Electrical Stimulation - Its role in upper limb recovery post-stroke
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Rebecca Graham, Grant Burns, Craig Philip, Joshua Tan, Hannah Little, Rucha Gadgil, Kim Jackson, 127.0.0.1, Admin, Rachael Lowe, Venugopal Pawar, Cindy John-Chu, Carina Therese Magtibay, Dinu Dixon, Evan Thomas and Jane Hislop
Introduction and Learning Outcomes[edit | edit source]
Welcome to this online learning resource on the use of functional electrical stimulation (FES) to support recovery of upper limb following a stroke. This interactive learning package has been created by a small group of final year Physiotherapy students from Queen Margaret University as part of the Contemporary and Emerging Issues in Physiotherapy module.
This resource aims:
to provide an interactive learning package for final year students and newly qualified physiotherapists to develop their knowledge and understanding of FES for upper limb recovery following a stroke, and
to provide a resource of key literature and signposting to further reading and content.
Learning Outcomes
The following learning outcomes (LO) have been constructed to support competencies expected of a newly qualified (Band 5) physiotherapist role (ref xxxx). A balance of theory, policy and evidence-base, as well more practical aspects for application of FES has been integrated into the LOs. This choice was based on discussion and feedback with tutors and peers.
By the end of this learning package the user should be able:
LO1: to appraise the guidelines and underpinning literature on the use of FES in stroke upper limb recovery and relate this to your current or future clinical practice setting.
LO2: to discuss the principles, applications and parameters of FES in relation to stroke upper limb recovery.
LO3: to justify the consideration of FES in stroke upper limb assessment and intervention planning.
Layout and Approach
This package should take approximately ten hours to work through however the sections have been designed in a way which enables users to dip in and out to suit their needs. At the start of each section a brief outline of what is covered will be outlined and linked to the above learning outcomes.
A key design of the package is to be interactive. While synthesis and summary of key information has been provided, the user will gain greater benefit by engaging with the directed reading, activities, short quizzes and case study that have been developed to support a deeper learning experience.
Also a range of material has been considered in the design of this package to try and suit most learning styles (VARK xxxx). If you find that a section does not suit then please review the additional resource section at the bottom for alternative options.
The following describes the main sections found below in this resource package.
Introduction
What is FES
When should I use FES
How do I use FES
General
Shoulder Subluxation
Motor control
Conclusion
Further Resources
Context - Why this Topic?
Stroke plays a large part and burden on society (Stroke Association 2015) and is currently the 4th largest cause of mortality in the UK (Stroke Association 2015). Although trends show decreased mortality rates over the last 20 years, it is still the leading cause of adult disability. The UK has approximately 1.2 million stroke survivors with half experiencing disability and 77% with upper limb difficulties (Stroke Association 2015).
In the UK the over 65s population is estimated to grow by 25% by 2020, which is a demographic where stroke incidence is higher. This could potentially lead to even greater numbers of survivors requiring support and rehabilitation from health care professions such as Physiotherapy.
Maintaining and improving people’s functional abilities is a key goal for physiotherapists working with those who have a stroke and FES is a technology that offers the potential to support this (ref xxxx). This goal aligns with current Scottish health and wellbeing policy aimed at driving improved health outcomes for patients (The Scottish Government 2015).
What is Functional Electrical Stimulation[edit | edit source]
This section will cover:
- introduction
- terminology
- physiology
- considerations for use
- ES devices ad parameters
- whats available?
- quiz
Introduction [edit | edit source]
Functional electrical stimulation (FES) is an assistive technology that works by stimulating peripheral nerves and muscles of a weakened part of the body. It activates contraction and relaxation of the muscles that have been affected by an upper motor neuron lesion. The muscles are triggered to contract during an activity, in order to improve function of completing these tasks. FES engages the patient and delivers feedback of a sensory and visual nature, which is said to be beneficial for stroke patients during their recovery and should promote motor re-learning (Dobkin and Dorsch 2013; Kawashima et al. 2013; Howlett et al. 2015; Odstock medical 2015).
Alongside stroke, conditions whereby FES may be effective include Cerebral Palsy, Parkinson’s Disease, Multiple Sclerosis and Spincal Cord Injuires if this is above T12, all of which being upper motor neuron injuries (Odstock medical 2006).
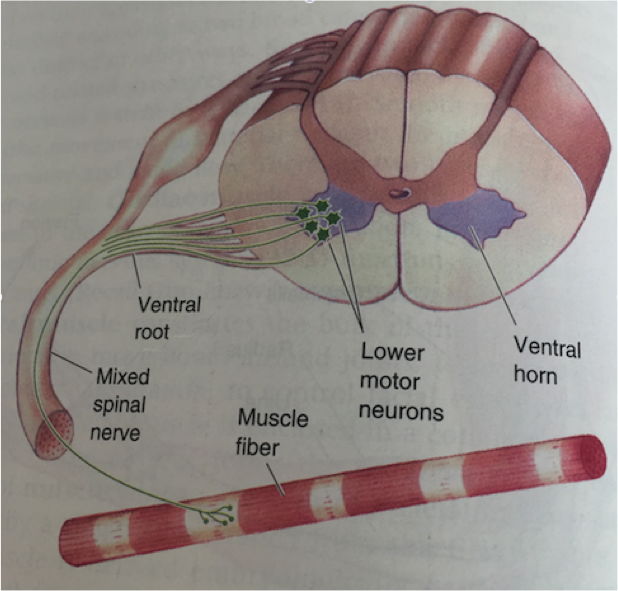
FES is not suitable for lower motor neuron lesions as lower motor neurons directly innervate skeletal muscles via the ventral horn of the spinal cord and are needed for voluntary muscle contraction. They contain both sensory and motor fibres (Odstock Medical 2006; Bear et al. 2007).
(Bear et al. 2007)
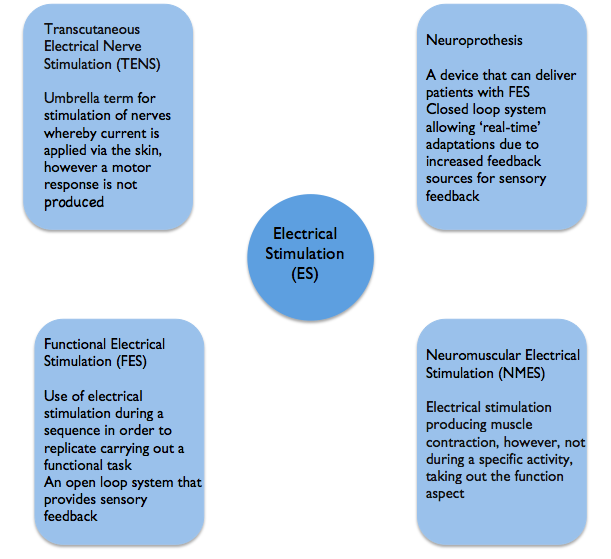
Terminology[edit | edit source]
(Robertson et al. 2006; SSAHPF 2014; Neo Stroke Network 2015)
[edit | edit source]
Physiology[edit | edit source]
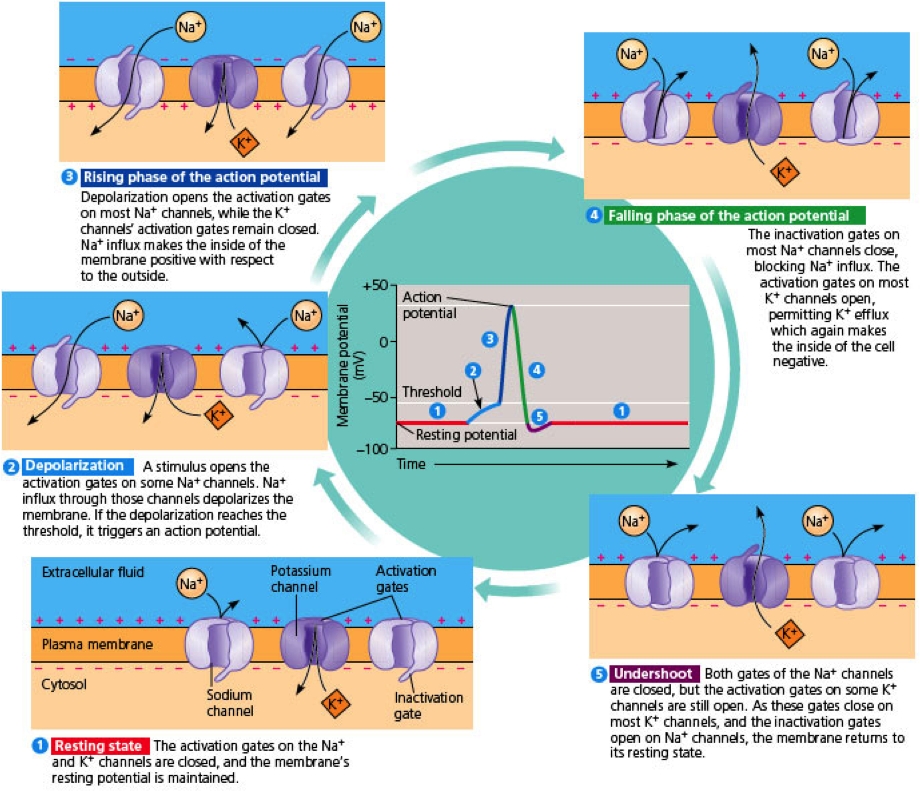
Motor units are electrically stimulated by depolarization of motor axons, or terminal motor nerve braches. When depolarization reaches threshold an action potential occurs due to sodium flowing from extracellular to intracellular space, leading to the contraction of muscle (Neo stroke network 2015).
