Cubital Tunnel Syndrome: Difference between revisions
m (Text replace - ''''Lead Editors'''' to ''''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}') |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="noeditbox"> | <div class="noeditbox"><br></div> <div class="editorbox"> | ||
'''Original Editors ''' | '''Original Editors ''' | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} - Lindsey Katt, Matt Malone, Greg Propst, Zane Richardson | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} - Lindsey Katt, Matt Malone, Greg Propst, Zane Richardson | ||
</div> | </div> | ||
== Definition/Description<br> == | == Definition/Description<br> == | ||
| Line 24: | Line 16: | ||
Depending on the duration and progression of the disorder, patients with cubital tunnel syndrome will present with similar but specific symptoms (see Table 1).<ref name="Coppieters" /> The most common complaint for any cubital tunnel syndrome patient is paresthesias in the 4th and 5th digits that often wakes them at night.<ref name="Tetro" /> The patient may also report non-painful "snapping" or "popping" during active and passive flexion and extension of the elbow and a Wartenberg sign (abduction of the fifth digit due to weakness of the third palmar interosseous muscle) may also be present. Patients may also notice weakness while pinching, occasional clumsiness, and a tendency to drop things.<ref>ASSH. Cubital Tunnel Syndrome. http://www.assh.org/Public/HandConditions/Pages/CubitalTunnelSyndrome.aspx. Accessed November 1, 2010.</ref><br> | Depending on the duration and progression of the disorder, patients with cubital tunnel syndrome will present with similar but specific symptoms (see Table 1).<ref name="Coppieters" /> The most common complaint for any cubital tunnel syndrome patient is paresthesias in the 4th and 5th digits that often wakes them at night.<ref name="Tetro" /> The patient may also report non-painful "snapping" or "popping" during active and passive flexion and extension of the elbow and a Wartenberg sign (abduction of the fifth digit due to weakness of the third palmar interosseous muscle) may also be present. Patients may also notice weakness while pinching, occasional clumsiness, and a tendency to drop things.<ref>ASSH. Cubital Tunnel Syndrome. http://www.assh.org/Public/HandConditions/Pages/CubitalTunnelSyndrome.aspx. Accessed November 1, 2010.</ref><br> | ||
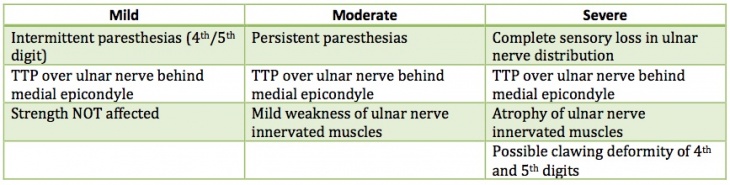
[[Image:Symptom chart II.jpg|thumb|740x185px|Table 1 - Modified from McGowan's grading system found in Coppieters et al]]<br> | [[Image:Symptom chart II.jpg|thumb|center|740x185px|Table 1 - Modified from McGowan's grading system found in Coppieters et al]]<br> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Revision as of 00:27, 8 July 2013
Original Editors
Top Contributors - Lindsey Katt, Greg Propst, Laura Ritchie, Adam West, Rani Sileghem, Admin, Scott Cornish, Kim Jackson, Uchechukwu Chukwuemeka, Boris Alexandra, Anas Mohamed, Vidya Acharya, Zane Richardson, Johnathan Fahrner, WikiSysop, Rachael Lowe, Matthew Malone, Wanda van Niekerk, Amanda Ager, Scott Brown, Jeremy Brady, Scott Buxton and 127.0.0.1 - Lindsey Katt, Matt Malone, Greg Propst, Zane Richardson
Definition/Description
[edit | edit source]
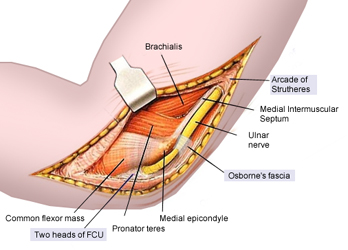
Cubital tunnel syndrome (CBTS) is a progressive entrapment neuropathy of the ulnar nerve at the medial aspect of the elbow. The ulnar nerve, which is a motor and sensory nerve, is formed from the medial cord of the brachial plexus, which originates from nerve roots C8 and T1.[1][2][3] The ulnar nerve travels down the posterior aspect of the arm to eventually traverse posterior to the medial epicondyle through an area known as the cubital tunnel. The cubital tunnel extends from the medial epicondyle of the humerus to the olecranon process of the ulna.[4] The nerve runs superficial to the ulnar collateral ligament (UCL) and deep to the aponeurotic attachment of the flexor carpi ulnaris (FCU), which is also known as Osborne’s ligament. Once the ulnar nerve reaches the proximal border of Osborne’s ligament it is located in the cubital tunnel.
