Determinants of Health: Difference between revisions
Rachael Lowe (talk | contribs) No edit summary |
m (Removed protection from "Determinants of Health": Retired Course page) |
||
| (41 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | '''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
"Health care is an important determinant of health. Lifestyles are important determinants of health. But... it is factors in the social environment that determine access to health services and influence lifestyle choices in the first place." Director-General Dr Margaret Chan | ''"Health care is an important determinant of health. Lifestyles are important determinants of health. But... it is factors in the social environment that determine access to health services and influence lifestyle choices in the first place."'' WHO Director-General Dr Margaret Chan<ref>Dr Margaret Chan. [http://www.who.int/dg/speeches/2008/20080828/en/ Launch of the final report of the Commission on Social Determinants of Health]. 2008. Accessed online 6 January 2017.</ref> | ||
Many factors combine together to affect the health of individuals and communities. Whether | Many factors combine together to affect the health of individuals and communities. Whether a person is healthy or unhealthy is determined by his/her circumstances and environment. To a large extent, factors such as where we live, the state of our environment, genetics, our income and education level, and our relationships with friends and family all have considerable impacts on health, whereas the more commonly considered factors such as access and use of health care services often have less of an impact. | ||
The determinants of health include: | The context of people’s lives determine their health, and so blaming individuals for having poor health or crediting them for good health is inappropriate. Individuals are unlikely to be able to directly control many of the determinants of health. These determinants, or things that make people healthy or not, include the following and many others: | ||
== Determinants of Health == | |||
The | The range of personal, social, economic and environmental factors that influence health status are known as determinants of health. These can be classified as: | ||
#The social and economic environment | |||
#The physical environment | |||
#The person’s individual characteristics and behaviours | |||
<br> | |||
There are many commonly accepted determinants of health but there is no single definition. The Office of Disease Prevention and Health Promotion ('''ODPHP''') has broadly categorised the determinants of health<ref name="ODPHP">Office of disease prevention and health promotion. [https://www.healthypeople.gov/2020/about/foundation-health-measures/Determinants-of-Health Determinants of Health]. Accessed online 6 January 2017.</ref> and these have been summarised below: | |||
=== 1. Policy-making === | |||
Policies at the local, state and federal level effect individual and population health. Increasing taxes on tobacco sales, for example, can improve population health by reducing the number of people using tobacco products. Unfavorable conditions can result due to substandard policies and programmes, inadequate governance and unfair economic arrangements.<ref>Islam MM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376855/ Social determinants of health and related inequalities: confusion and implications]. Frontiers in public health. 2019 Feb 8;7:11.</ref> | |||
=== 2. Social Factors === | |||
Social and physical determinants of health reflect the conditions of the environment in which people are born, live, learn, play, work and age. Also known as social determinants of health, they impact a wide range of health, functioning and quality-of-life outcomes. They represent economic and political systems, physical and social environments, as well as health service access. Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life.<ref>Palmer RC, Ismond D, Rodriquez EJ, Kaufman JS. Social Determinants of Health: Future Directions for Health Disparities Research. Am J Public Health. 2019;109(S1):S70-S71. </ref> | |||
Examples include: | |||
{| width="100%" | *Availability of resources to meet daily needs, such as educational and job opportunities, living wages or healthful foods | ||
*Social norms and attitudes such as discrimination | |||
*Exposure to crime, violence and social disorder | |||
*Social support and social interactions | |||
*Socioeconomic conditions such as concentrated poverty | |||
*Quality schools | |||
*Transportation options | |||
*Urbanisation and the built environment such as buildings or transportation | |||
*Worksites, schools and recreational settings | |||
<nowiki>**</nowiki> Poor health outcomes are associated with adverse conditions leading to social risk factors<ref>Alderwick H, Gottlieb LM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6554506/ Meanings and misunderstandings: a social determinants of health lexicon for health care systems.] The Milbank Quarterly. 2019 Jun;97(2):407.</ref> | |||
