Congenital torticollis: Difference between revisions
No edit summary |
No edit summary |
||
| (65 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Nikki Rommers|Nikki Rommers]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Nikki Rommers|Nikki Rommers]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | |||
== Introduction/ Description == | |||
[[File:Torticollis 1.jpg|alt=|right|frameless]] | [[File:Torticollis 1.jpg|alt=|right|frameless]] | ||
Congenital torticollis | [[Congenital and Acquired Neuromuscular and Genetic Disorders|Congenital]] torticollis (CMT) is a condition in infants commonly diagnosed at or soon after birth. The term torticollis is derived from the Latin word ''tortus'', meaning <nowiki>''twisted''</nowiki> and ''collum'' meaning <nowiki>''neck.''</nowiki> This condition is, therefore, also known as twisted neck or wry neck. | ||
CMT occurs when there is reduced length and increased tone of [[sternocleidomastoid]] (SCM) on one side. Infants present with lateral flexion on the ipsilateral side (i.e. the side where the SCM is affected) and contralateral rotation.<ref name=":2">Ellwood J, Draper-Rodi J, Carnes D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7288527/ The effectiveness and safety of conservative interventions for positional plagiocephaly and congenital muscular torticollis: a synthesis of systematic reviews and guidance]. Chiropractic & manual therapies. 2020 Dec;28(1):1-1.</ref> | |||
Treatment approaches for CMT include | Treatment approaches for CMT include:<ref name=":2" /> | ||
* manual therapy (e.g. therapist-led stretching exercises) | |||
* repositioning therapy (e.g. tummy time) | |||
* botulinum toxin (botox) / surgery may be necessary for more severe cases that do not resolve | |||
Secondary changes associated with CMT can include:<ref name=":2" /> | |||
= | |||
* cranial asymmetry ([[plagiocephaly]]) | |||
* functional problems, such as difficulty breastfeeding | |||
== Epidemiology == | == Epidemiology == | ||
* Torticollis in infants is most commonly caused by CMT<ref>Amaral DM, Cadilha RP, Rocha JA, Silva AI, Parada F. Congenital muscular torticollis: where are we today? A retrospective analysis at a tertiary hospital. Porto biomedical journal. 2019 May;4(3). </ref> | |||
* CMT is the third most common congenital musculoskeletal condition in newborns - its incidence ranges from 0.3% to 19.7%<ref>Kuo AA, Tritasavit S, Graham JM. Congenital muscular torticollis and positional plagiocephaly. Pediatr Rev. 2014;35(2):79-87; quiz 87. </ref> | |||
* It has been associated with upper [[Structure and Function of the Cervical Spine|cervical spine]] dysfunction and has been called a "kinetic imbalance due to suboccipital strain"<ref name=":2" /> | |||
== Clinically Relevant Anatomy == | |||
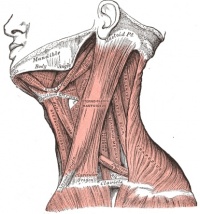
[[File:Grays 385.JPEG|Sternocleidomastoid muscle|alt=|right|frameless|214x214px]]The [[Sternocleidomastoid|sternocleidomastoid muscle]] has a [[Sternum|sternal]] and [[Clavicula|clavicular]] head. The sternal head originates at the [[Sternum|manubrium sterni]]<ref>Gray H. [https://books.google.co.in/books?hl=en&lr=&id=9zBKAQAAMAAJ&oi=fnd&pg=PR30&dq=Gray%E2%80%99s+Anatomy+of+the+Human+Body&ots=XQbFp5nsga&sig=nfBceFQEHppdeFNtD4DGno09Hjs&redir_esc=y#v=onepage&q=Gray%E2%80%99s%20Anatomy%20of%20the%20Human%20Body&f=false Anatomy of the human body.] Lea & Febiger; 1878.</ref> moving superiorly, laterally and posteriorly. The clavicular head originates at the medial third of the clavicle and runs vertically upward. It inserts at the mastoid process and enables ipsilateral lateral flexion and contralateral rotation. SCM also extends the upper part of the cervical spine and flexes the lower part.<ref name="p6">Alison Middleditch MC, Jean Oliver MC. [https://books.google.co.in/books?hl=en&lr=&id=y5f_UYKL28UC&oi=fnd&pg=PR7&dq=Middleditch+A,+Oliver+J.+Functional+anatomy+of+the+spine:+second+edition.+Edinburgh%3B+New+York:+Elsevier&ots=pJziT5ywB7&sig=74BcHr3OJogFjpiaOjaDWmrg8S0&redir_esc=y#v=onepage&q=Middleditch%20A%2C%20Oliver%20J.%20Functional%20anatomy%20of%20the%20spine%3A%20second%20edition.%20Edinburgh%3B%20New%20York%3A%20Elsevier&f=false Functional anatomy of the spine]. Elsevier Health Sciences; 2005 Sep 30.</ref> | |||
== Aetiology == | |||
