Functional Anorectal Pain: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 3: | Line 3: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Adu Omotoyosi Johnson]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|Adu Omotoyosi Johnson]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
A specialist convention in the area of gastroenterology devised a criteria, known as Rome criteria for diagnosing functional gastrointestinal disorders (FGIDs)<ref>Simren M, Palsson OS, Whitehead WE. [https://link.springer.com/article/10.1007/s11894-017-0554-0 Update on Rome IV criteria for colorectal disorders: implications for clinical practice]. Current gastroenterology reports. 2017 Apr 1;19(4):15.</ref>. The first version was released in 1990<ref>Drossman DA, Thompson WG, Talley NJ, Funch-Jensen P, Janssens J, Whitehead WE. [https://limo.libis.be/primo-explore/fulldisplay?docid=LIRIAS1325863&context=L&vid=Lirias&search_scope=Lirias&tab=default_tab&lang=en_US&fromSitemap=1 Identification of sub-groups of functional gastrointestinal disorders.] Gastroenterology International. 1990;3(4):159-72.</ref>. According to the most recent version of these criteria's, Rome IV, functional disorders affiliated with anorectal pain include proctalgia fugax, levtor ani syndrome and unspecified functional anorectal pain<ref name=":6">Drossman DA, Chang L, Chey WD, Kellow J, Tack J, Whitehead WE and the Rome IV Committees, editors. Rome IV—functional GI disorders: disorders of gut-brain interaction. 4th | A specialist convention in the area of gastroenterology devised a criteria, known as Rome criteria for diagnosing functional gastrointestinal disorders (FGIDs)<ref>Simren M, Palsson OS, Whitehead WE. [https://link.springer.com/article/10.1007/s11894-017-0554-0 Update on Rome IV criteria for colorectal disorders: implications for clinical practice]. Current gastroenterology reports. 2017 Apr 1;19(4):15.</ref>. The first version was released in 1990<ref>Drossman DA, Thompson WG, Talley NJ, Funch-Jensen P, Janssens J, Whitehead WE. [https://limo.libis.be/primo-explore/fulldisplay?docid=LIRIAS1325863&context=L&vid=Lirias&search_scope=Lirias&tab=default_tab&lang=en_US&fromSitemap=1 Identification of sub-groups of functional gastrointestinal disorders.] Gastroenterology International. 1990;3(4):159-72.</ref>. According to the most recent version of these criteria's, Rome IV, functional disorders affiliated with anorectal pain include proctalgia fugax, levtor ani syndrome and unspecified functional anorectal pain<ref name=":6">Drossman DA, Chang L, Chey WD, Kellow J, Tack J, Whitehead WE and the Rome IV Committees, editors. Rome IV—functional GI disorders: disorders of gut-brain interaction. 4th Edition. Vol 2. Rome Foundation Inc, 2016. p531-535 </ref>. These three types of anorectal disorders are chiefly differentiated by the length of time pain is present and by the feature or lack of anorectal tenderness<ref name=":5">Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5035713/pdf/nihms776224.pdf Anorectal disorders.] Gastroenterology. 2016 May 1;150(6):1430-42.</ref>. However, these pain disorders do coincide and show similitude with each other<ref name=":5" /><ref name=":7">Bharucha AE, Lee TH. [https://www.mayoclinicproceedings.org/action/showPdf?pii=S0025-6196%2816%2930503-1 Anorectal and pelvic pain.] InMayo Clinic Proceedings 2016 Oct 1 (Vol. 91, No. 10, pp. 1471-1486). Elsevier.</ref>, for instance patients presenting with either levator ani syndrome or unspecified anorectal pain will have chronic pain or intermittent pain with a persistent duration<ref name=":5" />. | ||