=== 3. Health Services === | |||
Both access to health services and the quality of health services can impact health. Barriers to accessing health services include lack of availability, high cost, lack of insurance coverage and limited language access. These barriers to accessing health services lead to unmet health needs, delays in receiving appropriate care, inability to get preventive services as well as hospitalisations that could have been prevented. | |||
=== 4. Individual Behaviour === | |||
Individual behaviours such as diet, physical activity, alcohol, tobacco and other drug use also play a role in health outcomes. | |||
=== 5. Biology and Genetics === | |||
Some biological and genetic factors affect specific populations more than others. Examples of biological and genetic determinants of health include age, sex, inherited conditions and genetic make-up.<br> | |||
{| width="100%" cellspacing="1" cellpadding="1" border="0" align="center" | |||
|- | |- | ||
| {{#ev:youtube|SXcSjTcrskM}} | | {{#ev:youtube|SXcSjTcrskM}} | ||
| Line 52: | Line 64: | ||
|} | |} | ||
== | == Improving Health Worldwide == | ||
WHO have identified three "common interventions" for improving health conditions worldwide:<ref name=":0">World Health Organization (2013). [http://apps.who.int/iris/bitstream/handle/10665/84213/9789241548625_eng.pdf;jsessionid=97F39CFE3967A7FE93BA46E18B4418E9?sequence=1 The economics of social determinants of health and health inequalities: a resource book (PDF)]. World Health Organization. ISBN 978-92-4-154862-5</ref> | |||
==== 1. Education ==== | |||
A large number of studies have demonstrated a strong link between better education and better health,<ref>Knesebeck O et al. Education and health in 22 European countries. Social Science and Medicine, 2006, 63:1344–1351</ref> and education has been shown to be a reliable predictor of lower mortality rates.<ref>Muller A. Education, income inequality, and mortality: a multiple regression analysis. BMJ, 2002, 324(7328):23–25</ref><ref>Deaton A, Paxson C, eds. Mortality, education, income, and inequality among American cohorts. Chicago, University of Chicago Press, 2001</ref> The probability of being in good or very good health is higher for people with university or post-secondary education.<ref>Hurd M, Kapteyn A. Health, wealth, and the role of institutions. Journal of Human Resources, 2003, 38(2):386–415</ref> | |||
[[Image:Biopsychosocial-model-of-health. | ==== 2. Social Protection ==== | ||
Countries with some sort of social protection (i.e. a safety net or social security system) show improved health and economic outcomes in circumstances where people become unable to earn a living.<ref>Chung H, Muntaner C. Welfare state matters: a typological multilevel analysis of wealthy countries. Health Policy, 2007, 80(2):328–339</ref> | |||
==== 3. Urban Development ==== | |||
The physical environment where communities live has a great impact on the health of the residents.<ref>Chung H, Muntaner C. Welfare state matters: a typological multilevel analysis of wealthy countries. Health Policy, 2007, 80(2):328–339</ref><ref>Thompson S et al. Do urban regeneration programmes improve public health and reduce health inequalities? A synthesis of the evidence from UK policy and practice (1980–2004). Journal of Epidemiology and Community Health, 2006, 60(2):108–115</ref> Factors which have a negative impact on health include overcrowding, damp living conditions and crime (in particular fear of crime). The WHO concludes that health outcomes "are largely determined by the accessibility to adequate housing and to healthy and safe urban environments and by transport conditions".<ref name=":0" /> | |||
== Relevance to Rehabilitation == | |||
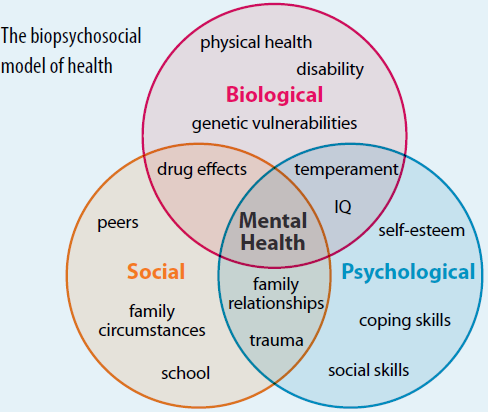
In our contact time with our patients, we spend a lot of time understanding their health and social status. In other words, we explore the determinants that might be affecting their health and in particular ones that we can influence. The model we use to analyse and understand these determinants of health is the [[Biopsychosocial Model|biopsychosocial model]] of health care. | |||
[[Image:Biopsychosocial-model-of-health.PNG|center]] | |||
It is essential that healthcare workers dedicated to improving health increase their effectiveness by addressing the “upstream” causes of health in the community and by engaging in ways to change the broad policies, systems and environments that shape the social and economic conditions that, in turn, so strongly influence health. Swain et al.<ref name="Swain">Swain et al. [http://u21health.org/s/Social-Determinants-of-Health.pdf Health Care Professionals: Opportunities to Address Social Determinants of Health]. 2014. WMJ, 113:6</ref> describe opportunities for the health-care professional to address social determinants of health. They suggest that to be most effective at improving the health of families and communities and to ensure the greatest impact for the investment of resources, health professionals need to expand their repertoire of skills and activities both with their individual patients and in the policy arena. | |||