In FES it is the nerves that are stimulated rather than muscle, as they require a lesser current of that which would be needed to trigger muscles directly. Factors including distance from electrode to nerve fibre, size of motor unit, and surrounding tissue will all have an impact on the number and type of motor units activated.
If FES is effective muscle fibres will change in structure over the course of treatment with type II glycolytic fibres converting to type I oxidative skeletal muscle fibres due to improved resistance to fatigue (Gorman and Peckham 2014). Type II fibres create greater forces however fatigue more quickly, whereas type I fibres produce lesser force however take longer to fatigue (Sheffler and Chae 2007).
In normal physiology, nerve fibre recruitment occurs as described by the Henneman size principle of voluntary motor unit recruitment, whereby fibres with the smallest diameter neurons will be recruited first. When using electrical stimulation, the reverse of this happens, with the largest diameter neurons being the first recruit. This is because they have a lower nerve stimulus threshold (Sheffler 2007).
Ion Movement and Action Potential (Dundee Med Student Notes 2012)
If you require a refresher on the structure and function of motor neurons, visit this short youtube clip to familiarise yourself.
For further revision of physiology please visit the book ‘Principles of Physiology’ by Levy, Koeppen and Stantion (2006).
Chapters of interest:
- chapter 3 – Generation and Conduction of Action Potential (Howard C. Kutchai)
- chapter 4 – Synaptic Transmission (Howard C. Kutchai)
- chapter 9 – Motor System (William D. Willis, Jr)
Considerations for use[edit | edit source]
A limitation of FES is that muscles may fatigue (Thrasher et al. 2005). It is reported that the higher frequency that is selected, the quicker muscle fatigue will set in. Therefore to solve this issue a lower frequency should be selected. (reference)
There is argument for and against whether muscle strengthening can occur once fatigue has set in. It has been suggested that when fatigued, that no advantages can be gained from additional stimulation and therefore you should try to prevent fatigue. The opposite view however suggests that strengthening will only be achieved is the muscle fibre is worked to its maximum.
It appears that strengthening can occur if fatigue is within the muscle fibres due to cellular processes being activated, however is fatigue has resulted from neurotransmitter depletion or propogation failure, the muscle will not be strengthened as the fibre is not being stimulated (Robertson et al. 2006).
Response to continual stimulation may reduce due to the action potential decreasing the distance reached over membrane of the muscle fibre. (reference)
ES Devices and Parameters[edit | edit source]
FES systems include three mechanisms: the control, an electrical stimulator and electrodes which connects the FES with the nervous system (Gorman and Peckham 2014).
The electrical current activates the nerves via electrodes. These can be surface electrodes meaning they are placed on the skin which is the most common and detailed further below; percutaneous electrodes, which penetrate through the skin into the muscle or completely implanted electrodes, which receive stimulation from an external unit.
Surface electrodes
As well as stimulating muscle, surface electrodes may also be used to achieve a reflex action. Surface electrodes appear the most practical however there can be issue with disuse due to the sensory component, which may make stimulation of deeper muscles more difficult. Implanted and percutaneous electrodes can resolve some of these issues but the cost and practicality should be taken into consideration (Ewins and Durham 2005).
Parameters of FES needed when using surface electrodes can differ depending on factors such as material of the electrodes, placement and surface area. An issue with surface electrodes is that there can be difficulty contracting small individual muscles, and to activate deeper muscles, those more superficical must first be activated. Surface electrodes may also cause pain for some patients and it is reported that subcutaneous electrodes are more pleasant (Popaviz 2003).
Two electrodes should always be used however these can be unipolar or bipolar. Unipolar is the term for when one electrode is more active than another, due to their sizes. Biploar electrode placement means they are both the same size meaning the current at each site will be equal (Robertson 2006).
To further familiarise and gain greater understanding regarding use of electrdoes, please read pages 50-58 of Electrotherapy Explained – Princicples and Practice (Robertson et al. 2006).
(Allan and Goodman 2014) (SSAHPF 2014)
Specific parameters for the use of ES within shoulder subluxation and motor control will be detailed below in their specific sections.
What's Available?[edit | edit source]
Odstock medical is one of the main suppliers of FES devices, which vary in design and paramters available. The odstock 4 channel stimulator kit and microstim 2V2 kit are both simple to use in order to allow regular activity in the home environment. They have this in common however differ in output as the 4 channel stimulator can provide alternating or continuous output, unlike the microstim.
The odstock website has further images and descriptions of the FES kits available. Please visit the website to familiarise with the options available. The link is as follows: http://www.odstockmedical.com
Microstim 2V2 Kit (Odstock Medical 2015) '
Channel Stimulation Kit (Odstock Medical 2015)
Quiz[edit | edit source]
https://www.onlinequizcreator.com/what-is-fes/quiz-144398
When should I use Functional Electrical Stimulation[edit | edit source]
When should I use FES?
Functional Electrical Stimulation (FES) can be used in a variety of different ways. This learning package focuses upon the use of FES in improving motor control and in reducing shoulder subluxation. FES can be applied by qualified health professionals including physiotherapists and occupational therapists who are competent in its use. Although this wiki gives a theoretical overview of FES we advise that practical training is performed before applying this as a treatment (Allan and Goodman 2014). This checklist below details what training is required prior to use of FES.
Link to checklist: http://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0004/211819/Using-Electrical-Stimulation-January-2014.pdf
What do Patients need to know?
Patients need to give verbal consent prior to treatment. Patients must be informed of the expected the skin sensation and of the sensation they should not feel. Patients should also be told what to do if they experience these sensations and how to work the FES device if a patient or carer is able to adjust it. It might be worthwhile providing an instruction manual which is in lay terms. Contraindications and precautions should be considered with relevant information explained to patients all this should be documented in patient notes (Allan and Goodman 2014).
Contraindications and Precautions:
To ensure patient safety it is important to consider the contraindications and precautions before using an FES device. Please take time to read these linked documents taking notes as you go.
