. Acta anaesthesiologica scandinavica. 1996 Mar;40(3):372-5.
- ↑ Harmon D, Ryan M, Kelly A, Bowen M. Acupressure and prevention of nausea and vomiting during and after spinal anaesthesia for caesarean section. British journal of anaesthesia. 2000 Apr 1;84(4):463-7.
- ↑ Yin J, Chen JD. Gastrointestinal motility disorders and acupuncture. Autonomic Neuroscience. 2010 Oct 28;157(1-2):31-7.
- ↑ Dundee JW, McMillan CM. Clinical uses of P6 acupuncture antiemesis. Acupuncture & electro-therapeutics research. 1990 Jan 1;15(3-4):211-5.
- ↑ Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. Journal of the Royal Society of Medicine. 1996 Jun;89(6):303-11.
- ↑ Parfitt A. Acupuncture as an antiemetic treatment. The Journal of Alternative and Complementary Medicine. 1996 Feb 1;2(1):167-74.
- ↑ Jewell D, Young G. Interventions for nausea and vomiting in early pregnancy. Cochrane Database of Systematic Reviews. 2003(4).
- ↑ Shi HZ. Application of traditional Chinese medicine in space medical research. Hang tian yi xue yu yi xue gong cheng= Space medicine & medical engineering. 2001 Feb;14(1):75-8.
- ↑ Flake ZA, Scalley R, Bailey AG. Practical selection of antiemetics. American family physician. 2004 Mar 1;69(5):1169-74.
- ↑ Sun W, Li M, Lin T, Sun Z, Zhuang Z, Wen J, Ji S, Xie Y, Lu J, Luo C, Wu W. Effectiveness of acupuncture for recovery of flatulence after cesarean section: A case report. Medicine. 2018 Dec;97(50).
- ↑ Zhou D, Hu B, He S, Li X, Gong H, Li F, Wang Q. Transcutaneous Electrical Acupoint Stimulation Accelerates the Recovery of Gastrointestinal Function after Cesarean Section: A Randomized Controlled Trial. Evidence-Based Complementary and Alternative Medicine. 2018;2018.
- ↑ 42.0 42.1 Holey LA. Connective tissue manipulation: towards a scientific rationale. Physiotherapy. 1995 Dec 1;81(12):730-9.
- ↑ 43.0 43.1 Holey EA. Connective tissue massage: a bridge between complementary and orthodox approaches. Journal of bodywork and movement therapies. 2000 Jan 1;4(1):72-80.
- ↑ 44.0 44.1 Goats GC, Keir KA. Connective tissue massage. British journal of sports medicine. 1991 Sep 1;25(3):131-3.
- ↑ Tappan FM. Healing massage techniques: Holistic, classic, and emerging methods. Appleton & Lange; 1988.
- ↑ 46.0 46.1 46.2 46.3 Noble E. Essential exercises for the childbearing year: a guide to health and comfort before and after your baby is born. New Life Images; 2003.
- ↑ 47.0 47.1 Holey LA, Lawler H. The effects of classical massage and connective tissue manipulation on bowel function. British Journal of Therapy and Rehabilitation. 1995 Nov 2;2(11):627-31.
- ↑ 48.0 48.1 48.2 48.3 48.4 48.5 Bagaria SJ, Bagaria VB. Strategies for diagnosis and prevention of venous thromboembolism during pregnancy. Journal of pregnancy. 2011;2011.
- ↑ James AH. Venous thromboembolism in pregnancy. Arteriosclerosis, Thrombosis, and Vascular Biology. 2009 Mar 1;29(3):326-31
- ↑ Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Annals of internal medicine. 2005 Nov 15;143(10):697-706.
- ↑ Cho S, Atwood JE. Peripheral edema. The American journal of medicine. 2002 Nov 1;113(7):580-6.
- ↑ 52.0 52.1 Sochart DH, Hardinge K. The relationship of foot and ankle movements to venous return in the lower limb. The Journal of bone and joint surgery. British volume. 1999 Jul;81(4):700-4.
- ↑ 53.0 53.1 Polden M, Mantle J. Physiotherapy in Obstetrics and Gynecology. Oxford: Butterworth – Heinemann; 1994.
- ↑ Jacobsen AF, Skjeldestad FE, Sandset PM. Ante‐and postnatal risk factors of venous thrombosis: a hospital‐based case–control study. Journal of thrombosis and haemostasis. 2008 Jun;6(6):905-12.
- ↑ Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. Cmaj. 2007 Feb 13;176(4):455-60.
- ↑ Deniau B, Bouhadjari N, Faitot V, Mortazavi A, Kayem G, Mandelbrot L, Keita H. Evaluation of a continuous improvement programme of enhanced recovery after caesarean delivery under neuraxial anaesthesia. Anaesthesia Critical Care & Pain Medicine. 2016 Dec 1;35(6):395-9.
- ↑ Bortolini MA, Drutz HP, Lovatsis D, Alarab M. Vaginal delivery and pelvic floor dysfunction: current evidence and implications for future research. International urogynecology journal. 2010 Aug 1;21(8):1025-30.
- ↑ de Souza Caroci A, Riesco ML, Da Silva Sousa W, Cotrim AC, Sena EM, Rocha NL, Fontes CN. Analysis of pelvic floor musculature function during pregnancy and postpartum: a cohort study: (A prospective cohort study to assess the PFMS by perineometry and digital vaginal palpation during pregnancy and following vaginal or caesarean childbirth). Journal of clinical nursing. 2010 Sep;19(17‐18):2424-33.
