Functional Anorectal Pain: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 14: | Line 14: | ||
==== Proctalgia Fugax ==== | ==== Proctalgia Fugax ==== | ||
For this disorder pain is momentary, present for seconds to minutes and happens sporadically such as once a | For this disorder pain is momentary, present for seconds to minutes and happens sporadically such as once a month or less<ref name=":5" />. Please use the link for more information on this disorder; [[Proctalgia Fugax]]. | ||
== Epidemiology == | == Epidemiology == | ||
| Line 32: | Line 32: | ||
Patients presenting with levator ani syndrome or unspecified functional anorectal pain often describe the feeling of pain as a dull ache or a sense of pressure upmost in the rectum. This is usually aggravated by a long duration of sitting, such as long distance car journey, and lessened by standing or lying <ref name=":7" /><ref name=":0">Wald A, Bharucha AE, Enck P, Rao SSC. Functional anorectal disorders. 3rd ed. Drossman DA, Corazzairi E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, and Whitehead WE, editors. Rome III: The Functional Gastrointestinal Disorders. McLean: Degnon Associates; 2006. pp. 639–685. [Google Scholar]</ref><ref>Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, and Eao SSC. Functional disorders of the anus and rectum. 2nd ed. Drossman DA, Corazziari E, Talley NJ, Thompson WG, and Whitehead WE, editors. Rome II: The Functional Gastrointestinal Disorders. McLean: Degnon Associates; 2000. pp. 483–542. [Google Scholar]</ref>. The pain rarely occurs at night but it's severity can rise throughout the day. It may be made more severe with sexual intercourse, stress or defecation<ref name=":2" /> <ref name=":3">Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. Biofeedback for intractable rectal pain: outcome and predictors of success. Dis Colon Rectum. 1997;40:190–196. [PubMed] [Google Scholar]</ref>. Associations have been made between patients presenting with levator ani syndrome, who are also experiencing 'psychosocial distress' (p.1474)<ref name=":7" /> and impacted quality of life<ref>Heymen S, Wexner SD, Gulledge AD. [https://pubmed.ncbi.nlm.nih.gov/8500378/ MMPI assessment of patients with functional bowel disorders]. Diseases of the colon & rectum. 1993 Jun 1;36(6):593-6.</ref>, this includes anxiety disorders, depression and stress<ref name=":2">Wald A. Functional anorectal and pelvic pain. Gastroenterol Clin North Am. 2001;30:243–51, viii-ix.[PubMed] [Google Scholar]</ref><ref>. Renzi C, Pescatori M. Psychologic aspects in proctalgia. Dis Colon Rectum. 2000;43:535–539.[PubMed] [Google Scholar]</ref>. Other causative factors to functional anorectal pain can include childbirth<ref>Salvati EP. [https://europepmc.org/article/med/3298056 The levator syndrome and its variant.] Gastroenterology Clinics of North America. 1987 Mar 1;16(1):71-8.</ref> and surgery, inclusive of 'herniated lumbar disk, hysterectomy, or low anterior resection' (p.1473)<ref name=":7" />. | Patients presenting with levator ani syndrome or unspecified functional anorectal pain often describe the feeling of pain as a dull ache or a sense of pressure upmost in the rectum. This is usually aggravated by a long duration of sitting, such as long distance car journey, and lessened by standing or lying <ref name=":7" /><ref name=":0">Wald A, Bharucha AE, Enck P, Rao SSC. Functional anorectal disorders. 3rd ed. Drossman DA, Corazzairi E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, and Whitehead WE, editors. Rome III: The Functional Gastrointestinal Disorders. McLean: Degnon Associates; 2006. pp. 639–685. [Google Scholar]</ref><ref>Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, and Eao SSC. Functional disorders of the anus and rectum. 2nd ed. Drossman DA, Corazziari E, Talley NJ, Thompson WG, and Whitehead WE, editors. Rome II: The Functional Gastrointestinal Disorders. McLean: Degnon Associates; 2000. pp. 483–542. [Google Scholar]</ref>. The pain rarely occurs at night but it's severity can rise throughout the day. It may be made more severe with sexual intercourse, stress or defecation<ref name=":2" /> <ref name=":3">Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. Biofeedback for intractable rectal pain: outcome and predictors of success. Dis Colon Rectum. 