Using Electrical Stimulation A Guideline for Health Professionals
Page 3
http://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0004/211819/Using-Electrical-Stimulation-January-2014.pdf
Scottish Stroke Allied Health Professionals Forum Use of Electrical Stimulation Following Stroke A Consensus Statement
Page 19
http://www.chss.org.uk/documents/2014/10/electrical-stimulation-consensus-statement-ssahpf-pdf.pdf
Referral Criteria OML Learning Through Technology Precautions
Page 2
http://www.odstockmedical.com/sites/default/files/referral-criteria_0.pdf
Contraindications Quiz:
Once you have completed the reading above complete the questions below:
https://www.onlinequizcreator.com/fes-contraindications-and-precautions/quiz-144392
Outcome Measures:
Motor Assessment Scale:
One outcome measure which could be used to assess functional improvement whilst using an FES device is the Motor assessment scale(MAS). MAS is an outcome measure which focuses upon functional motor activities. It has specific sections for Supine to side lying, Supine to sitting over side of bed, Balanced sitting, Sitting to standing, Walking, Upper-arm function, Hand movements, Advanced hand activities and general tonus. Each of these are scored from 0-6. A score of six is the optimal motor score in that area (CARR et al 1985a).
File:Motor Assessment Scale.pdf
Advantages:
• A 2004 study by LANNIN found that the upper limb section had good reliability as well as good Concurrent and construct validity for stroke recovery (Lannin 2003).
• It is an easy scale to use which takes a short time to complete (CARR et al 1985 b)
• The MAS is recommended as a standard physiotherapy outcome measure after stroke over the Functional Independence Measure and other outcome measures (Williams et al 2001a).
Limitations:
• Although MAS has a section upon UL it was not designed to be upper limb specific.
• Despite having a high score in upper limb sections patients may not be able to perform high level functional skills (Williams et al 2001b)
• General tonus is difficult to assess reliably (Salter et al 2013)
Wolf Motor Function Test:
The Wolf Motor Function Test is a time measured outcome measure which aims to assess how quickly functional upper limb tasks can be performed. Patients are given 120 seconds to complete each task before the task is marked as incomplete. Each of these are scored from 0 to 5. Five being the best score achievable (WOLF ET AL 2005a). 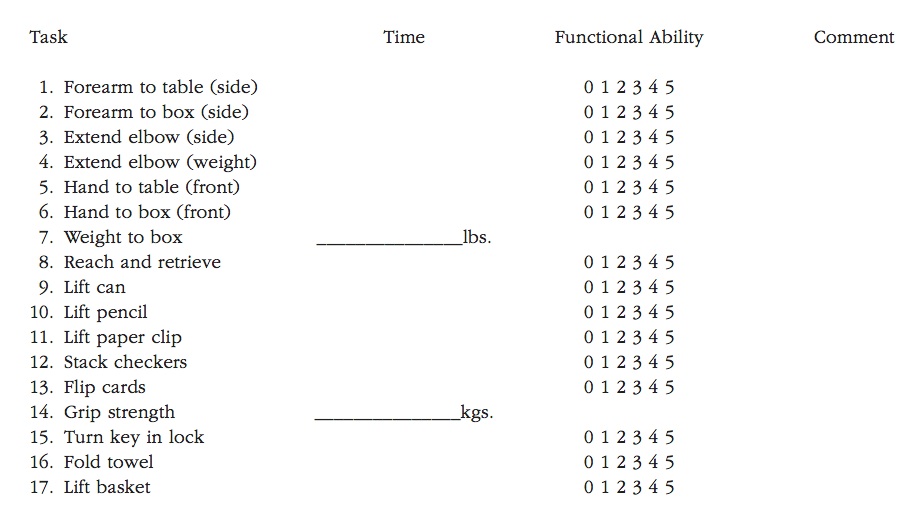
Wolf Motor Function Test: Watch this video to see how the test is performed
Advantages:
• Focused upon upper limb function (WOLF ET AL 2005b)
• High interrater reliability, internal consistency, and test-retest reliability (Morris et al 2001)
Limitations:
• Time consuming can take up to 30 minutes to complete and therefore may not be suitable for clinical practice (WOLF ET AL 2005c).
These are only two outcome measures many others suitable for upper limb stroke rehab can be found at:
http://www.ebrsr.com/sites/default/files/Chapter21_Outcome-Measures_FINAL_16ed.pdf
Activity:
Using this document http://www.ebrsr.com/sites/default/files/Chapter21_Outcome-Measures_FINAL_16ed.pdf choose an outcome measure you believe is appropriate for measuring the progress of someone with shoulder subluxation or someone with a motor control deficit following stroke and research the outcome measure further answering the questions below:
1. What are the strengths of your selected outcome measure?
2. What are the limitations of your selected outcome measure?
3. Why is it appropriate for stroke rehab?
4. What other outcome measures could have been considered?
How do I use Functional Electrical Stimulation[edit | edit source]
[edit | edit source]
Shoulder Subluxation[edit | edit source]
In this section the reader will have the opportunity to develop their knowledge and understanding relating to ES and it’s uses for shoulder subluxation post stroke.
This section will cover:
• Shoulder subluxation in stroke
• How does FES aid in Shoulder Subluxation?
• Application
• Dosage and Parameters
• How would I identify patients at risk?
• Outcome measures
• Summary
• Key note
• Evidence based
• Case study
• Further Resources
Shoulder subluxation in stroke
• Shoulder subluxation is a common problem amongst patients with extreme muscle weakness and limb inactivity. This occurs mainly due to the effect of gravity, stretching inactive soft tissues (Carr and Shepard 2003).
• Weakness of the shoulder musculature can result after a stroke, often leading to subluxation due to the muscles being unable to hold the humerus within the socket of the glenohumeral joint, further assisting gravity in pulling the humerus into an abnormal position.
• A reliable measure to test for a subluxed shoulder, is by using callipers to measure the subacromial space between the acromion and humeral head (Boyd & Torrance 1992).
For further information of shoulder subluxation in stroke please read Carr and Shepard 2003 pages 195 – 197 & 204
Definition:
Shoulder subluxation is described as inferior glenohumeral joint displacement and is a very common secondary musculoskeletal impairment in the upper limb post stroke (Ada and Foongchomcheay 2002).
Incidence of shoulder subluxation:
Shoulder subluxation occurs in 17 – 81% of patients following a stroke and has been reported as the main cause of shoulder complications (Manigandan et al. 2014). Shoulder subluxation has a high occurance rate in hemiplegic patients.
Take 10 mins to read the pathophysiology of Shoulder Subluxation in Stroke:
➢ Section 11.3
➢ Pages: 6 – 11
➢ http://www.ebrsr.com/sites/default/files/Chapter11_HemiplegicShoulder_FINAL__16ed.pdf
How does FES aid in Shoulder Subluxation?
• There is strong evidence supporting the use of FES in clinical practice in order to treat shoulder subluxation. whereby it directly stimulates the nerves and not the muscle fibres.
• Electrical stimulation should be started as early as possible i.e. initiated acutely post stroke as part of best practice for those patients who are at risk of developing subluxation due to paralysis of shoulder muscles after stroke (Ada and Foongchomcheay 2002). It also has benefits for patients in the chronic stages of stroke such as reducing the distance between the acromion and the humeral head (EBRSR 2013).
• FES also seems to helps improve function, muscle tone, joint alignment and sensory deficits (Price & Pandyan 2001).
• Functional electrical stimulation is applied to structures that aid in maintaining the position of the head of humerus in the glenoid fossa such as the supraspinatus and deltoid muscles (Vafadar et al. 2014). The long head of biceps should also be taken into consideration for patients post stroke to help minimise the risk of shoulder subluxation (Manigandan et al. 2014).
• Stimulation of the supraspinatus alone would be inadequate to maintain the humerus position in the shoulder (Kobayashi et. al. 1999)
• FES may aid in minimizing shoulder subluxation and could further be used as a preventive measure, however it does not seem to reduce pain (EBRSR 2013).