As mentioned, CMT is caused by an imbalance in the SCM, but its aetiology is still being explored. There are a number of suggested causes, including ischaemia, trauma during childbirth, intrauterine malposition.<ref name=":1">Gundrathi J, Cunha B, Mendez MD. Congenital Torticollis. 2023 Jan 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 31747185. </ref> | |||
CMT caused by intrauterine deformation may be associated with limited space in utero (e.g. in first pregnancies, multiple births), decreased amniotic fluid volume, or uterine compression syndrome.<ref name=":1" /> | |||
== Pathophysiology == | == Pathophysiology == | ||
A fibrous band forms in the SCM muscle in infants with CMT. This may be due to muscle injury, i.e. prolonged compression and stretching of the muscle. Histological studies also found: oedema, muscle fibre degeneration, and fibrosis in babies with CMT (which suggests the presence of compartment syndrome).<ref name=":1" /> | |||
== Clinical Presentation == | |||
* Unilateral contraction of the SCM causing a lateral flexion towards the affected side with slight rotation of the chin to the contralateral side.<ref name="p1">Haque S, Shafi BB, Kaleem M. [https://pubs.rsna.org/doi/full/10.1148/rg.322105143 Imaging of Torticollis in Children]. RadioGraphics. Mar 2012; 32(2): 558-571</ref><ref name="p7">Petronic I, Brdar R, Cirovic D, Nikolic D, Lukac M, Janic D, et al. [https://europepmc.org/article/med/20485220 Congenital muscular torticollis in children: distribution, treatment duration and out come]. European journal of physical and rehabilitation medicine. 2009 Dec 15;46(2):153-7.</ref><ref name="p8">Ta JH, Krishnan M. [https://www.sciencedirect.com/science/article/abs/pii/S0165587612004041 Management of congenital muscular torticollis in a child: a case report and review]. International journal of pediatric otorhinolaryngology. 2012 Nov 1;76(11):1543-6.</ref> | |||
* Affected side may seem excessively stronger than the contralateral side | |||
** this causes an imbalance in the neck muscles | |||
** the lateral head righting on the contralateral side is weaker than the affected side<ref name="p3">Öhman A, Mårdbrink EL, Stensby J, Beckung E. [https://www.tandfonline.com/doi/abs/10.3109/09593985.2010.536305 Evaluation of treatment strategies for muscle function in infants with congenital muscular torticollis.] Physiotherapy Theory and Practice. 2011; 27(7): 463-470 (Level of Evidence 2)</ref> | |||
* In some cases, the shoulder may be elevated on the affected side<ref name="p8" /> | |||
* Can be accompanied by [[plagiocephaly]]<ref name=":0">Kaplan SL, Coulter C, Fetters L. [https://journals.lww.com/pedpt/Fulltext/2018/10000/Physical_Therapy_Management_of_Congenital_Muscular.2.aspx Physical Therapy Management of Congenital Muscular Torticollis: An Evidence-Based Clinical Practice Guideline] FROM THE SECTION ON PEDIATRICS OF THE AMERICAN PHYSICAL THERAPY ASSOCIATION. Pediatric Physical Therapy. 2013 Dec 1;25(4):348-94. </ref> | |||
CMT is | When CMT is left untreated, it can cause: | ||
* fibrosis of the cervical musculature - this is associated with progressive limitations in head movements | |||
* asymmetry of craniofacial structures | |||
* compensatory [[scoliosis]] - this tends to get worse with age<ref name="p8" /> | |||
There are three types of congenital muscular torticollis:<ref name=":1" /><ref name=":0" /> | |||
# Postural | # Postural - occurs in 20% of cases - the infant will have a postural preference, but they do not have any muscle restrictions or reductions in passive range of motion | ||
# Muscular | # Muscular - occurs in 30% of cases - the infant will have SCM tightness and a reduction in passive range of motion | ||
# Sternocleidomastoid mass | # Sternocleidomastoid mass - occurs in 50% of cases - the infant will have thickening of SCM and restricted passive range of motion | ||
Postural CMT is the mildest form of CMT. If identified early, postural CMT is associated with shorter treatment times. Infants with sternocleidomastoid mass and who are identified later (after 3-6 months) tend to require longer intervention and may need more invasive management.<ref name=":0" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
*[http://www.physio-pedia.com/Adult-onset_Idiopathic_Torticollis Acquired torticollis]<ref name="p1" /> | *[http://www.physio-pedia.com/Adult-onset_Idiopathic_Torticollis Acquired torticollis]<ref name="p1" /> | ||