== Resources == | |||
*[https://www.who.int/publications/m/item/health-in-the-post-2015-development-agenda-need-for-a-social-determinants-of-health-approach Health in the post-2015 development agenda: need for a social determinants of health approach: joint statement of the UN Platform on Social Determinants of Health]. | |||
*[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3863696/ The Social Determinants of Health: It's Time to Consider the Causes of the Causes] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Physical_Activity]] | |||
[[Category:Physical_Activity_Content_Development_Project]] | |||
[[Category:Displaced Persons]] | |||
Latest revision as of 18:55, 5 May 2023
Original Editor - Rachael Lowe
Top Contributors - Rachael Lowe, Wendy Walker, Naomi O'Reilly, Laura Ritchie, Kim Jackson, Jess Bell, Robin Tacchetti, Rucha Gadgil, Tarina van der Stockt, Vidya Acharya, Shaimaa Eldib and Carin Hunter
Introduction[edit | edit source]
"Health care is an important determinant of health. Lifestyles are important determinants of health. But... it is factors in the social environment that determine access to health services and influence lifestyle choices in the first place." WHO Director-General Dr Margaret Chan[1]
Many factors combine together to affect the health of individuals and communities. Whether a person is healthy or unhealthy is determined by his/her circumstances and environment. To a large extent, factors such as where we live, the state of our environment, genetics, our income and education level, and our relationships with friends and family all have considerable impacts on health, whereas the more commonly considered factors such as access and use of health care services often have less of an impact.
The context of people’s lives determine their health, and so blaming individuals for having poor health or crediting them for good health is inappropriate. Individuals are unlikely to be able to directly control many of the determinants of health. These determinants, or things that make people healthy or not, include the following and many others:
Determinants of Health[edit | edit source]
The range of personal, social, economic and environmental factors that influence health status are known as determinants of health. These can be classified as:
- The social and economic environment
- The physical environment
- The person’s individual characteristics and behaviours
There are many commonly accepted determinants of health but there is no single definition. The Office of Disease Prevention and Health Promotion (ODPHP) has broadly categorised the determinants of health[2] and these have been summarised below:
1. Policy-making[edit | edit source]
Policies at the local, state and federal level effect individual and population health. Increasing taxes on tobacco sales, for example, can improve population health by reducing the number of people using tobacco products. Unfavorable conditions can result due to substandard policies and programmes, inadequate governance and unfair economic arrangements.[3]
2. Social Factors[edit | edit source]
Social and physical determinants of health reflect the conditions of the environment in which people are born, live, learn, play, work and age. Also known as social determinants of health, they impact a wide range of health, functioning and quality-of-life outcomes. They represent economic and political systems, physical and social environments, as well as health service access. Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life.[4]
Examples include:
- Availability of resources to meet daily needs, such as educational and job opportunities, living wages or healthful foods
- Social norms and attitudes such as discrimination
- Exposure to crime, violence and social disorder
- Social support and social interactions
- Socioeconomic conditions such as concentrated poverty
- Quality schools
- Transportation options
- Urbanisation and the built environment such as buildings or transportation
- Worksites, schools and recreational settings
** Poor health outcomes are associated with adverse conditions leading to social risk factors[5]
3. Health Services[edit | edit source]
Both access to health services and the quality of health services can impact health. Barriers to accessing health services include lack of availability, high cost, lack of insurance coverage and limited language access. These barriers to accessing health services lead to unmet health needs, delays in receiving appropriate care, inability to get preventive services as well as hospitalisations that could have been prevented.
4. Individual Behaviour[edit | edit source]
Individual behaviours such as diet, physical activity, alcohol, tobacco and other drug use also play a role in health outcomes.