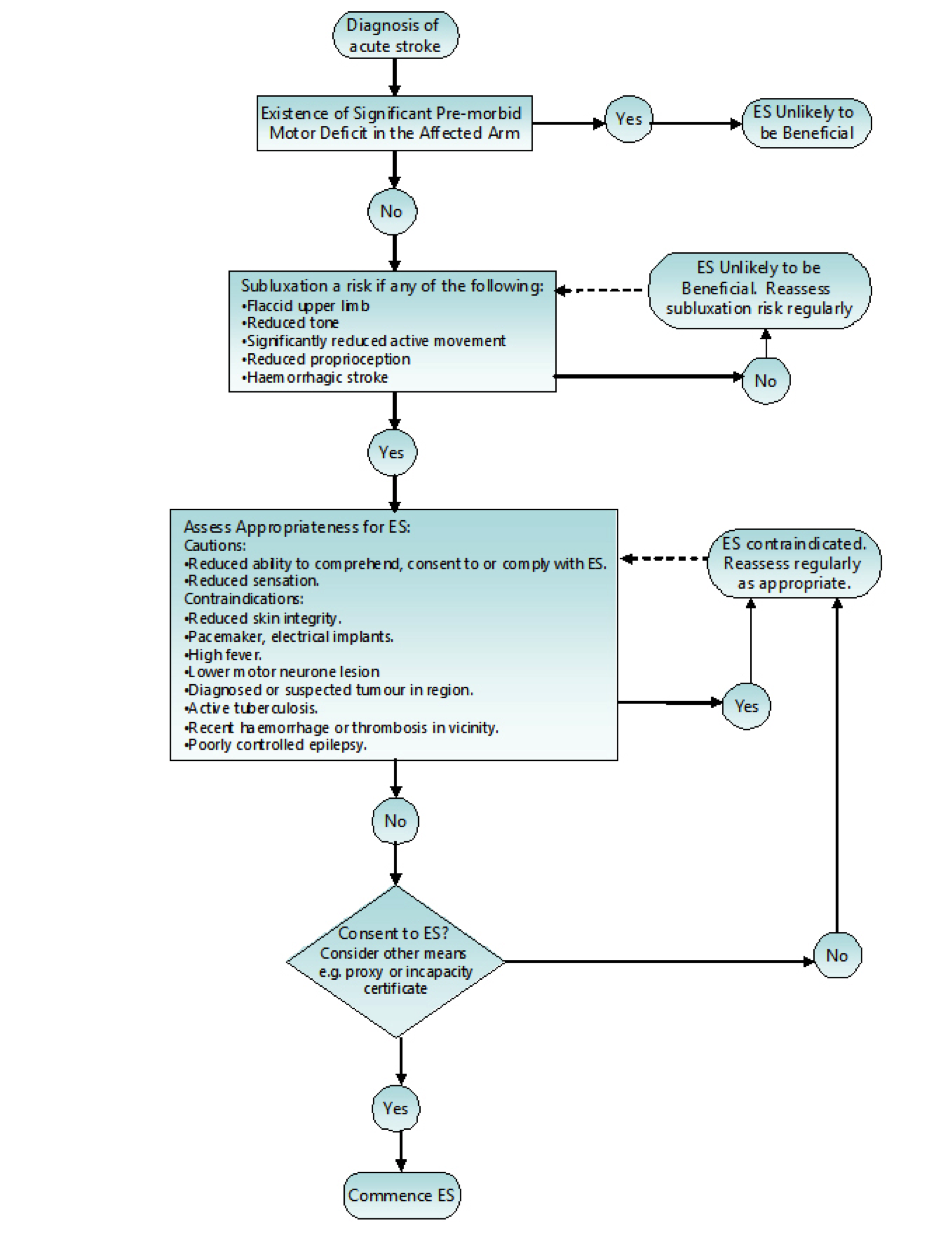
How do I identify a patient at risk of a shoulder subluxation?
An audit by (Macdonald 2013) reported:
• That patient with a subluxation was precisely identified as at risk by using the predetermined criteria (Appendix B2).
• Great majority of patients presented with a subluxation within the first week of admission.
• Patients who did not develop subluxation exhibited an increase of decreased sensation and proprioception compared to those with shoulder subluxation.
• 100% of patients who developed subluxation had low tone. Further stating that patients with either flaccidity or low tone around the shoulder with reduced active ranges of motion could be considered a risk.
• However she mentioned that only 50% of patients with the risk of shoulder subluxation would be suitable electrical stimulation and therapists should use their own clinical reasoning and judgment to select such eligible patients.
Application:
Before applying FES to the upper limb to assist reduction of shoulder subluxation, you should consider the movement you wish to illicit and the structures involved in this movement.
Below are some illustrations of FES being used with slight variations.
The settings below are by Odstock Medical Limited who are one of the main distributors of FES in the UK.
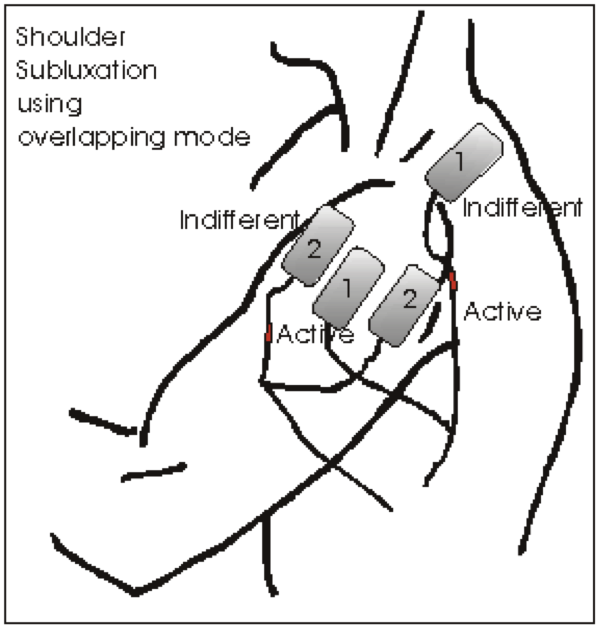
Reducing Shoulder Subluxation
2 pairs of electrodes required
Placement of pair 1: Supraspinatus & Middle of Deltoids
Placement of pair 2: Anterior & Posterior Deltoids
All 4 electrodes should fit under the hand of the clinician over the patient’s shoulder. When adjusting the current to relocate the position of the humerus, extensive shoulder abduction should be avoided.
Reduction of shoulder subluxation with external rotation
This is suitable for patients with significant anterior subluxation/ internal rotation of humerus.
2 pairs of electrodes required
Placement of pair 1: Supraspinatus & Middle of Deltoids
Placement of pair 2: Teres Minor & Posterior Deltoids
You can adjust which electrodes is active or indifferent depending on your patient’s needs. This set up should relocate the humerus more posteriorly.
Current levels maybe too high when shoulder is brought into elevation and you should adjust the current where appropriate to achieve humeral relocation.
Take 5 minutes to watch the tutorial on shoulder subluxation and skip video to 1.45 to commence shoulder subluxation video.