Epidemiology /Etiology[edit | edit source]
Cubital tunnel syndrome is the second most commonly reported upper extremity entrapment neuropathy and is the most common ulnar nerve neuropathy.[5][6] Risk factors include: head injuries with upper extremity flexion contractures, age > 40, overhead throwers, work that involves prolonged periods of elbow flexion such as holding a telephone, and resting elbows on a hard surface.[3][7][8] Entrapment can occur at multiple levels in the cubital tunnel including: the Arcade of Struthers, the medial intermuscular septum, the medial epicondyle, Osborne's ligament and the flexor-pronator aponeurosis.[9] It may be a result of direct or indirect trauma and is vulnerable to traction, friction, and compression. Traction injuries may be the result of longstanding valgus deformity and flexion contractures, but are most common in throwers due to extreme valgus stress placed on the arm.[10] Compression of the nerve at the cubital tunnel may occur due to reactive changes at the UCL, adhesions within the tunnel, hypertrophy of the surrounding musculature, or joint changes.
Characteristics/Clinical Presentation[edit | edit source]
Depending on the duration and progression of the disorder, patients with cubital tunnel syndrome will present with similar but specific symptoms (see Table 1).[5] The most common complaint for any cubital tunnel syndrome patient is paresthesias in the 4th and 5th digits that often wakes them at night.[3] The patient may also report non-painful "snapping" or "popping" during active and passive flexion and extension of the elbow and a Wartenberg sign (abduction of the fifth digit due to weakness of the third palmar interosseous muscle) may also be present. Patients may also notice weakness while pinching, occasional clumsiness, and a tendency to drop things.[11]
Differential Diagnosis[edit | edit source]
Differential diagnoses should include but are not limited to:[3][12][13]
- Cervical Radiculopathy C8-T1 – Motor and sensory deficits in a dermatomal pattern including 4th-5th digits, associated weakness of intrinsic muscles of the hand, and associated painful and often limited cervical range of motion.
- Thoracic Outlet Syndrome – Compression of the structures of the brachial plexus potentially leading to pain, paresthesias, and weakness in arm, shoulder, and neck.[14]
- UCL Insufficiency – Laxity of the UCL can lead to excessive or abnormal movement of structures in or around the cubital tunnel creating new sites of compression.
- Pancoast Tumor - Abnormal growth of tissue on the apex of the lung causing compression of the lower trunk of the brachial plexus.
These diagnoses present similarly to cubital tunnel with pain, paresthesias, and potential weakness; however, symptoms specific to each diagnosis allow the practitioner to rule out the doppelganger and rule in cubital tunnel syndrome. Examples of such symptoms are limited cervical motion and paresthesias in other areas outside the ulnar nerve distribution. It is important for clinicians to correctly identify this diagnosis early, as studies have shown an 88% improvement rate when treated within one year of onset as opposed to 67% improvement if treated after one year.[3][15]
Examination[edit | edit source]
In order to properly diagnose cubital tunnel syndrome, a skilled physical therapist must conduct a proper physical examination including: sensory changes in the ulnar nerve distribution (ulnar ½ of the 4th digit and entirety of the 5th), vague pain, atrophy of the intrinsic muscles of the hand innervated by the ulnar nerve, a neural provocation test of the ulnar nerve, and sparing of the flexor carpi ulnaris muscle.[16] Patients with this diagnosis will also present with a positive Elbow Flexion Test and a positive Tinel test. These special tests are detailed below. Not only is the examination vital to ruling in a correct diagnosis, it allows the practitioner to properly rule out patients with similar presentations.
