Charcot-Marie-Tooth Disease: A Case Study: Difference between revisions
Evan Lukasik (talk | contribs) m (added hyperlinks) |
mNo edit summary |
||
| Line 109: | Line 109: | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Queen's University Neuromotor Function Project]] | [[Category:Queen's University Neuromotor Function Project]] | ||
[[Category:Neurological Conditions]] | [[Category:Neurological Conditions]] | ||
[[Category:Case Studies]] | [[Category:Case Studies]] | ||
Revision as of 03:39, 8 May 2019
Abstract[edit | edit source]
Introduction[edit | edit source]
This is a case study on a male patient with Charcot-Marie-Tooth Disease (CMT). It will detail the assessment process of the patient, as well as the interventions used and the results of these interventions.
Client Characteristics[edit | edit source]
The patient is an 18 year old male Queen's University student and varsity soccer player. He was referred to physiotherapy by a neurologist with a recent diagnosis of Charcot-Marie-Tooth Disease but was previously very fit with no significant medical history. He spends most of his time in class or at soccer practices/games. The patient complains of difficulties walking to and from class and around campus/town as well as significant decreases in ability to play a full game of soccer due to foot drop, calf pain, and bilateral lower extremity muscle fatigue and weakness. He also indicates tripping often while walking/running and problems with shooting accuracy and cutting during soccer practices/games. Finally, the patient reports a progressive decrease in his ability to sleep.
Examination Findings[edit | edit source]
Subjective[edit | edit source]
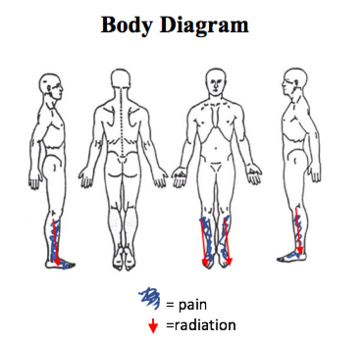
Discomfort and Pain
Onset: April 16th, 2019 (3 wks ago)
Site: bilateral antero-lateral lower leg
Characteristics: deep, dull ache or sharp and shooting
Radiation: antero-lateral leg to dorsum of the foot
Periodicity: intermittent, no discernable pattern
Duration: varies from 10-30+ minutes.
Aggravating factors: activities such as soccer or walking to class
Alleviating factors: rest
Intensity: McGill Pain Questionnaire: Sensory: 3/33, Affective: 4/12, VAS: 4/10
Objective[edit | edit source]
Observation
Lower extremities: slightly more right side calf muscle atrophy when compared to left but present bilaterally predominantly in the antero-lateral portion of the shank. Pes planus foot presentation bilaterally.
Palpation: increased tone bilaterally in the antero-lateral portions of the shank, gastrocnemius, and soleus muscles. Hypertrophic nerve, predominantly the common and superficial peroneal nerve, is palpable but not visible.
Examination
Upper and Lower Neurological Scan:
- Physiological ROM: Cervical and lumbar: WNL
- Non-physiological ROM: Cervical and lumbar: WNL
- Dermatomes: normal.
- Myotomes: decrease strength through L4- S1 bilaterally.
- AROM: right dorsiflexion slightly diminished but all other movements for upper and lower extremity WNL.
- Dural testing: negative Spurling's Test, Straight Leg Raise Test, and Slump Test.
- Reflexes: negative Babinski and Hoffman’s, decreased deep tendon reflexes bilaterally (Achilles and patellar).
- Vascularity: radial and tibial pulses found bilaterally.
Range of Motion:
- Composite functions of the hand: full
- Upper extremity: All joints WNL.
- Lower extremity: 14° of dorsiflexion on right side, all other joints WNL.
Muscle Strength Testing:
- Grip strength using dynamometer:
- Dominant hand (R) 52.1 kg, non-dominant hand (L) 49,4 kg
- Maximal Voluntary Isometric Contraction:
- Reduced strength bilaterally with dorsiflexion (R: 3/5, L: 4/5) and eversion (R: 3/5, L: 4/5).