https://www.youtube.com/watch?v=yWMzzY_Zrv0#t=436
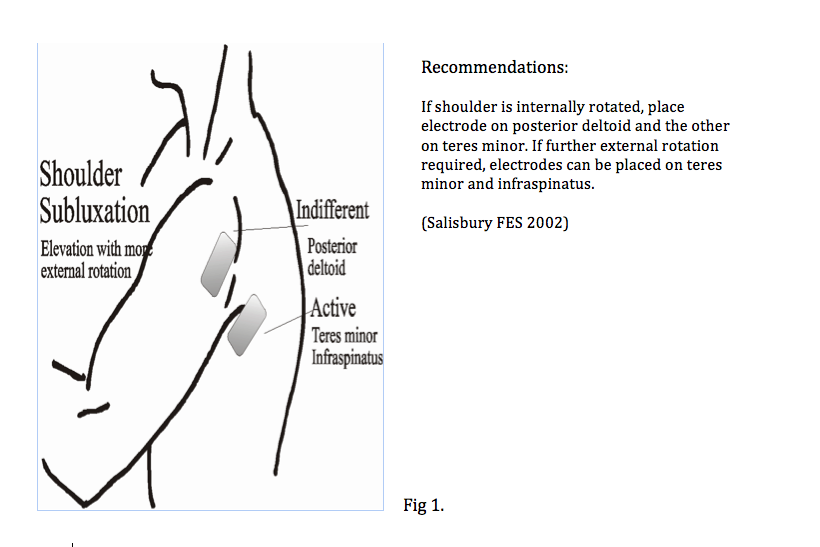
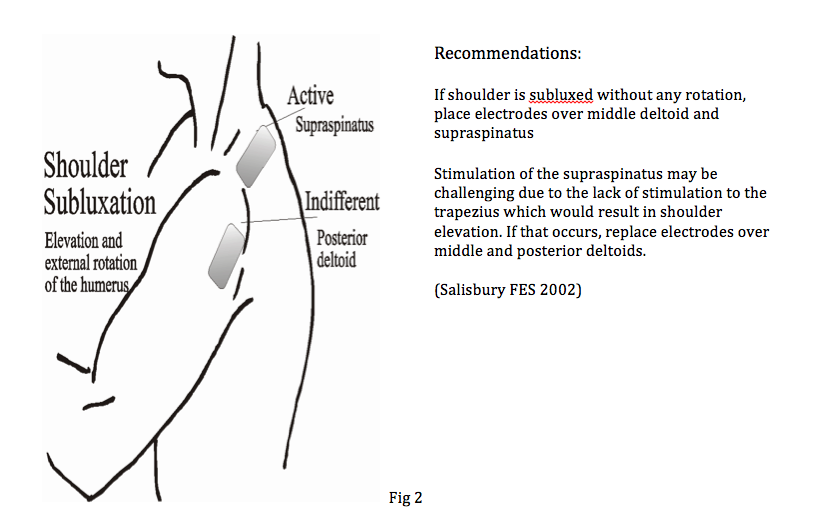
• For Figures 1 & 2 choose which electrode to make active (Strongest effect) i.e. if active electrode over teres minor causing extensive external rotation, reverse the polarity.
• Dual channels of stimulation can be applied or alternation of electrode positions.
Take note:
1. Different electrode sizes available, use whereby appropriate.
2. Electrodes should strictly be a one patient use.
Dosage and Parameters:
• Scottish Stroke AHP forum has reported that subluxation appears to arise during the flaccid period, which is the first 3 weeks post stroke. Shoulder subluxation is less likely to occur if the supraspinatus has developed some movement.
• Further evidence has also shown that early application of FES preferably within the first 48 hours post stroke is vital in preventing shoulder subluxation (Linn et. al. 1999, Fil et. al. 2011).
• FES treatments also show no further improvements after 12 months and the results remained the same 12 months later (Chantraine et. al. (1999)).
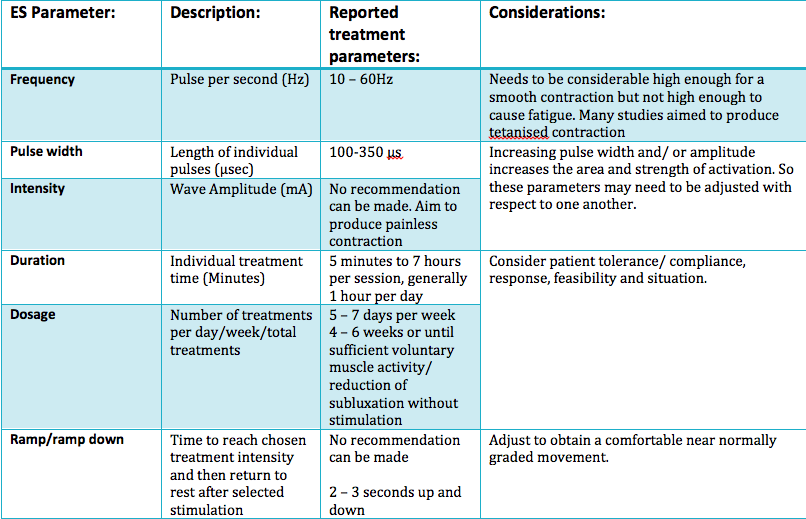
• Before commencing an FES treatment on a patient, it is important to consider the types of parameter settings available and decide upon the most appropriate setting for your patient. The different types of settings used can provoke various responses from patients.
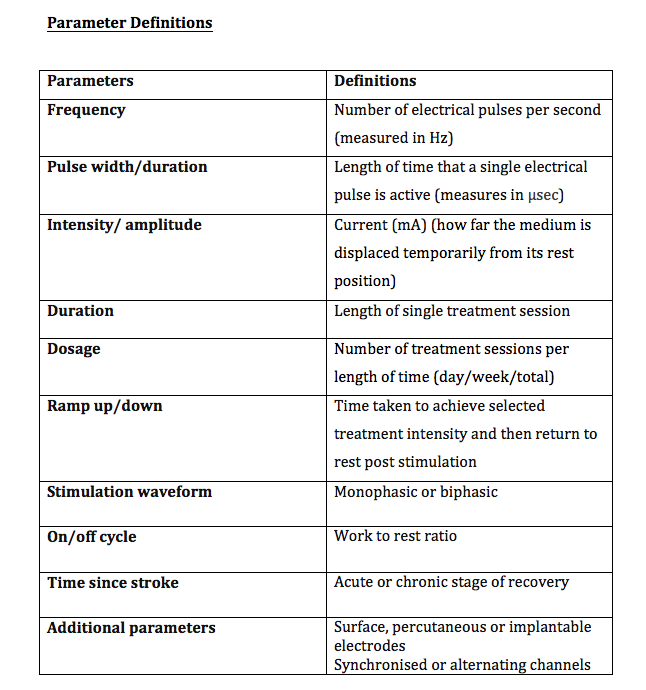
Types of parameters to consider:
1. Frequency
2. Pulse width
3. Amplitude (intensity)
4. Duration of treatment
5. Dosage i.e. number of treatments a week
6. Ramp/ Ramp down
7. Type of wave form
8. On/off cycle
9. Structures stimulated
10. Time post stroke
This was taken from the Scottish Stroke AHP forum.
For more in depth information on the different types of settings, please read pages 75 – 77 from the Scottish Stroke AHP forum
The link to this document can be found below:
http://www.chss.org.uk/documents/2014/10/electrical-stimulation-consensus-statement-ssahpf-pdf.pdf
Summary of main parameters outlined below:
Frequency:
In order to determine the amount of muscle activity generated, the frequency choice of most authors were between 10 and 60 Hz. Whereas some used a range of frequencies to produce a tetanic contraction catered to the individual (Baker, Parker 1986). However it was reported that only frequencies above 30Hz were sufficient to eilicit muscle activity due to the need to generate enough force to counteract the inferior subluxation (Ada and Foongchomcheay 2002).
Pulse amplitude and pulse width:
Many authors did not state the pulse width or justify the choice, however, the general consciences reports of values varying from 100µs and 350µs. Factors such as muscle fatigue and patient comfort should be taken into account Kroon et. al. (2005). Though it may be the tweaking of the 3 variables that generates the most important factor, which is a visible muscle contraction. However, further investigation is required to uncover the full effects of the parameter settings of electrical stimulation on shoulder subluxation.
Length of treatment:
The evidence for length of treatment showed substantial inconsistency towards the overall. The evidence was synthesized Ada and Foongchomcheay (2002) and recommended that electrical stimulation be initially applied 1 hour per day initially and gradually increased to 6 hours per day. The evidence is unclear in the case whereby subluxation has already transpired.
Patients should continue with the treatment until they have a score of more than four on the motor assessment scale (MAS) Ada and Foongchomcheay (2002). However this was in adjust with improved levels of motor control. Correspondingly, patients who scored two or more on the motor assessment scale (MAS) did not develop shoulder subluxation Linn et. al. (1999). Therefore this could be used as an outcome measure when treating patients. Furthermore, the evidence suggested that improvements of subluxation did not change from 12 – 24 months but improved within the first 12 months of treatment.
Waveform, ramp times and on/off cycle time:
The evidence showed inconclusive waveform, ramp times and on/off cycle time and that there was no definitive guidelines on the specific type of parameters towards treating shoulder subluxation. However, the general conscencious is that electrical stimulation should be considered during the acute stages, ideally the first few days post stroke in the flaccid period where there is a high risk of subluxation due to significant muscle weakness on top of conventional therapy.