1997;40:190–196. [PubMed] [Google Scholar]</ref>. Associations have been made between patients presenting with levator ani syndrome, who are also experiencing 'psychosocial distress' (p.1474)<ref name=":7" /> and impacted quality of life<ref>Heymen S, Wexner SD, Gulledge AD. [https://pubmed.ncbi.nlm.nih.gov/8500378/ MMPI assessment of patients with functional bowel disorders]. Diseases of the colon & rectum. 1993 Jun 1;36(6):593-6.</ref>, this includes anxiety disorders, depression and stress<ref name=":2">Wald A. Functional anorectal and pelvic pain. Gastroenterol Clin North Am. 2001;30:243–51, viii-ix.[PubMed] [Google Scholar]</ref><ref>. Renzi C, Pescatori M. Psychologic aspects in proctalgia. Dis Colon Rectum. 2000;43:535–539.[PubMed] [Google Scholar]</ref>. Other causative factors to functional anorectal pain can include childbirth<ref>Salvati EP. [https://europepmc.org/article/med/3298056 The levator syndrome and its variant.] Gastroenterology Clinics of North America. 1987 Mar 1;16(1):71-8.</ref> and surgery, inclusive of 'herniated lumbar disk, hysterectomy, or low anterior resection' (p.1473)<ref name=":7" />. | ||
A digital rectal examination may be performed to ascertain the presence of tenderness when traction is applied to the levator ani muscle<ref name=":8">Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SS. [https://gut.bmj.com/content/45/suppl_2/II55?utm_source=trendmd&utm_medium=cpc&utm_campaign=gut&utm_content=consumer&utm_term=0-A Functional disorders of the anus and rectum]. Gut. 1999 Sep 1;45(suppl 2):II55-9.</ref>. Often a lack of symmetry may be noted on the physical exam and pain is mainly left sided. Presently, there is no logic as to why this side is generally more affected<ref name=":8" /><ref name=":9" />. | A digital rectal examination may be performed to ascertain the presence of tenderness when traction is applied to the [[Levator Ani Muscle|levator ani muscle]]<ref name=":8">Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SS. [https://gut.bmj.com/content/45/suppl_2/II55?utm_source=trendmd&utm_medium=cpc&utm_campaign=gut&utm_content=consumer&utm_term=0-A Functional disorders of the anus and rectum]. Gut. 1999 Sep 1;45(suppl 2):II55-9.</ref>. Often a lack of symmetry may be noted on the physical exam and pain is mainly left sided. Presently, there is no logic as to why this side is generally more affected<ref name=":8" /><ref name=":9" />. | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Summary of clinical features for one of the subtypes of functional anorectal pain. | |+Summary of clinical features for one of the subtypes of functional anorectal pain. | ||
Table adapted from Bharucha | Table adapted from Bharucha & Lee 2016 (p.1473)<ref name=":7" /> | ||
!Variable | !Variable | ||
!Levator ani syndrome | !Levator ani syndrome | ||
| Line 77: | Line 77: | ||
External pelvic tender points | External pelvic tender points | ||
| | | | ||
Yes (Puborectalis) with asymmetry (left side greater than right side). | Yes (Puborectalis) with asymmetry (left side greater than right side). | ||
| Line 84: | Line 85: | ||
== Diagnostic Criteria == | == Diagnostic Criteria == | ||
Diagnosis of Levator Ani Syndrome, as per Rome IV criteria (p.533)<ref name=":6" />, must present with all symptoms listed below: | Diagnosis of Levator Ani Syndrome, as per Rome IV criteria (p.533)<ref name=":6" />, must present with all symptoms listed below: | ||
* Chronic or recurrent rectal pain or aching. | |||
* Episodes last 30 minutes or longer. | |||
* Soreness during traction on the puborectalis. | |||
* Elimination of other sources of rectal pain, see differential diagnosis below. | |||
* Criteria is to be met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis. | |||
The diagnosis of unspecified functional anorectal pain has the same criteria as that for chronic levator ani syndrome, but there is no soreness during posterior traction on the puborectalis muscle. Again criteria is met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis<ref name=":6" /><ref name=":5" />. | The diagnosis of unspecified functional anorectal pain has the same criteria as that for chronic levator ani syndrome, but there is no soreness during posterior traction on the puborectalis muscle. Again criteria is met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis<ref name=":6" /><ref name=":5" />. | ||