*Occipitoatlantal | *Occipitoatlantal fusion<ref name="p1" /> | ||
*[http://www.physio-pedia.com/Klippel-Feil_syndrome Klippel-Feil syndrome]<ref name="p1" /> | *[http://www.physio-pedia.com/Klippel-Feil_syndrome Klippel-Feil syndrome]<ref name="p1" /> | ||
* | *Sternocleidomastoid tumour: palpable mass on the sternocleidomastoid muscle, this must be confirmed with ultrasonography<ref name="p4">Tatli B, Aydinli N, Caliskan M, Ozmen M, Bilir F, Acar G. [https://www.sciencedirect.com/science/article/abs/pii/S0887899405003437 Congenital muscular torticollis: evaluation and classification.] Pediatric Neurology. 2006;34(1): 41-44 (Level of Evidence 2)</ref> | ||
*[http://www.physio-pedia.com/Scoliosis Scoliosis]<ref name="p8" /> | *[http://www.physio-pedia.com/Scoliosis Scoliosis]<ref name="p8" /> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Diagnosis of CMT can usually be made based on the clinical presentation. The following clinical features may be present:<ref name=":0" /> | |||
* reduced neck range of motion | |||
* palpable SCM mass | |||
* head position preference | |||
* plagiocephaly | |||
However, some cases will require complementary diagnostic tests. In 50% of cases, infants are diagnosed before two months of age. Parents are often the ones to identify CMT.<ref name=":1" /> | |||
* Ultrasonography (US) is the most frequently used form of imaging, especially for neonates | |||
** it is useful for assessing neck masses, pseudo-tumour | |||
** useful for monitoring/evaluation post-treatment | |||
* Magnetic resonance imaging (MRI) may be used to rule out non-muscular causes | |||
== Outcome Measures == | |||
* Cervical range of movement testing | |||
* Cervical range of movement testing | * Muscle Function Scale<ref>Öhman AM, Nilsson S, Beckung ER. [https://www.tandfonline.com/doi/abs/10.1080/09593980802686904 Validity and reliability of the muscle function scale, aimed to assess the lateral flexors of the neck in infants.] Physiotherapy theory and practice. 2009 Jan 1;25(2):129-37.</ref> | ||
== Examination == | == Examination == | ||
The assessment for CMT includes: | |||
* passive cervical range of motion with arthrodial goniometer | |||
* active range of motion | |||
* global assessment | |||
* neurological, auditory and visual function assessments to rule out other conditions<ref name=":1" /> | |||
Identification of [[The Flag System|red flags]] is essential. These include: poor visual tracking; abnormal muscle tone; other features inconsistent with CMT; poor progress with treatment. If you identify these features, appropriate onward referral is necessary.<ref name=":0" /> | |||
== Treatment == | |||
There is no standardised treatment for CMT, but with appropriate interventions, it has been found that 90 to 95% of infants will improve before the age of 1 year. If treatment is commenced before 6 months, 97% of infants will improve.<ref name=":1" /> | |||
== Physiotherapy Management == | |||
Physiotherapy (stretching, strengthening and developmental facilitation) and aggressive repositioning are first-line treatments. Helmet therapy may be considered for infants with moderate to severe and persisting asymmetry. | |||
=== '''Education''' === | |||
Education, guidance and support can reassure and help parents. It is important to educate parents/caregivers on positioning and handling skills to encourage active neck rotation towards the affected side and to discourage side flexion to the affected side<ref name="p3" /><ref name="p4" /> (e.g. during feeding).<ref name=":3">Eskay K. Torticollis and Plagiocephaly Course. Plus, 2023.</ref> | |||
=== '''Manual Stretching''' === | |||
Manual stretches are an important part of treatment. Manual stretches include side flexion and lateral rotation. It is necessary to show the caregiver how to stabilise and correctly position their hands for each stretch. Please note that stretching techniques are contraindicated in infants diagnosed with Klippel-Feil syndrome. | |||
==== Passive ROM Lateral Neck Flexion ==== | |||
The following stretch is useful to encourage lateral flexion of the neck: | |||
* hold infant's shoulder | |||
* perform side tilt until you feel a gentle stretch | |||
* never force the stretch | |||
* infant should not be crying, but might be fussy, so try to keep them distracted | |||