Below is a FES pathway in the usage FES to prevent shoulder subluxation post acute stroke
(Scottish stroke AHP forum 2014)
Outcome Measures:
• Motor Assessment Scale (MAS) is one of the outcome measures used to gauge a patient’s functional ability and thus feed backing to clinicians if FES is necessary. However, there is limited evidence to suggest that it is the outcome measure to be used.
To familiar yourself with the motor assessment scale, click here.
http://www.rehabmeasures.org/Lists/Admin%20fields/Attachments/924/Motor_Assessment_Scale.pdf
In Summary:
The use of FES as a treatment for preventing shoulder subluxation and those having shoulder subluxation post stroke is advocated (Intercollegiate Stroke Working Party 2012, Scottish Intercollegiate Guidelines Network (SIGN) June 2010). Furthermore, early application of FES in adjunct of traditional therapeutic treatments have proven to be more superior to conventional therapy alone. Subluxation tends to occur within the flaccid period in the first 3 weeks post stroke.
The main muscles targeted for stimulation are supraspinatus and deltoids however the evidence varies with regards to which deltoid fibers prove most beneficial. It may depend on the type of subluxation your patient may have i.e. anterior or inferior subluxation. FES should be commenced for one hour per day initially and subsequently increased to 6 hours per day (Ada and Foongchomcheay (2002).
The recommended dosage of FES is that patients should continue with the treatment until they have a score of more than four on the motor assessment scale (MAS) (Ada and Foongchomcheay (2002). However this was in adjust with improved levels of motor control. Correspondingly, patients who scored two or more on the motor assessment scale (MAS) did not develop shoulder subluxation Linn et. al. (1999). Therefore this could be used as an outcome measure when treating patients.
Key Note:
• Clinical application and parameters for shoulder subluxation and motor control vary and are different.
• Early application of FES may result in a substantial decrease in subluxation as compared to late/chronic stages of subluxation.
Evidence based/Conclusion:
There is increasing more evidence supporting the use of FES in shoulder subluxation post stroke. Currently, there is good quality evidence to show that FES should be considered during the acute stages of stroke being it either used for the prevention or treatment of subluxation. However, further research is required towards the feasibilities of the device’s parameters due to the variations of study designs and treatment constraints used.
Case Study:
To review your learning, we have developed a case study of Mr Moses to help synthesis the information previously mentioned.
Mr Moses is a 70 year old retired male living with his wife. He suffered a left sided stroke three weeks ago and has been diagnosed with right sided hemiplegia. It was noted through an initial physiotherapy assessment that due to the hemiplegia there was a significant reduction of active shoulder movement and upon further examination of the shoulder the patient was showing signs of subluxation, however a definite diagnosis of the shoulder being subluxed was never completed.
In addition, due to the stroke, Mr Mose’s cognition has been affected and therefore his wife now has power of attorney. Medical staff also noted that the patient’s overall skin condition is relatively poor in adjunct with oedema of his right hand. A colleague has approached you to help with the diagnosis and for some advice due to the lack of improvements from conventional physiotherapy treatments.
You are the clinical specialist in treating patients with FES. Would FES be beneficial towards this patient?
Activity:
Looking back at the case study above;
• Can you name a reliable measure to aid in measuring a subluxed shoulder?
Answer: Callipers by measuring the subacromial space between the acromion and humeral head.
• Identify some contraindications or cautions if any?
Answer: Poor skin condition, Oedema of right hand.
• Could you recommend a potential treatment parameter for Mr Moses?
Answer: See recommended parameters of FES pages 17 – 18 from the Scottish Stroke AHP forum.
• Which muscles would you place the electrodes on and why?
Answer: Supraspinatus, Middle or Posterior deltoid due to these muscles being the main structures in maintaining humeral position in the glenoid fossa.
8 months on, Mr Moses has made a significant recovery and is being reviewed for discharge. However, his wife is concerned about him returning home, as she is keen for him to continue progress with the use of FES as she has seen the benefits this has. She has approached you to enquire about purchasing an FES device independently to continue in Mr Mose’s rehabilitation and self management.
• Now have a think about some of the requirements you would expect from an FES device, which would enable a patient to use at home.
Answer: Easy to use, Inexpensive, Easy to charge, Suitable for unsupervised use, Light weight and compact, Easily cleaned, Not for single person use.
• Having read about the possible interventions and evidence, reflect upon a situation whereby, a patient has informed you that he would like to purchase an FES device for home use even though he has been using FES for more than a year. What advice would you give this patient and why?
Answer: I would advice this patient to reconsider buying an FES device as the evidence states that there is minimal to no change in improvements past the 12 month period. Therefore there would not be much benefit in buying the device due to the limited recovery of shoulder subluxation post stroke.
Motor Control and Recovery[edit | edit source]
In this section the reader will have the opportunity to develop their knowledge and understanding relating to ES and it’s uses for motor control recovery of the upper limb post stroke.
The section is split into sections:
- How does ES aid motor control?
- The application
- Dosage and Parameters
- Evidence
- Case Study
Introduction:[edit | edit source]
It is often common for individuals to be left with a motor control deficit on their hemi-paretic side following a stroke. Many sufferers are left with controlled flexor synergy. This can cause difficulties when perfoming activities of daily living. (REFERENCE)
Electrical stimulation (ES) in patients with motor function impairment of the upper extremity has been employed as one rehabilitation modality for many years. In order for ES as a treatment for motor control to be beneficial, evidence shows that patients should have some degree of movement. NICE (2015), suggest that patients should be able to hold a contraction but may not be able to move their arm against resistance. The proposed mechanisim for upper limb motor control ES is to strengthen the elbow, wrist and finger extensor muscles, reduce the spasticity of the antagonist muscles and help to promote nueroplastic changes (Sailsbury 2002, Module 10). However, there is a limited evidence indicating that repeated muscle activation using ES may lead to improvement in voluntary motor control and providing a carry over effect (Quandt and Hummel 2014).
How does ES aid Motor control?
• It is understood that when a muscle contraction is produced by an electric stimulation, a whole range of sensory inputs are produced.
• This includes the direct sensation from the stimulation and proprioceptive feedback from joints, tendons, muscles and mechanoreceptors.
• This will cause a significant increase in the activity along the intact pathways to the cortex, stimulating the production of new synpatic connections. (Taylor et al. 2002)
• The increased level of motor neurone excitation will also make it easier for weak descending inputs to activate the motor neuron and therefore help to produce a voluntary contraction (Quandt and Hummel 2014).
• When using ES to improve motor function it is often useful to combine muscles to produce a larger pattern of movement, similar to the combination of movements in ADL’s.
Appplication[edit | edit source]
Typically there are three main focuses of ES for upper limb. These are:
elbow extension, wrist, finger and thumb extension, and a reaching action.
Overall the placement of the electrodes is key to achieving a comfortable, effective movement for the patient.
It is important to ask to the patient to assist with the movement. However, this voluntary effort must not be so great that it causes a rise in spasticity and inhibits the desired movement.
The images below indicate the electrode placement and the functional movement they help to produce.
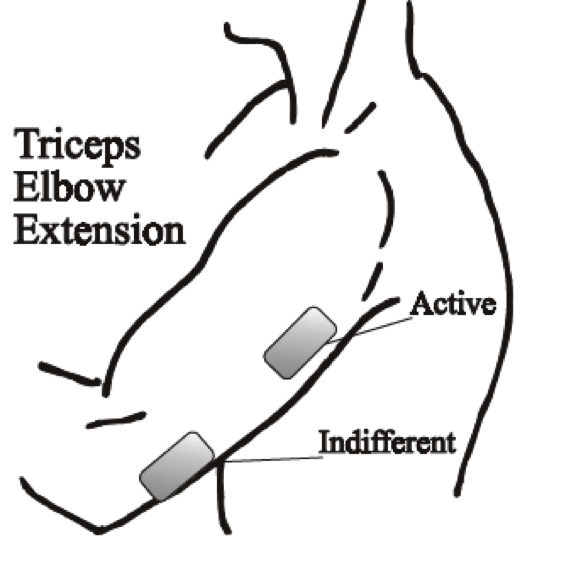
(2.1) Elbow Extension:
• The triceps can be activated placing an active electrode over its motor point and the indifferent over the tendon at the elbow.