| Line 107: | Line 102: | ||
* Anorectal or intramuscular abscesses | * Anorectal or intramuscular abscesses | ||
* Viral/bacterial infections in the rectum area | * Viral/bacterial infections in the rectum area | ||
* | * Haemorrhoids or thrombosed haemorrhoids | ||
* Rectal foreign body | * Rectal foreign body | ||
* Disorders associated with thrombosis, or necrosis that can result in pain<ref name=":6" /><ref name=":5" /><ref>Ooijevaar RE, Felt-Bersma RJ, Han-Geurts IJ, van Reijn D, Vollebregt PF, Molenaar CB. [https://link.springer.com/article/10.1007/s10151-019-01945-8 Botox treatment in patients with chronic functional anorectal pain: experiences of a tertiary referral proctology clinic.] Techniques in Coloproctology. 2019 Mar 1;23(3):239-44.</ref> | * Disorders associated with thrombosis, or necrosis that can result in pain<ref name=":6" /><ref name=":5" /><ref>Ooijevaar RE, Felt-Bersma RJ, Han-Geurts IJ, van Reijn D, Vollebregt PF, Molenaar CB. [https://link.springer.com/article/10.1007/s10151-019-01945-8 Botox treatment in patients with chronic functional anorectal pain: experiences of a tertiary referral proctology clinic.] Techniques in Coloproctology. 2019 Mar 1;23(3):239-44.</ref> | ||
Revision as of 21:29, 24 September 2020
Introduction[edit | edit source]
A specialist convention in the area of gastroenterology devised a criteria, known as Rome criteria for diagnosing functional gastrointestinal disorders (FGIDs)[1]. The first version was released in 1990[2]. According to the most recent version of these criteria's, Rome IV, functional disorders affiliated with anorectal pain include proctalgia fugax, levtor ani syndrome and unspecified functional anorectal pain[3]. These three types of anorectal disorders are chiefly differentiated by the length of time pain is present and by the feature or lack of anorectal tenderness[4]. However, these pain disorders do coincide and show similitude with each other[4][5], for instance patients presenting with either levator ani syndrome or unspecified anorectal pain will have chronic pain or intermittent pain with a persistent duration[4].
Functional Anorectal Disorder Type Definitions[edit | edit source]
Levator Ani Syndrome[edit | edit source]
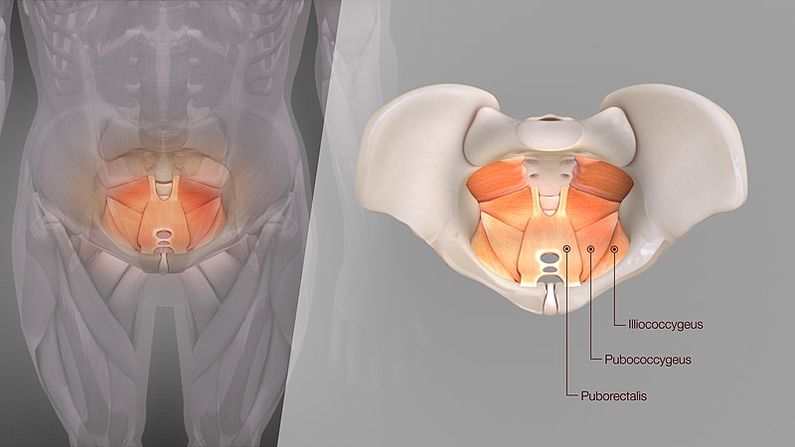
This syndrome has other names including 'levator spasm, puborectalis syndrome, and pelvic tension myalgia' (p.531)[3]. In this syndrome pain can be present for 30 minutes to being ceaseless. It's distinguishing attribute is on physical examination a hypertonic levator ani muscle and soreness on palpation of the pelvic floor or vagina[3].
Unspecified Functional Anorectal Pain[edit | edit source]
In this syndrome pain will also be present for 30 minutes to being continuous in the rectum. However, it does not present with levator ani soreness on palpation[3].
Proctalgia Fugax[edit | edit source]
For this disorder pain is momentary, present for seconds to minutes and happens sporadically such as once a month or less[4]. Please use the link for more information on this disorder; Proctalgia Fugax.
Epidemiology[edit | edit source]
A symptom specific questionnaire, Rome IV questionnaire, was used in 1990 to conduct a large population based survey to establish the extensiveness of the three types of functional anorectal pain disorders[6]. Pain resulting from the combination of these disorders was 11.6% and levator ani syndrome accounted for 6.6%[6], No physical examination was conducted and therefore, the findings did not separate levator ani syndrome and unspecified functional anorectal pain[3]. In addition, there was little difference in the incidence of anorectal pain or it's types between men and women in this survey[3]. The occurrences of anorectal pain was found to be greater in those under 45 years of age, 14% > 45 years vs 9% </= 45 years). Finally, it was estimated that 8.3% with functional anorectal pain and 11.5% with levator ani syndrome indicated they were currently too disabled to work or attend school[6]
In recent times there is currently 'no published data' (p.532)[3] on the commonness to which chronic anorectal pain is came upon in clinical practice[3].