* can perform supine, or lying on your lap | |||
* hold stretch for 30 seconds | |||
* perform this 3-6 times a day (e.g. every diaper change)<ref name=":3" /> | |||
==== Passive ROM Cervical Rotation ==== | |||
The following stretch is useful to encourage cervical rotation: | |||
* rotate to the infant's non-preferred side | |||
* place your hand on their cheek | |||
* block their opposite shoulder and rotate them | |||
* the goal is to get their chin over the top of their shoulder | |||
* can be performed supine or while being held<ref name=":3" /> | |||
<nowiki>**</nowiki> This short video by Baby Movement Tips shows stretching techniques.{{#ev:youtube|LxGenW5EHxU|600}}<ref>Baby Movement Tips. Congenital Torticollis Stretches. Available from:https://www.youtube.com/watch?v=LxGenW5EHxU&t=5s [last accessed 11/28/2021]</ref> | |||
=== Kinesio Taping === | |||
Kinesio taping is an alternative intervention for CMT. It has been suggested that kinesio taping might decrease treatment duration for CMT<ref name="p6" /> and that it can have an immediate effect on muscular imbalance in children with CMT.<ref>Öhman AM. [https://www.sciencedirect.com/science/article/abs/pii/S1934148212001980 The immediate effect of kinesiology taping on muscular imbalance for infants with congenital muscular torticollis.] PM&R. 2012 Jul 1;4(7):504-8.</ref><br>To apply kinesio tape to the SCM: on the affected side, place tape from insertion to origin of SCM with 5-10% tension; on the unaffected side place tape from origin to insertion with 10-15% tension.<ref name="p6" /> | |||
=== '''Home Programme''' === | |||
There are certain measures that caregivers can take at home to help their child with CMT: | |||
* place toys/decorations to encourage infant to turn to other side | |||
* position the crib or changing table, so the infant must turn to the other side to see / interact with caregivers | |||
* Tubular Orthosis for Torticollis (T.O.T) collar<ref>Russo KJ, Fragala MA. [https://journals.lww.com/pedpt/citation/2001/13040/use_of_the_tot_collar_in_conjunction_with.45.aspx USE OF THE TOT COLLAR IN CONJUNCTION WITH TRADITIONAL INTERVENTION FOR A CHILD WITH TORTICOLLIS]. Pediatric Physical Therapy. 2001 Dec 1;13(4):204.</ref> | |||
This video below shows how to use a T.O.T collar.{{#ev:youtube|uLTv1_j1eMQ|600}}<ref>My Torticollis Baby. How to Apply TOT Collar (used for Torticollis). Available from: https://www.youtube.com/watch?v=uLTv1_j1eMQ&t=1s [last accessed 11/28/2021]</ref> | |||
== Medical Management == | == Medical Management == | ||
If conservative treatment is not successful botox<ref name=":0" /> or surgical options may be considered. | If conservative treatment is not successful, botox<ref name=":0" /> or surgical options may be considered. | ||
Surgical may be indicated for the following:<ref name=":1" /> | |||
* no improvement after six months of manual stretching | |||
* there is a deficit of more than 15 degrees in passive rotation and lateral bending | |||
* tight muscular band is present | |||
* there is a tumour in SCM | |||
Surgical options for torticollis include: unipolar/ bipolar sternocleidomastoids muscle lengthening; "Z" lengthening, and radical resection of SCM.<ref name=":1" /> | |||
== Resources | == Resources == | ||
For a comprehensive look at CMT and evidence-based physiotherapy management: | For a comprehensive look at CMT and evidence-based physiotherapy management: | ||
[https://journals.lww.com/pedpt/Fulltext/ | [https://journals.lww.com/pedpt/Fulltext/2018/10000/Physical_Therapy_Management_of_Congenital_Muscular.2.aspx Physical Therapy Management of Congenital Muscular Torticollis: An Evidence-Based Clinical Practice Guideline] | ||
== References == | == References == | ||
| Line 116: | Line 159: | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:Paediatrics - Conditions]] | [[Category:Paediatrics - Conditions]] | ||
[[Category:Congenital Conditions]] | |||
[[Category:Course Pages]] | |||
Latest revision as of 02:43, 19 April 2023
Introduction/ Description[edit | edit source]
Congenital torticollis (CMT) is a condition in infants commonly diagnosed at or soon after birth. The term torticollis is derived from the Latin word tortus, meaning ''twisted'' and collum meaning ''neck.'' This condition is, therefore, also known as twisted neck or wry neck.