- ↑ Barbosa AM, Marini G, Piculo F, Rudge CV, Calderon IM, Rudge MV. Prevalence of urinary incontinence and pelvic floor muscle dysfunction in primiparae two years after cesarean section: cross-sectional study. Sao Paulo Medical Journal. 2013;131(2):95-9.
- ↑ Hilde G, Stær-Jensen J, Siafarikas F, Engh ME, Brækken IH, Bø K. Impact of childbirth and mode of delivery on vaginal resting pressure and on pelvic floor muscle strength and endurance. American journal of obstetrics and gynecology. 2013 Jan 1;208(1):50-e1.
- ↑ Gürşen C, İnanoğlu D, Kaya S, Akbayrak T, Baltacı G. Effects of exercise and Kinesio taping on abdominal recovery in women with cesarean section: a pilot randomized controlled trial. Archives of gynecology and obstetrics. 2016 Mar 1;293(3):557-65.
- ↑ Gürşen C, İnanoğlu D, Kaya S, Akbayrak T, Baltacı G. Effects of exercise and Kinesio taping on abdominal recovery in women with cesarean section: a pilot randomized controlled trial. Archives of gynecology and obstetrics. 2016 Mar 1;293(3):557-65.
- ↑ Herbert J. Pregnancy and childbirth: the effects on pelvic floor muscles. Nurs Times. 2009 Mar 24;105(7):38-41.
- ↑ MacEvilly M, Buggy D. Back pain and pregnancy: a review. Pain. 1996 Mar 1;64(3):405-14.
- ↑ Liddle SD, Pennick V. Interventions for preventing and treating low‐back and pelvic pain during pregnancy. Cochrane Database of Systematic Reviews. 2015(9).
- ↑ Okanishi N, Kito N, Akiyama M, Yamamoto M. Spinal curvature and characteristics of postural change in pregnant women. Acta obstetricia et gynecologica Scandinavica. 2012 Jul;91(7):856-61.
- ↑ Stephenson RG, O'Connor LJ. Obstetric and gynecologic care in physical therapy. Slack Incorporated; 2000.
- ↑ Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal. 2008 Jun 1;17(6):794-819.
- ↑ 69.0 69.1 Kilmartin L. Physical Therapy Management of Thoracic Pain, Lumbar Pain, and Vasovagal Response During Pregnancy. Journal of Women's Health Physical Therapy. 2017 Jan 1;41(1):28-41.
- ↑ 70.0 70.1 70.2 Ghana S, Hakimi S, Mirghafourvand M, Abbasalizadeh F, Behnampour N. Randomized controlled trial of abdominal binders for postoperative pain, distress, and blood loss after cesarean delivery. International Journal of Gynecology & Obstetrics. 2017 Jun;137(3):271-6.
- ↑ 71.0 71.1 71.2 71.3 Gustafson JL, Dong F, Duong J, Kuhlmann ZC. Elastic abdominal binders reduce cesarean pain postoperatively: A randomized controlled pilot trial. Kansas Journal of Medicine. 2018 May;11(2):48.
- ↑ 72.0 72.1 72.2 72.3 72.4 Tussey C, Kelly LA, Oja KJ, Bay RC, Makarova N. Reducing Discomfort After Cesarean Birth Using Abdominal Binders. MCN: The American Journal of Maternal/Child Nursing. 2019 Nov 1;44(6):310-6.
- ↑ Karlström A, Engström‐Olofsson R, Norbergh KG, Sjöling M, Hildingsson I. Postoperative pain after cesarean birth affects breastfeeding and infant care. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2007 Sep 1;36(5):430-40.
- ↑ Woods AB, Crist B, Kowalewski S, Carroll J, Warren J, Robertson J. A cross‐sectional analysis of the effect of patient‐controlled epidural analgesia versus patient controlled analgesia on postcesarean pain and breastfeeding. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2012 May 1;41(3):339-46.
- ↑ Gillier CM, Sparks JR, Kriner R, Anasti JN. A randomized controlled trial of abdominal binders for the management of postoperative pain and distress after cesarean delivery. International Journal of Gynecology & Obstetrics. 2016 May;133(2):188-91.
- ↑ 76.0 76.1 76.2 Daly B, Young S, Marla R, Riddell L, Junkin R, Weidenhammer N, et al. Persistent Pain After Caesarean Section and its Association With Maternal Anxiety and Socioeconomic Background. Obstetric Anesthesia Digest. 2017;37(4):184–5.
- ↑ Lee YM, Dalton ME. Cesarean Delivery on Maternal Request: The Impact on Mother and Newborn. Clinics in Perinatology. 2008;35(3):505–18.
- ↑ 78.0 78.1 78.2 78.3 78.4 Farnworth A, Robson S, Thomson R, Watson DB, Murtagh M. Decision support for women choosing mode of delivery after a previous caesarean section: A developmental study. Patient Education and Counseling. 2008;71(1):116–24.
- ↑ 79.0 79.1 Bick D. Caesarean Section. Clinical Guideline. National Collaborating Centre for Womens and Childrens Health: Worldviews on Evidence-Based Nursing. 2004;1(3):198–9
- ↑ Roter D. The medical visit context of treatment decision-making and the therapeutic relationship. Health Expectations. 2000;3(1):17–25.
- ↑ 81.0 81.1 81.2 Hobbs AJ, Mannion CA, Mcdonald SW, Brockway M, Tough SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy and Childbirth. 2016;16(1).
- ↑ Evans KC. Effect of caesarean section on breast milk transfer to the normal term newborn over the first week of life. Archives of Disease in Childhood - Fetal and Neonatal Edition. 2003;88(5).