Pathophysiological Process[edit | edit source]
There is poor insight into the pathophysiology of functional anorectal pain and happens without of any pathology[7]. Levator ani syndrome is thought to be caused by hypertonic pelvic floor muscles[3], as may be identified by an increase in 'muscle tone of the puborectalis sling' (p.190)[8] . It was found a presence of pelvic floor muscle spasm, raised anal resting pressure[9] and 'dyssynergic defecation' (p.1322)[10] to be contributors of levator ani syndrome. The latter refers to an inefficiency through defecation process in the anorectum[5] but does not include constipation[3].
The Rome IV criteria has highlighted in it's earlier editions that the three types of functional anorectal pain were classified under the title 'chronic proctalgia' (p.533)[3]. However, it is now recognised the symptom of levator ani soreness, relates to a muscular component as opposed to a rectal source for pain. This is now accepted by the definition of levator ani syndrome and the title of chronic proctalgia has been discontinued[3].
Clinical Presentation[edit | edit source]
Patients presenting with levator ani syndrome or unspecified functional anorectal pain often describe the feeling of pain as a dull ache or a sense of pressure upmost in the rectum. This is usually aggravated by a long duration of sitting, such as long distance car journey, and lessened by standing or lying [5][11][12]. The pain rarely occurs at night but it's severity can rise throughout the day. It may be made more severe with sexual intercourse, stress or defecation[13] [14]. Associations have been made between patients presenting with levator ani syndrome, who are also experiencing 'psychosocial distress' (p.1474)[5] and impacted quality of life[15], this includes anxiety disorders, depression and stress[13][16]. Other causative factors to functional anorectal pain can include childbirth[17] and surgery, inclusive of 'herniated lumbar disk, hysterectomy, or low anterior resection' (p.1473)[5].
A digital rectal examination may be performed to ascertain the presence of tenderness when traction is applied to the levator ani muscle[18]. Often a lack of symmetry may be noted on the physical exam and pain is mainly left sided. Presently, there is no logic as to why this side is generally more affected[18][19].
| Variable | Levator ani syndrome |
|---|---|
| Average age | 30-60 years |
| Sex | Men less than women |
| Pain Quality
Pain Duration Typical Pain Location Pain at other sites Precipitating factors |
Vague dull ache or pressure sensation
30 minutes or longer Rectum No Sitting long period, Stress, sexual intercourse, Defecation, Childbirth, Surgical procedure. |
| Urinary symptoms
Sexual dysfunction Psychosocial symptoms |
No
No Possible |
| Physical examination
Internal pelvic tender points External pelvic tender points |
Yes (Puborectalis) with asymmetry (left side greater than right side). No |
Diagnostic Criteria[edit | edit source]
Diagnosis of Levator Ani Syndrome, as per Rome IV criteria (p.533)[3], must present with all symptoms listed below:
- Chronic or recurrent rectal pain or aching.
- Episodes last 30 minutes or longer.
- Soreness during traction on the puborectalis.
- Elimination of other sources of rectal pain, see differential diagnosis below.
- Criteria is to be met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis.
The diagnosis of unspecified functional anorectal pain has the same criteria as that for chronic levator ani syndrome, but there is no soreness during posterior traction on the puborectalis muscle. Again criteria is met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis[3][4].
Differential Diagnosis[edit | edit source]
- Anal fissures
- Fistulas
- Inflammatory bowel disease
- Prostatitis
- Coccygodynia
- Major structural changes of the pelvic floor.
- Pudendal neuralgia
- Anorectal or intramuscular abscesses
- Viral/bacterial infections in the rectum area
- Haemorrhoids or thrombosed haemorrhoids
- Rectal foreign body
- Disorders associated with thrombosis, or necrosis that can result in pain[3][4][20]
Outcome Measures[edit | edit source]
Management/Interventions[edit | edit source]
The first line of treatment most commonly provided is reassurance that pain is benign and is not suggestive of malignanacy
Diazepam; a study revealed that hot sitz baths and or diazepam were effective for relieving pain in 68% of 316 chronic proctalgia patients[19]
Physiotherapy Management[edit | edit source]
The goal of physiotherapy in this case is to relieve pain
- Puborectalis muscle massge; this should be performed up to like 50 times depending on well the patient can tolerate it. Some claim that it may not be effective if the patient is not uncomfortable while being performed[21]
- Electro galvanic muscle stimulation has been used traditionally by Physiatrists to treat muscle spasticity especially when conservative therapy seems not to be effective.