== Functional Anorectal Disorder Type Definitions == | == Functional Anorectal Disorder Type Definitions == | ||
| Line 30: | Line 30: | ||
The Rome IV criteria has highlighted in it's earlier editions that the three types of functional anorectal pain were classified under the title 'chronic proctalgia' (p.533)<ref name=":6" />. However, it is now recognised the symptom of levator ani soreness, relates to a muscular component as opposed to a rectal source for pain. This is now accepted by the definition of levator ani syndrome and the title of chronic proctalgia has been discontinued<ref name=":6" />. | The Rome IV criteria has highlighted in it's earlier editions that the three types of functional anorectal pain were classified under the title 'chronic proctalgia' (p.533)<ref name=":6" />. However, it is now recognised the symptom of levator ani soreness, relates to a muscular component as opposed to a rectal source for pain. This is now accepted by the definition of levator ani syndrome and the title of chronic proctalgia has been discontinued<ref name=":6" />. | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Patients presenting with levator ani syndrome or unspecified functional anorectal pain often describe the feeling of pain as a dull ache or a sense of pressure upmost in the rectum. This is usually aggravated by a long duration of sitting, such as long distance car journey, and lessened by standing or lying <ref name=":7" /><ref name=":0"> | Patients presenting with levator ani syndrome or unspecified functional anorectal pain often describe the feeling of pain as a dull ache or a sense of pressure upmost in the rectum. This is usually aggravated by a long duration of sitting, such as long distance car journey, and lessened by standing or lying <ref name=":7" /><ref name=":0">Drossman DA, Corazzairi E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, Whitehead WE, and Rome III Committees, editors. Rome III: The Functional Gastrointestinal Disorders. 3rd Edition. Degnon Associates, 2006. p639–685. </ref><ref>Drossman DA, Corazziari E, Talley NJ, Thompson WG, Whitehead WE and the Rome II Multinational working teams, editors. Rome II: The Functional Gastrointestinal Disorders. 2nd Edition. Degnon Associates Inc, 2000. p483-542</ref>. The pain rarely occurs at night but it's severity can rise throughout the day. It may be made more severe with sexual intercourse, stress or defecation<ref name=":2" /> <ref name=":3">Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. [https://link.springer.com/article/10.1007%2FBF02054987 Biofeedback for intractable rectal pain.] Diseases of the colon & rectum. 1997 Feb 1;40(2):190-6.</ref>. Associations have been made between patients presenting with levator ani syndrome, who are also experiencing 'psychosocial distress' (p.1474)<ref name=":7" /> and impacted quality of life<ref>Heymen S, Wexner SD, Gulledge AD. [https://pubmed.ncbi.nlm.nih.gov/8500378/ MMPI assessment of patients with functional bowel disorders]. Diseases of the colon & rectum. 1993 Jun 1;36(6):593-6.</ref>, this includes anxiety disorders, depression and stress<ref name=":2">Wald A. [https://www.sciencedirect.com/science/article/abs/pii/S088985530570176X Functional anorectal and pelvic pain.] Gastroenterology Clinics of North America. 2001 Mar 1;30(1):243-52.</ref><ref>Renzi C, Pescatori M. [https://link.springer.com/article/10.1007%2FBF02237201 Psychologic aspects in proctalgia.] Diseases of the colon & rectum. 2000 Apr 1;43(4):535-9.</ref>. Other causative factors to functional anorectal pain can include childbirth<ref>Salvati EP. [https://europepmc.org/article/med/3298056 The levator syndrome and its variant.] Gastroenterology Clinics of North America. 1987 Mar 1;16(1):71-8.</ref> and surgery, inclusive of 'herniated lumbar disk, hysterectomy, or low anterior resection' (p.1473)<ref name=":7" />. | ||