- Repeated Body Weight Calf Raises to Fatigue:
- R: 7; L: 13
Neurological Testing:
- Deep Tendon Reflexes:
- Biceps, brachioradialis, and triceps: 2 (normal)
- Achilles and patellar: 1 (depressed but present)
- Sensation Testing:
- Issues with differentiating between hot and cold stimuli throughout the L4-L1 distributions but not between 1st and 2nd toes.
- Intact differentiating to soft touch, dull/ sharp, and crude pressure.
CMT Specific Outcome Measures:
- Fatigue Severity Scale (FSS): to measure fatigue, activities of daily living, life participation, and sleep.
- Score= 49/63
- CMT Neuropathy Score: measure of disability
- 12 /36
- Overall Neuropathy Limitations Scale (ONLS):
- Upper Limb Score:0/5 (arms not affected)
- Lower Limb Score: 2/7(Walks independently but gait looks abnormal)
- Total score: 2/12
Balance Assessment:
- Community Balance and Mobility Scale (CBMS) : 81/96
Gait Analysis:
- 10 Meter Walk Test (T10MW): 1.1 m/sec
- Observation:
- Step and stride length WNL, stride width WNL, no noticeable deviation from normal time spent in single and double support, stance phase slightly longer on the left side, and swing phase slightly longer on the right side. There is a lower walking speed of 1.1 m/sec as measured by the T10MW but data still within normal limits. Foot drop was detected as well as decreased dorsiflexion at the level of the right ankle. The pelvis shows slight hiking on the right and there is a marginal trunk lean to the left possibly to allow for clearance of the right lower extremity. Arm swing is normal and reciprocal.
Clinical Impressions[edit | edit source]
PT Diagnosis: 18 year old male recently diagnosed with Charcot-Marie-Tooth Disease presenting with decreased muscle strength and endurance, increased muscle fatiguability, balance and sensory deficits, gait abnormalities, and pain in lower extremities. Condition is affecting patient’s ability to participate in sport and get to and from classes.
Problem List:
- Decreased muscle strength and endurance
- Increased muscle fatiguability
- Minimal balance deficits
- Gait abnormalities (tripping, foot drop, etc.)
- Pain in lower extremities
Intervention[edit | edit source]
Due to weakness found in the patients ankle dorsiflexors, this could lead to increased tone and tightening of the gastrocnemius and soleus muscles as well as fibrosis of the achilles tendon. These changes could all put the patient at a high risk for developing ankle contractures (skalsky). In order to avoid these changes and maintain appropriate joint range of motion the patient was prescribed to do a minimum of 2 to 3 hours a day of standing or walking as well as some passive stretching exercises 2-3 times per day for the structures at risk for contractures (skalsky). Passive range of motion exercises have been shown to be effective in delaying the development of contractures in CMT (skalsky).
With walking, because the patient has expressed tripping issues that can be attributed to drop foot and sensory deficits, a custom ankle-foot orthoses (AFO) has been recommended. There are many benefits in wearing an AFO for those with CMT, including improvement in walking economy by reducing the energy cost of walking compared to just wearing shoes (Menotti). AFO’s have also been shown to increase gait velocity, increase comfort, decrease pain, improve lower extremity control during walking, and very importantly increase dorsiflexion and therefore reducing foot drop in patients with CMT (Phillips, McCorquodale, Ramdharry). On top of this recommendation, the patient was also provided with gait training and education in order to allow for normal gait biomechanics in the hopes of decreasing compensatory muscle recruitment and improving energy efficiency (Dufek).
As the patient presented with symptoms of muscle fatigue, and with overwork weakness being a common finding in CMT, it was decided that education on energy conservation techniques would be one of the focal points during treatment (McCorquodale). The education included advice on pacing himself with activities and ensuring adequate rest periods, planning out the most efficient walking routes while on campus, and making sure he wears his custom AFO once received in order to optimize his biomechanics and improve his walking efficiency. Unfortunately, it was also recommended that the patient discontinues playing competitive soccer in order to prioritize other activities of daily living from an energy cost standpoint. Lastly, because the patient reported difficulties with sleep, and because it is known that CMT may predispose patients to sleep conditions such as obstructive sleep apnoea and restless leg syndrome, it was decided that the patient be referred out to a sleep specialist (Boentert).