CMT occurs when there is reduced length and increased tone of sternocleidomastoid (SCM) on one side. Infants present with lateral flexion on the ipsilateral side (i.e. the side where the SCM is affected) and contralateral rotation.[1]
Treatment approaches for CMT include:[1]
- manual therapy (e.g. therapist-led stretching exercises)
- repositioning therapy (e.g. tummy time)
- botulinum toxin (botox) / surgery may be necessary for more severe cases that do not resolve
Secondary changes associated with CMT can include:[1]
- cranial asymmetry (plagiocephaly)
- functional problems, such as difficulty breastfeeding
Epidemiology[edit | edit source]
- Torticollis in infants is most commonly caused by CMT[2]
- CMT is the third most common congenital musculoskeletal condition in newborns - its incidence ranges from 0.3% to 19.7%[3]
- It has been associated with upper cervical spine dysfunction and has been called a "kinetic imbalance due to suboccipital strain"[1]
Clinically Relevant Anatomy[edit | edit source]
The sternocleidomastoid muscle has a sternal and clavicular head. The sternal head originates at the manubrium sterni[4] moving superiorly, laterally and posteriorly. The clavicular head originates at the medial third of the clavicle and runs vertically upward. It inserts at the mastoid process and enables ipsilateral lateral flexion and contralateral rotation. SCM also extends the upper part of the cervical spine and flexes the lower part.[5]
Aetiology[edit | edit source]
As mentioned, CMT is caused by an imbalance in the SCM, but its aetiology is still being explored. There are a number of suggested causes, including ischaemia, trauma during childbirth, intrauterine malposition.[6]
CMT caused by intrauterine deformation may be associated with limited space in utero (e.g. in first pregnancies, multiple births), decreased amniotic fluid volume, or uterine compression syndrome.[6]
Pathophysiology[edit | edit source]
A fibrous band forms in the SCM muscle in infants with CMT. This may be due to muscle injury, i.e. prolonged compression and stretching of the muscle. Histological studies also found: oedema, muscle fibre degeneration, and fibrosis in babies with CMT (which suggests the presence of compartment syndrome).[6]
Clinical Presentation[edit | edit source]
- Unilateral contraction of the SCM causing a lateral flexion towards the affected side with slight rotation of the chin to the contralateral side.[7][8][9]
- Affected side may seem excessively stronger than the contralateral side
- this causes an imbalance in the neck muscles
- the lateral head righting on the contralateral side is weaker than the affected side[10]
- In some cases, the shoulder may be elevated on the affected side[9]
- Can be accompanied by plagiocephaly[11]
When CMT is left untreated, it can cause:
- fibrosis of the cervical musculature - this is associated with progressive limitations in head movements
- asymmetry of craniofacial structures
- compensatory scoliosis - this tends to get worse with age[9]
There are three types of congenital muscular torticollis:[6][11]
- Postural - occurs in 20% of cases - the infant will have a postural preference, but they do not have any muscle restrictions or reductions in passive range of motion
- Muscular - occurs in 30% of cases - the infant will have SCM tightness and a reduction in passive range of motion
- Sternocleidomastoid mass - occurs in 50% of cases - the infant will have thickening of SCM and restricted passive range of motion
Postural CMT is the mildest form of CMT. If identified early, postural CMT is associated with shorter treatment times. Infants with sternocleidomastoid mass and who are identified later (after 3-6 months) tend to require longer intervention and may need more invasive management.[11]
Differential Diagnosis[edit | edit source]
- Acquired torticollis[7]
- Occipitoatlantal fusion[7]
- Klippel-Feil syndrome[7]
- Sternocleidomastoid tumour: palpable mass on the sternocleidomastoid muscle, this must be confirmed with ultrasonography[12]
- Scoliosis[9]
Diagnostic Procedures[edit | edit source]
Diagnosis of CMT can usually be made based on the clinical presentation. The following clinical features may be present:[11]
- reduced neck range of motion