The Elbow Flexion Test: Typically performed bilaterally with the shoulder in full external rotation and the elbow actively held in sustained maximal flexion for 1 minute with the wrist kept in neutral.[5] Symptoms are produced because maximal elbow flexion reduces the cubital tunnel volume by approximately 55% causing increased neural pressure on the ulnar nerve.[6] Some studies state this test can include additional components such as wrist extension and wrist flexion or sustained maximal elbow flexion for up to 3 minutes.[6] Note, these studies also state that quicker signs of a positive test are more indicative of a true diagnosis of cubital tunnel syndrome. A positive test is reproduction of pain at the medial aspect of the elbow and numbness and tingling in the ulnar distribution on the involved side. This test has a high positive predictive value (0.97), indicating a high probability of cubital tunnel syndrome if positive. Specificity (0.99) Sensitivity (0.75).[17]
Tinel Sign: After locating the ulnar groove posterior to the medial epicondyle of the humerus, the clinician will proceed with percussions (tapping) of the ulnar nerve as it passes through the cubital tunnel.[5][6] The number of percussions vary depending on the research, but four to six taps should be sufficient to elicit symptoms. A positive test is the reproduction of tingling and numbness in the ulnar nerve distribution on the involved side. Practitioners must be cautious with the interpretation of the test because it has been found positive in 24% of asymptomatic subjects and it could be negative for those in the advanced stage of the diagnosis because the nerve is no longer regenerating. Specificity (0.98) Sensitivity (0.70).[18]
The Pressure Provocative Test: The clinician applies pressure on the ulnar nerve at the cubital tunnel with the UE positioned as in the elbow flexion test for 30 seconds. Sensitivity (0.91).[18]
Medical Management (current best evidence)[edit | edit source]
Indications for surgical intervention include moderate muscle weakness without response to conservative treatment after three months and an electrodiagnostic test of less than 39-50 meters per second across the elbow.[18][19][20] There have been several surgical techniques advocated for cubital tunnel syndrome including:[21]
- Simple decompression: A release of Osborne’s ligament done through an incision traversing in a proximal to distal direction throughout the length of the ligament increasing the space in the cubital tunnel. It can be seen in conjunction with a medial epicondylectomy.
- Medial epicondylectomy: An incision is made in a proximal to distal direction parallel to ulnar nerve. The incision exposes the roof of the nerve and the medial epicondyle. The aponeurotic origin of the flexor mass is then dissected allowing partial excision of the epicondyle. The UCL is not compromised in this procedure and it can be done in addition to the simple decompression.
- Anterior transposition (see image[22]): A longitudinal curvilinear incision is made anterior to the medial epicondyle penetrating the roof to expose the nerve. A portion of the medial intermuscular septum is excised which normally provides protection for the ulnar nerve; however, it must be removed in order to expose the nerve for transposition. At the area where the nerve enters the forearm fascia (cubital tunnel), the flexor carpi ulnaris aponeurosis and the deep flexor-pronator aponeurosis are dissected and the nerve is removed from the ulnar groove and moved into the anterior aspect of thearm. Adipose tissue is then sutured from the anterior flap to the medial epicondyle to prevent the nerve from slipping back into the ulnar groove. There are three types of anterior transposition techniques that are named in relation to the flexor-pronator mass:File:Anterior Transposition 3.pngUlnar Nerve Positioned Anterior to Medial Epicondyle while Fascial Flap is Tethered to Dermis to Maintain New Position
o Subcutaneous (above)
o Intermuscular (within)
o Submuscular (below)
As with any surgical procedure it is important for patients to understand the risks and benefits involved before making the decision to proceed with an operative treatment. While the benefits are obvious, the risks are not always apparent to patients so clinicians should be prepared to offer them some amount of insight. Fortunately, serious complications are not common with any of the aforementioned procedures, but they can be susceptible to injuring the medial antebrachial cutaneous nerve, not alleviating CBTS symptoms, and creating new points of compression.[3]
Results found no significant difference in motor nerve-conduction velocities or clinical outcome scores between simple decompression and ulnar nerve transposition meaning the type of surgery is often based on surgeon and patient preference.[23] Simple decompression has shorter operative times and preserves the anatomic location of the ulnar nerve, while ulnar nerve transposition is seen by some as the only way to properly address dynamic compression of the nerve with elbow flexion. Regardless of the type of procedure it is important that the clinician is aware of what tissues were compromised and the anatomic location of the nerve in order to properly treat the post-operative patient.