• Due to the size of the muscle it is useful to use larger electrodes, which may help produce a more effective movement.
• Practising ‘table polishing’ by sliding the hand over a table using a cloth to reduce friction can be useful.
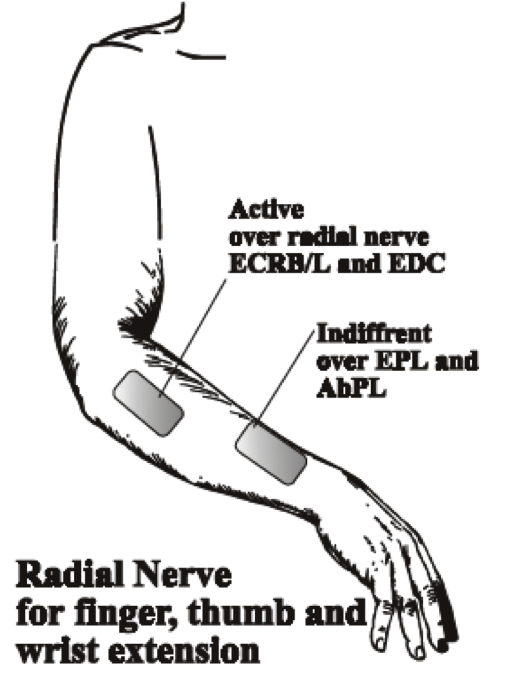
(2.2) Wrist, finger and thumb extension:
• This is best achieved by stimualtion of the radial nerve, which produces an extension pattern.
• It is often a problem to get good thumb extension so it is good practice to place the indifferent over the motor points of extensor palmaris longus and abductor palmaris longus, about three fingerbreadths proximal to the wrist.
• If thumb extension is still not good, make this electrode the active, assuming this does not significantly reduce finger and wrist extension.
• Care should be taken to avoid either radial or ulna deviation of the wrist. If there is excessive ulna deviation move the active electrode towards the extensor carpi radialis brevis on the radial side of the arm. If radial deviation occurs, move the electrode towards the ulna side and the extensor carpi ulnaris.
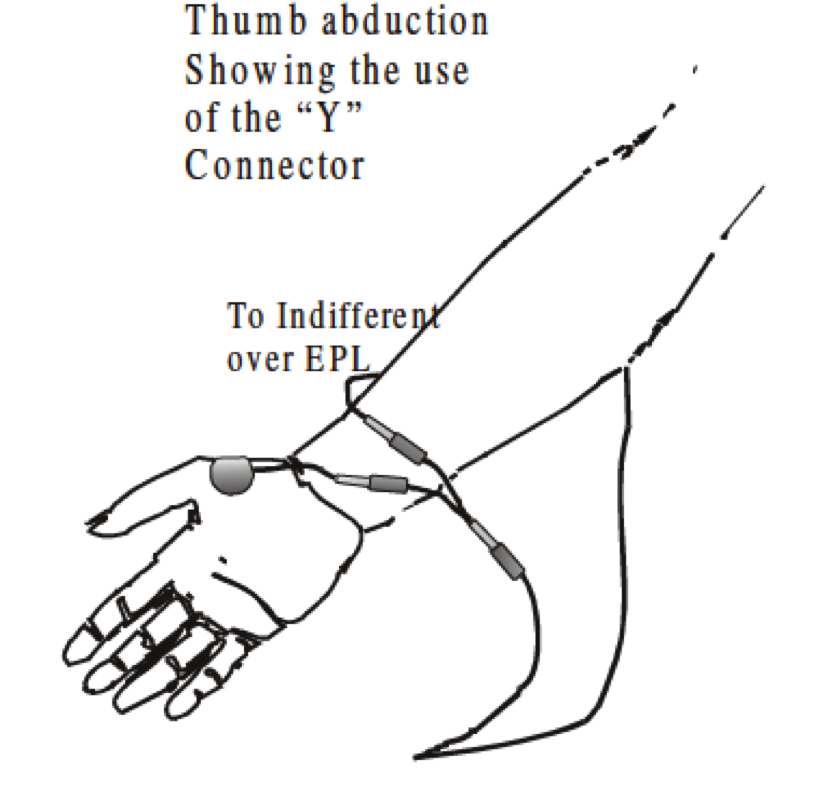
(2.3)Thumb Abduction and Opposition
• Radial nerve stimulation can be effective at opening the hand but thumb extension alone can leave the thumb in a less than functional position.
• Abduction and opposition can be produced by stimulating the thenar eminence.
• Place the active electrode over the motor point of Abductor poliicis brevis or opponens pollicis and the indifferent over the back of the wrist. To combine this movement with a general extension pattern it can be useful to use a ‘Y’ connector.
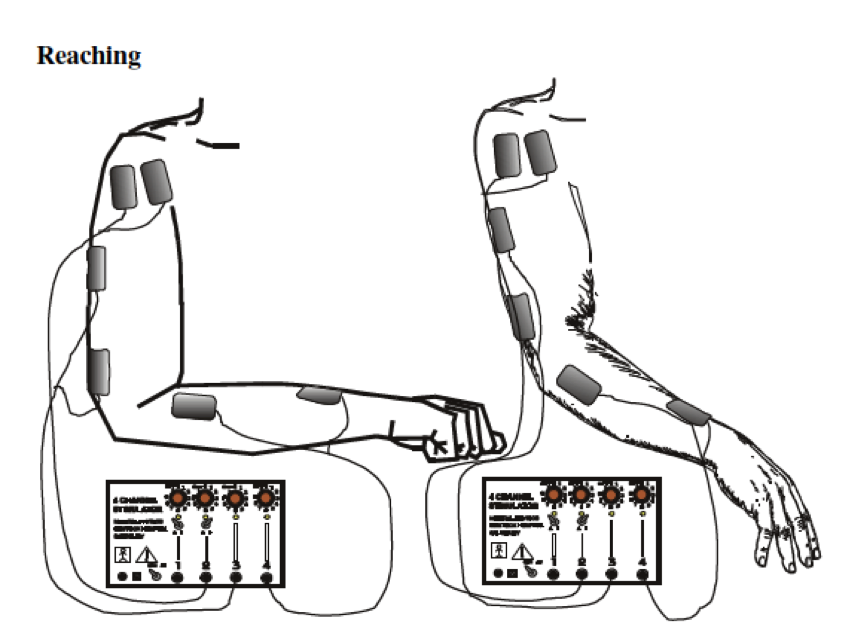
(2.4) Reaching
• It is often useful to combine muscles to produce a gross pattern of movement, similar to the combination movements used in every day life. In this way it may be possible to more effectively re-train function rather than by practising individual muscle activity.
• Reaching is where finger, thumb and wrist extension from radial nerve stimulation are combined with elbow extension and shoulder flexion by all channels on together.
The video below shows the placement of electrodes and patients carrying out a number of activities while using FES for rehabilitation of motor control for the upper limb post stroke.
Watch from 0- 1.29mins:
Dosage and Parameters[edit | edit source]
There are a wide variety of dosage and parameters in the literature. However, the SSAHPF (2014) has been developed to provide guidance for the recommended dosage and parameters for upper limb motor control recovery after stroke. Before selecting ES as a treatment it is important that you are aware of the different dosage and parameter settings and how these will affect the treatment.
In order to understand the recommended dosage and parameters for motor recovery read pages 66-71 from the Scottish Stroke Allied Health Professionals Forum 2014.
The link to this document can be found below:
http://www.chss.org.uk/documents/2014/10/electrical-stimulation-consensus-statement-ssahpf-pdf.pdf
While guidance has been given above in to the dosage and parameters, the clinician has to adjust these to fit the individual. It has been suggested in a review of ES, that it is the adjustment of these parameters which determines the nature of the evoked action potential response and thus impacts on the amount of muscle force generated as well as patient comfort and safety (de Kroon 2002; Ijzerman et al. 2005).