- palpable SCM mass
- head position preference
- plagiocephaly
However, some cases will require complementary diagnostic tests. In 50% of cases, infants are diagnosed before two months of age. Parents are often the ones to identify CMT.[6]
- Ultrasonography (US) is the most frequently used form of imaging, especially for neonates
- it is useful for assessing neck masses, pseudo-tumour
- useful for monitoring/evaluation post-treatment
- Magnetic resonance imaging (MRI) may be used to rule out non-muscular causes
Outcome Measures[edit | edit source]
- Cervical range of movement testing
- Muscle Function Scale[13]
Examination[edit | edit source]
The assessment for CMT includes:
- passive cervical range of motion with arthrodial goniometer
- active range of motion
- global assessment
- neurological, auditory and visual function assessments to rule out other conditions[6]
Identification of red flags is essential. These include: poor visual tracking; abnormal muscle tone; other features inconsistent with CMT; poor progress with treatment. If you identify these features, appropriate onward referral is necessary.[11]
Treatment[edit | edit source]
There is no standardised treatment for CMT, but with appropriate interventions, it has been found that 90 to 95% of infants will improve before the age of 1 year. If treatment is commenced before 6 months, 97% of infants will improve.[6]
Physiotherapy Management[edit | edit source]
Physiotherapy (stretching, strengthening and developmental facilitation) and aggressive repositioning are first-line treatments. Helmet therapy may be considered for infants with moderate to severe and persisting asymmetry.
Education[edit | edit source]
Education, guidance and support can reassure and help parents. It is important to educate parents/caregivers on positioning and handling skills to encourage active neck rotation towards the affected side and to discourage side flexion to the affected side[10][12] (e.g. during feeding).[14]
Manual Stretching[edit | edit source]
Manual stretches are an important part of treatment. Manual stretches include side flexion and lateral rotation. It is necessary to show the caregiver how to stabilise and correctly position their hands for each stretch. Please note that stretching techniques are contraindicated in infants diagnosed with Klippel-Feil syndrome.
Passive ROM Lateral Neck Flexion[edit | edit source]
The following stretch is useful to encourage lateral flexion of the neck:
- hold infant's shoulder
- perform side tilt until you feel a gentle stretch
- never force the stretch
- infant should not be crying, but might be fussy, so try to keep them distracted
- can perform supine, or lying on your lap
- hold stretch for 30 seconds
- perform this 3-6 times a day (e.g. every diaper change)[14]
Passive ROM Cervical Rotation[edit | edit source]
The following stretch is useful to encourage cervical rotation:
- rotate to the infant's non-preferred side
- place your hand on their cheek
- block their opposite shoulder and rotate them
- the goal is to get their chin over the top of their shoulder
- can be performed supine or while being held[14]
** This short video by Baby Movement Tips shows stretching techniques.
Kinesio Taping[edit | edit source]
Kinesio taping is an alternative intervention for CMT. It has been suggested that kinesio taping might decrease treatment duration for CMT[5] and that it can have an immediate effect on muscular imbalance in children with CMT.[16]
To apply kinesio tape to the SCM: on the affected side, place tape from insertion to origin of SCM with 5-10% tension; on the unaffected side place tape from origin to insertion with 10-15% tension.[5]
Home Programme[edit | edit source]
There are certain measures that caregivers can take at home to help their child with CMT:
- place toys/decorations to encourage infant to turn to other side
- position the crib or changing table, so the infant must turn to the other side to see / interact with caregivers
- Tubular Orthosis for Torticollis (T.O.T) collar[17]
This video below shows how to use a T.O.T collar.
Medical Management[edit | edit source]
If conservative treatment is not successful, botox[11] or surgical options may be considered.