Physical Therapy Management (current best evidence)[edit | edit source]
Conservative treatment has been shown to have a 90% success rate in low-stage ulnar irritation with symptoms often resolving in 2-3 months.[24] Conservative treatment may include a 4-6 week
period of immobilization with the elbow splinted at 45 degrees of flexion and forearm in neutral rotation, activity modification, modalities and anti-inflammatories for inflammation, soft elbow pads, joint mobilizations, neural flossing [25], neural gliding [26], exercise, and patient education.[14][24] While there is strong evidence in support of splinting (Figure 2[27]), activity modification, and patient education; only low-level evidence supports manual techniques such as nerve glides, joint mobilizations and manipulation, and exercise.[5][13][27] Despite the low-level evidence, improvements have still been seen with manual techniques in patients with cubital tunnel syndrome. Linked in resources is an example of a treatment plan for a patient with CBTS. Please be aware the evidence to support these treatments is low; however, there is some evidence to support it.
In regards to the post-surgical CBTS patient, the general treatment plan should follow a similar pathway as those who have not undergone a surgical procedure. It will be important for the clinician to understand the different surgical techniques, tissues involved, anatomical location of the nerve, and the need to maintain contact and communication with the surgeon. Each procedure will have certain precautions that must be followed to protect the integrity of the nerve and the incision site. Linked in resources are two sample treatment plans for the post-operative patient.
Key Research[edit | edit source]
Svernlov et al.[27]
Medium RCT using three groups to compare effectiveness of elbow night splinting, self-nerve glides, and a control. A 3-month period of self-nerve gliding and instruction about the anatomy of the cubital tunnel including information about provocative positions in those with cubital tunnel syndrome resulted in increased pain-free grip strength, decreased daytime pain, and “normalized” EMG studies but was not significantly different from night splinting with instruction or instruction alone. Conclusion: All groups showed statistically significant improvements in COPM scores and night pain compared to baseline, as well as improvements in grip strength, 5th digit adduction power, and EMG studies but these changes did not reflect a statistically significant change.
Zlowodzki et al.[23]
Meta-Analysis of four RCT comparing simple decompression with anterior ulnar nerve transpositions. There were no significant differences between simple decompression and anterior transposition in terms of the clinical scores in those studies (standard mean difference in effect size = -0.04 [95% CI = -0.36 to 0.28], p = 0.81. Authors did not find significant heterogeneity across the studies. Two reports presented post-operative motor nerve conduction velocities; they showed no significant difference between the procedures. Conclusion: Data suggests that simple decompression is a reasonable alternative to anterior transposition for surgical management of ulnar nerve compression at the elbow.
Resources
[edit | edit source]
Conservative Treatment of Cubital Tunnel Syndrome Example[5][19][27] View Licensing Terms
Post-Surgical Treatment following Ulnar Nerve Transposition #1[28]
Post-Surgical Treatment following Ulnar Nerve Transposition #2 [29]
Clinical Bottom Line[edit | edit source]
With CBTS being the most common ulnar nerve neuropathy and the 2nd most common upper extremity neuropathy, early detection through sound differential diagnosis is key to ensuring best possible patient outcomes. As skilled clinicians we must tailor our treatment to each patient, post-surgical or not, in a manner that follows surgeon precautions and aims to normalize the sensitivity of the nerve, nerve biomechanics, and restores or prevents secondary complications. With insufficient quality evidence to support conservative management of CBTS, we need more randomized controlled trials to determine the effectiveness of current treatment trends.
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ Feindel W, Stratford J. Cubital tunnel compression in tardy ulnar nerve palsy. Can Med Assoc J. 1958;78:351.
- ↑ Osborne GV. The surgical treatment of tardy ulnar neuritis. J Bone Joint Surg Br. 1957;39B:782.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Tetro AM, Pichora DR. Cubital tunnel syndrome and the painful upper extremity. Hand Clin. 1996;12(4):665-677.
- ↑ Wheeless CR. Cubital tunnel syndrome. http://www.wheelessonline.com/ortho/cubital_tunnel_syndrome. Updated June 5, 2010. Accessed November 1, 2010.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Coppieters MW, Bartholomeeusen KE, Stappaerts KH. Incorporating nerve-gliding techniques in the conservative treatment of cubital tunnel syndrome. J Manip Physiol Ther. 2004;27(9):560-568.
- ↑ 6.0 6.1 6.2 6.3 Kuschner SH, Ebramzadeh E, Mitchell S. Evaluation of elbow flexion and tinel tests for cubital tunnel syndrome in asymptomatic individuals. Orthopedics. 2006;29(4):305-308.
- ↑ Bartels RHMA, Verbeek ALM. Risk factors for ulnar nerve compression at the elbow: a case control study. Acta Neurochir Wien. 2007;149:669-674.