5. Biology and Genetics[edit | edit source]
Some biological and genetic factors affect specific populations more than others. Examples of biological and genetic determinants of health include age, sex, inherited conditions and genetic make-up.
Improving Health Worldwide[edit | edit source]
WHO have identified three "common interventions" for improving health conditions worldwide:[6]
1. Education[edit | edit source]
A large number of studies have demonstrated a strong link between better education and better health,[7] and education has been shown to be a reliable predictor of lower mortality rates.[8][9] The probability of being in good or very good health is higher for people with university or post-secondary education.[10]
2. Social Protection[edit | edit source]
Countries with some sort of social protection (i.e. a safety net or social security system) show improved health and economic outcomes in circumstances where people become unable to earn a living.[11]
3. Urban Development[edit | edit source]
The physical environment where communities live has a great impact on the health of the residents.[12][13] Factors which have a negative impact on health include overcrowding, damp living conditions and crime (in particular fear of crime). The WHO concludes that health outcomes "are largely determined by the accessibility to adequate housing and to healthy and safe urban environments and by transport conditions".[6]
Relevance to Rehabilitation[edit | edit source]
In our contact time with our patients, we spend a lot of time understanding their health and social status. In other words, we explore the determinants that might be affecting their health and in particular ones that we can influence. The model we use to analyse and understand these determinants of health is the biopsychosocial model of health care.
It is essential that healthcare workers dedicated to improving health increase their effectiveness by addressing the “upstream” causes of health in the community and by engaging in ways to change the broad policies, systems and environments that shape the social and economic conditions that, in turn, so strongly influence health. Swain et al.[14] describe opportunities for the health-care professional to address social determinants of health. They suggest that to be most effective at improving the health of families and communities and to ensure the greatest impact for the investment of resources, health professionals need to expand their repertoire of skills and activities both with their individual patients and in the policy arena.
Resources[edit | edit source]
- Health in the post-2015 development agenda: need for a social determinants of health approach: joint statement of the UN Platform on Social Determinants of Health.
- The Social Determinants of Health: It's Time to Consider the Causes of the Causes
References[edit | edit source]
- ↑ Dr Margaret Chan. Launch of the final report of the Commission on Social Determinants of Health. 2008. Accessed online 6 January 2017.
- ↑ Office of disease prevention and health promotion. Determinants of Health. Accessed online 6 January 2017.
- ↑ Islam MM. Social determinants of health and related inequalities: confusion and implications. Frontiers in public health. 2019 Feb 8;7:11.
- ↑ Palmer RC, Ismond D, Rodriquez EJ, Kaufman JS. Social Determinants of Health: Future Directions for Health Disparities Research. Am J Public Health. 2019;109(S1):S70-S71.
- ↑ Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. The Milbank Quarterly. 2019 Jun;97(2):407.
- ↑ 6.0 6.1 World Health Organization (2013). The economics of social determinants of health and health inequalities: a resource book (PDF). World Health Organization. ISBN 978-92-4-154862-5
- ↑ Knesebeck O et al. Education and health in 22 European countries. Social Science and Medicine, 2006, 63:1344–1351
- ↑ Muller A. Education, income inequality, and mortality: a multiple regression analysis. BMJ, 2002, 324(7328):23–25
- ↑ Deaton A, Paxson C, eds. Mortality, education, income, and inequality among American cohorts. Chicago, University of Chicago Press, 2001
- ↑ Hurd M, Kapteyn A. Health, wealth, and the role of institutions. Journal of Human Resources, 2003, 38(2):386–415
- ↑ Chung H, Muntaner C. Welfare state matters: a typological multilevel analysis of wealthy countries. Health Policy, 2007, 80(2):328–339
- ↑ Chung H, Muntaner C. Welfare state matters: a typological multilevel analysis of wealthy countries. Health Policy, 2007, 80(2):328–339
- ↑ Thompson S et al. Do urban regeneration programmes improve public health and reduce health inequalities? A synthesis of the evidence from UK policy and practice (1980–2004). Journal of Epidemiology and Community Health, 2006, 60(2):108–115
- ↑ Swain et al. Health Care Professionals: Opportunities to Address Social Determinants of Health. 2014. WMJ, 113:6