Surgical may be indicated for the following:[6]
- no improvement after six months of manual stretching
- there is a deficit of more than 15 degrees in passive rotation and lateral bending
- tight muscular band is present
- there is a tumour in SCM
Surgical options for torticollis include: unipolar/ bipolar sternocleidomastoids muscle lengthening; "Z" lengthening, and radical resection of SCM.[6]
Resources[edit | edit source]
For a comprehensive look at CMT and evidence-based physiotherapy management:
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Ellwood J, Draper-Rodi J, Carnes D. The effectiveness and safety of conservative interventions for positional plagiocephaly and congenital muscular torticollis: a synthesis of systematic reviews and guidance. Chiropractic & manual therapies. 2020 Dec;28(1):1-1.
- ↑ Amaral DM, Cadilha RP, Rocha JA, Silva AI, Parada F. Congenital muscular torticollis: where are we today? A retrospective analysis at a tertiary hospital. Porto biomedical journal. 2019 May;4(3).
- ↑ Kuo AA, Tritasavit S, Graham JM. Congenital muscular torticollis and positional plagiocephaly. Pediatr Rev. 2014;35(2):79-87; quiz 87.
- ↑ Gray H. Anatomy of the human body. Lea & Febiger; 1878.
- ↑ 5.0 5.1 5.2 Alison Middleditch MC, Jean Oliver MC. Functional anatomy of the spine. Elsevier Health Sciences; 2005 Sep 30.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Gundrathi J, Cunha B, Mendez MD. Congenital Torticollis. 2023 Jan 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 31747185.
- ↑ 7.0 7.1 7.2 7.3 Haque S, Shafi BB, Kaleem M. Imaging of Torticollis in Children. RadioGraphics. Mar 2012; 32(2): 558-571
- ↑ Petronic I, Brdar R, Cirovic D, Nikolic D, Lukac M, Janic D, et al. Congenital muscular torticollis in children: distribution, treatment duration and out come. European journal of physical and rehabilitation medicine. 2009 Dec 15;46(2):153-7.
- ↑ 9.0 9.1 9.2 9.3 Ta JH, Krishnan M. Management of congenital muscular torticollis in a child: a case report and review. International journal of pediatric otorhinolaryngology. 2012 Nov 1;76(11):1543-6.
- ↑ 10.0 10.1 Öhman A, Mårdbrink EL, Stensby J, Beckung E. Evaluation of treatment strategies for muscle function in infants with congenital muscular torticollis. Physiotherapy Theory and Practice. 2011; 27(7): 463-470 (Level of Evidence 2)
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Kaplan SL, Coulter C, Fetters L. Physical Therapy Management of Congenital Muscular Torticollis: An Evidence-Based Clinical Practice Guideline FROM THE SECTION ON PEDIATRICS OF THE AMERICAN PHYSICAL THERAPY ASSOCIATION. Pediatric Physical Therapy. 2013 Dec 1;25(4):348-94.
- ↑ 12.0 12.1 Tatli B, Aydinli N, Caliskan M, Ozmen M, Bilir F, Acar G. Congenital muscular torticollis: evaluation and classification. Pediatric Neurology. 2006;34(1): 41-44 (Level of Evidence 2)
- ↑ Öhman AM, Nilsson S, Beckung ER. Validity and reliability of the muscle function scale, aimed to assess the lateral flexors of the neck in infants. Physiotherapy theory and practice. 2009 Jan 1;25(2):129-37.
- ↑ 14.0 14.1 14.2 Eskay K. Torticollis and Plagiocephaly Course. Plus, 2023.
- ↑ Baby Movement Tips. Congenital Torticollis Stretches. Available from:https://www.youtube.com/watch?v=LxGenW5EHxU&t=5s [last accessed 11/28/2021]
- ↑ Öhman AM. The immediate effect of kinesiology taping on muscular imbalance for infants with congenital muscular torticollis. PM&R. 2012 Jul 1;4(7):504-8.
- ↑ Russo KJ, Fragala MA. USE OF THE TOT COLLAR IN CONJUNCTION WITH TRADITIONAL INTERVENTION FOR A CHILD WITH TORTICOLLIS. Pediatric Physical Therapy. 2001 Dec 1;13(4):204.
- ↑ My Torticollis Baby. How to Apply TOT Collar (used for Torticollis). Available from: https://www.youtube.com/watch?v=uLTv1_j1eMQ&t=1s [last accessed 11/28/2021]