It is important to take into consideration whether the patient has any upper limb tone or spasticity. The dosage and parameters may need to be adjusted for these. Sailsbury (2002) suggested that if spasticity is present then a slower stimulation with a longer ramp time may be beneficial.
A summary of the main dosage and parameters are outlined below:
Frequency
In order to achieve a muscle contraction and minimise patient discomfort and fatigue while maximising clinical benefits has been reported as 12.5Hz (Scheffler and Chae 2007). However, it has also been reported that somewhere between 20-50Hz is appropriate (de Kroon et al. 2005, Sijuth 2008), with lower frequencies required for the upper limb (Scheffler and Chae 2007).
Pulse amplitue and pulse width
To achieve greater muscle force generation through recuitment of neurons increasingly further from the electrode, pulse amplitude and pulse width may (usually 200-400 micro sec) need to be adjusted (Scheffler and Chae 2007, Shu-Shyuan 2002). It has been suggested that the intensity frequency and pulse width of electrical current should be adjusted in order to produce a visible contraction. Although there is agreement in this area, there is still variablity in application and the final decision will fall to the clinician when addressing the individual patient.
Length of treatment
Common doses and duration of treatments delivered range from 30minutes once per day to one hour three times per day for two weeks to three months (de Kroon et. Al. 2005) although this was not substantiated or justified by the original authors. Hsu (2012) randomised 95 participants to dosages of 0, 15, 30, 60 minutes of ES five times per week for four weeks and reported improved recovery in the upper limb with more intensive ES. However, de Kroon et al. (2005) suggested that the particular treatment parameters may not in fact be the critical element in the efficacy of ES within their study so it may be that individual patient treatment approaches may be sufficient.
Most evidence does not justify the choice of ramp times, stimulation wave forms or on/off cycle times so recoomendations regarding these are difficult to make. However, Hsu (2012) reported cycles of 10 seconds on 10 seconds off in the first two weeks and 10 seconds on and 5 seconds off in the second two weeks.
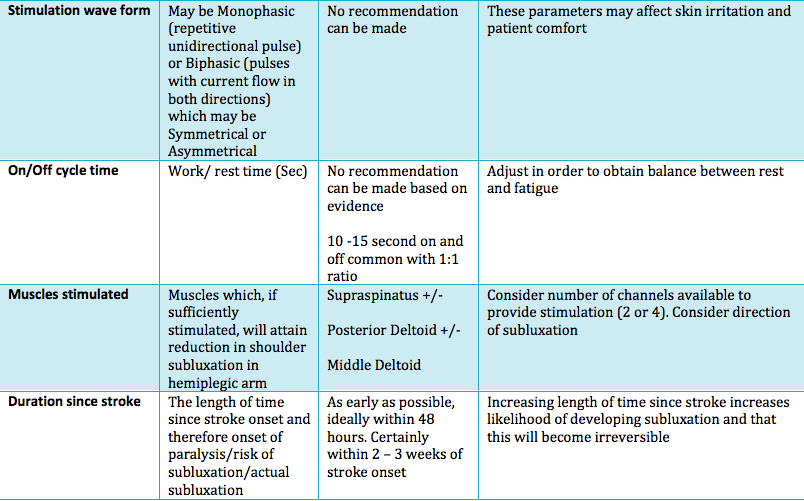
Descriptions of the common parameters reported in literature with recommeneded ranges are synthesised in the table below:
File:ES parameter and dosage Table .pdf
(CHSS Electrical Stimulation Consensus, 2014)
Evidence base[edit | edit source]
Currently there is a limited amount of evidence to support the use of FES for upper limb motor control. A number of articles have been appraised and below are their detailed findings.
A systematic review by Vafander et al. (2014), found that the use of FES does not have any significant benefits over conventional treatment. A number of the articles focused on early intervention after stroke, and concentrated on methods to measure impairments (spasticity, strength and joint motion), not function or activity. These articles showed positive benefits of FES for motor control. However, it is unclear if improvements in muscle activity and joint motion can be translated to improvement in motor function. The studies that found no superiority of FES over a conventional treatment tended to be of a higher quality and mostly used methods for measuring function or activity instead of impairment. A very limited number of articles concentrated on the use of FES in the later stages of recovery after stroke. Two out of the three studies found positive benefits, however once again these focused on impairments. This systematic review highlighted the need for further research into the effects of FES on upper motor function after both the early and late stages of recovery post stroke.
Although there is a lack of evidence showcasing the benefits for FES as a treatment on it’s own for upper limb motor function, one study has indicated when used in conjunction with other therapeutic techniques there is an improvement in an individuals motor control. Hara (2008), found that individuals that receive motor, proprioceptive, and cognitive inputs through the daily use of FES may demonstrate significantly greater improvements in voluntary movement and functional use of the hand and arm.
Another article by McCabe et al. (2015), suggested that for severely impaired stroke survivors with upper limb dysfunction the use of FES combined with motor learning (5 hours per day partial and whole-task practice of complex tasks) helped to improve coordination and functional task performance. However, when analysing the effectiveness of motor learning and FES, compared to motor learning alone or inconjuction with robotics there were no significant differences.
At this stage it is hard to say whether FES is an effective treatment due to the limited literature. Future research is needed with a greater consistency throughout the studies. More studies need to be undertaken with a larger sample size, they also need to explore the use of FES in early and late stage rehabilitation after stroke. Furthermore, the use of standarised outcome measures for function and activity will strengthen the generalisabilty for the use of FES for upper limb recovery post stroke.
The articles used in this section are referenced below if you wish to read these in full:
• HARA, Y., 2008. Neurorehabilitation with New Functional Electrical Stimulation for Hemiparetic Upper Extremity in Stroke Patients. Journal Nippon Medical School. [online]. Vol 75, no 1. [viewed 20 October 2015]. Available from: https://www.jstage.jst.go.jp/article/jnms/75/1/75_1_4/_pdf
• MCCABE, J., MONKIEWICZ, M., HOLCOMB, J., PUNDIK, S., AND DALY, J., 2015. Comparison of Robotics, Functional Elextrical Stimulation, and Motor Learning Methods for Treatment of Persistent Upper Extremity Dysfunction After Stroke: A Randomized Controlled Trial. Archieves of Physical Medicine and Rehabilitation. [online]. Vol 96, pp981-990. [viewed 19 October 2015.] Available from: http://www.archives-pmr.org/article/S0003-9993(14)01228-3/pdf
• VAFADAR, A., COTE, J., AND ARCHAMBAULT, P., 2014. Effectiveness of Functional Electrical Stimulation in Improving Clinical Outcomes in the Upper Arm Following Stroke: A Systematic Review and Meta-Analysis. Biomedical Research International. [online]. [viewed 19 October 2015]. Available from: http://www.hindawi.com/journals/bmri/2015/729768/
Case Study[edit | edit source]
Mrs Jones is a 62 year old women who lives alone she has had a hemiplegic stroke two months ago. Following her Stroke she has found the activities of daily living more difficult. Decreased motor control of her left upper limb is one of Mrs Jones key problems. Mrs Jones also suffers from spasticity in her left arm. As a result she finds dressing and cooking particularly difficult. Mrs Jones was previously very active and wishes to return to higher levels of function. She has been progressing well however recently her progress has been beginning to slow.
Questions:
- Is ES a suitable treatment for the motor recovery of Mrs Jone's left upper limb?(Using relevant evidence to guide your decision making)
- What factors would you have to take into consideration when treating Mrs Jones?
- Where would you apply ES to when you wanted to achieve: 1. elbow extension? 2. reaching?
- What dosage and parameters would you set for each application?
Recent Related Research (from <a href="http://www.ncbi.nlm.nih.gov/pubmed/">Pubmed</a>)[edit | edit source]
Feed goes here!!|charset=UTF-8|short|max=10
References
References will automatically be added here, see <a href="Adding References">adding references tutorial</a>.
<span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" />