- ↑ Oskay D, Meriç A, Kirdi N, Firat T, Ayhan Ç, Leblebicioglu G. Neurodynamic mobilization in the conservative treatment of cubital tunnel syndrome: long-term follow-up of 7 cases. J Manip Physiol Ther. 2010;33(2):156-163.
- ↑ Husain SN, Kaufmann RA. The diagnosis and treatment of cubital tunnel syndrome. Current Orthopaedic Practice. 2008;19(5):470-474.
- ↑ Lee ML, Rosenwasser MP. Chronic elbow instability. Orthop Coin North Am. 1999;30:81-89.
- ↑ ASSH. Cubital Tunnel Syndrome. http://www.assh.org/Public/HandConditions/Pages/CubitalTunnelSyndrome.aspx. Accessed November 1, 2010.
- ↑ Galarza M, Gazzeri R, Gazzeri G, Zuccarello M, Taha J. Cubital tunnel surgery in patients with cervical radiculopathy: double crush syndrome?. Neurosurg Rev. 2009;32(4):471-478.
- ↑ 13.0 13.1 Lund AT, Amadio PC. Treatment of cubital tunnel syndrome: perspectives for the therapist. J Hand Ther. 2006;19:170-179.
- ↑ 14.0 14.1 Office of Communications and Public Liaison. NINDS Thoracic Outlet Syndrome Information Page. http://www.ninds.nih.gov/disorders/thoracic/thoracic.htm. Updated July 14, 2010. Accessed November 1, 2010.
- ↑ Chan RC, Paine KWE, Varughese G. Ulnar neuropathy at the elbow: comparison of simple decompression and anterior transfer. Neurosurgery. 1980;7:545-550.
- ↑ Boucher B, Wainner R, Robertson E. Common disorders of the elbow-forearm complex: part II. Paper presented at: Texas State University DPT PT7559 Lecture; October 13, 2010; San Marcos, TX.
- ↑ Behr CT, Altchek DW. The elbow. Clin Sports Med. 1997;16:681-704.
- ↑ 18.0 18.1 18.2 Novak CB, Lee GW, Mackinnon SE, Lay L. Provacative testing for cubital tunnel syndrome. J Hand Surg Am. 1994;19:817-820.
- ↑ 19.0 19.1 Neal SL, Fields KB. Peripheral nerve entrapment and injury in the upper extremity. Am Fam Physician. 2010;81(2):147-155.
- ↑ Palmer BA, Hughes TB. Cubital Tunnel Syndrome. J Hand Surg, 2010;35A:153-163.
- ↑ Yamamoto K, Shishido T, Masaoka T, Katori Y, Tanaka S. Postoperative clinical results in cubital tunnel syndrome. Orthopedics. 2006;29(4):347-353.
- ↑ Eaton RG, Crowe JF, Parkes JC. Anterior transposition of the ulnar nerve using a non-compressing fasciodermal sling. J Bone Joint Surg Am. 1980;62:820-825.
- ↑ 23.0 23.1 Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89:2592-2598.
- ↑ 24.0 24.1 Shrivastava N, Szabo, RM. Decision making in upper extremity entrapment neuropathies. The Journal of Musculoskeletal Medicine, 2008;25(6), 278-280,284-285,288-289.
- ↑ Optimum Care Providers. 8.1 Upper Limb Ulnar Nerve Mobility. http://www.youtube.com/user/OptimumCareProviders#p/u/107/WtH2QOuwuCU. Updated May 5, 2009. Accessed November 1, 2010.
- ↑ Optimum Care Providers. 8.2 Upper Limb Ulnar Nerve Mobility. http://www.youtube.com/user/OptimumCareProviders#p/u/108/IlrJ7Ibop_4. Updated May 5, 2009. Accessed November 1, 2010.
- ↑ 27.0 27.1 27.2 27.3 Svernlov B, Larsson M, Rehn K, Adolfsson L. Conservative treatment of the cubital tunnel syndrome. J Hand Surg Eur 2009;34E(2):201-207.
- ↑ Lind CC. Ulnar nerve transposition post-operative protocol. http://www.rcmclinic.com/pdfs/elbow-hand/ulnar_nerve_transposition.pdf. Accessed November 1, 2010.
- ↑ Pho C, Godges J. Ulnar Nerve Transposition. http://xnet.kp.org/socal_rehabspecialists/ptr_library/03ElbowRegion/22Elbow-UlnarNerveTransposition.pdf. Accessed November 1, 2010.