- Biofeedback training to teach pelvic floor muscle relaxation.
Resources[edit | edit source]
References[edit | edit source]
- ↑ Simren M, Palsson OS, Whitehead WE. Update on Rome IV criteria for colorectal disorders: implications for clinical practice. Current gastroenterology reports. 2017 Apr 1;19(4):15.
- ↑ Drossman DA, Thompson WG, Talley NJ, Funch-Jensen P, Janssens J, Whitehead WE. Identification of sub-groups of functional gastrointestinal disorders. Gastroenterology International. 1990;3(4):159-72.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 Drossman DA, Hasler WL. Rome IV—functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016 May 1;150(6):1257-61.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A. Anorectal disorders. Gastroenterology. 2016 May 1;150(6):1430-42.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Bharucha AE, Lee TH. Anorectal and pelvic pain. InMayo Clinic Proceedings 2016 Oct 1 (Vol. 91, No. 10, pp. 1471-1486). Elsevier.
- ↑ 6.0 6.1 6.2 Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E, Richter JE. US householder survey of functional gastrointestinal disorders. Digestive diseases and sciences. 1993 Sep 1;38(9):1569-80.
- ↑ Iqbal F, Beggs AD, Holt T, Bowley DM. A pain in the bottom. Bmj. 2013 Jul 1;347:f4192.
- ↑ Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. Biofeedback for intractable rectal pain. Diseases of the colon & rectum. 1997 Feb 1;40(2):190-6.
- ↑ Grimaud JC, Bouvier M, Naudy B, Guien C, Salducci J. Manometric and radiologic investigations and biofeedback treatment of chronic idiopathic anal pain. Diseases of the colon & rectum. 1991 Aug 1;34(8):690-5.
- ↑ Chiarioni G, Nardo A, Vantini I, Romito A, Whitehead WE. Biofeedback is superior to electrogalvanic stimulation and massage for treatment of levator ani syndrome. Gastroenterology. 2010 Apr 1;138(4):1321-9.
- ↑ Wald A, Bharucha AE, Enck P, Rao SSC. Functional anorectal disorders. 3rd ed. Drossman DA, Corazzairi E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, and Whitehead WE, editors. Rome III: The Functional Gastrointestinal Disorders. McLean: Degnon Associates; 2006. pp. 639–685. [Google Scholar]
- ↑ Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, and Eao SSC. Functional disorders of the anus and rectum. 2nd ed. Drossman DA, Corazziari E, Talley NJ, Thompson WG, and Whitehead WE, editors. Rome II: The Functional Gastrointestinal Disorders. McLean: Degnon Associates; 2000. pp. 483–542. [Google Scholar]
- ↑ 13.0 13.1 Wald A. Functional anorectal and pelvic pain. Gastroenterol Clin North Am. 2001;30:243–51, viii-ix.[PubMed] [Google Scholar]
- ↑ Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. Biofeedback for intractable rectal pain: outcome and predictors of success. Dis Colon Rectum. 1997;40:190–196. [PubMed] [Google Scholar]
- ↑ Heymen S, Wexner SD, Gulledge AD. MMPI assessment of patients with functional bowel disorders. Diseases of the colon & rectum. 1993 Jun 1;36(6):593-6.
- ↑ . Renzi C, Pescatori M. Psychologic aspects in proctalgia. Dis Colon Rectum. 2000;43:535–539.[PubMed] [Google Scholar]
- ↑ Salvati EP. The levator syndrome and its variant. Gastroenterology Clinics of North America. 1987 Mar 1;16(1):71-8.
- ↑ 18.0 18.1 Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SS. Functional disorders of the anus and rectum. Gut. 1999 Sep 1;45(suppl 2):II55-9.
- ↑ 19.0 19.1 Grant SR, Salvati EP, Rubin RJ. Levator syndrome: an analysis of 316 cases. Diseases of the Colon & Rectum. 1975 Mar 1;18(2):161-3.
- ↑ Ooijevaar RE, Felt-Bersma RJ, Han-Geurts IJ, van Reijn D, Vollebregt PF, Molenaar CB. Botox treatment in patients with chronic functional anorectal pain: experiences of a tertiary referral proctology clinic. Techniques in Coloproctology. 2019 Mar 1;23(3):239-44.
- ↑ Salvati EP. The levator syndrome and its variant. Gastroenterol Clin North Am. 1987;16:71–78.[PubMed] [Google Scholar]