A digital rectal examination may be performed to ascertain the presence of tenderness when traction is applied to the [[Levator Ani Muscle|levator ani muscle]]<ref name=":8">Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SS. [https://gut.bmj.com/content/45/suppl_2/II55?utm_source=trendmd&utm_medium=cpc&utm_campaign=gut&utm_content=consumer&utm_term=0-A Functional disorders of the anus and rectum]. Gut. 1999 Sep 1;45(suppl 2):II55-9.</ref>. Often a lack of symmetry may be noted on the physical exam and pain is mainly left sided. Presently, there is no logic as to why this side is generally more affected<ref name=":8" /><ref name=":9">Grant SR, Salvati EP, Rubin RJ. Levator syndrome: an analysis of 316 cases. Diseases of the Colon & Rectum. 1975 Mar 1;18(2):161-3.</ref>. | A digital rectal examination may be performed to ascertain the presence of tenderness when traction is applied to the [[Levator Ani Muscle|levator ani muscle]]<ref name=":8">Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SS. [https://gut.bmj.com/content/45/suppl_2/II55?utm_source=trendmd&utm_medium=cpc&utm_campaign=gut&utm_content=consumer&utm_term=0-A Functional disorders of the anus and rectum]. Gut. 1999 Sep 1;45(suppl 2):II55-9.</ref>. Often a lack of symmetry may be noted on the physical exam and pain is mainly left sided. Presently, there is no logic as to why this side is generally more affected<ref name=":8" /><ref name=":9">Grant SR, Salvati EP, Rubin RJ. Levator syndrome: an analysis of 316 cases. Diseases of the Colon & Rectum. 1975 Mar 1;18(2):161-3.</ref>. | ||
Revision as of 21:56, 26 September 2020
Introduction[edit | edit source]
A specialist convention in the area of gastroenterology devised a criteria, known as Rome criteria for diagnosing functional gastrointestinal disorders (FGIDs)[1]. The first version was released in 1990[2]. According to the most recent version of these criteria's, Rome IV, functional disorders affiliated with anorectal pain include proctalgia fugax, levtor ani syndrome and unspecified functional anorectal pain[3]. These three types of anorectal disorders are chiefly differentiated by the length of time pain is present and by the feature or lack of anorectal tenderness[4]. However, these pain disorders do coincide and show similitude with each other[4][5], for instance patients presenting with either levator ani syndrome or unspecified anorectal pain will have chronic pain or intermittent pain with a persistent duration[4].
Functional Anorectal Disorder Type Definitions[edit | edit source]
Levator Ani Syndrome[edit | edit source]
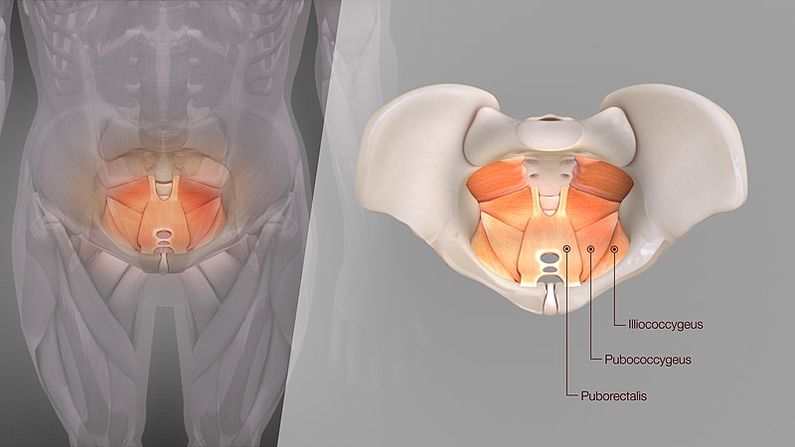
This syndrome has other names including 'levator spasm, puborectalis syndrome, and pelvic tension myalgia' (p.531)[3]. In this syndrome pain can be present for 30 minutes to being ceaseless. It's distinguishing attribute is on physical examination a hypertonic levator ani muscle and soreness on palpation of the pelvic floor or vagina[3].
Unspecified Functional Anorectal Pain[edit | edit source]
In this syndrome pain will also be present for 30 minutes to being continuous in the rectum. However, it does not present with levator ani soreness on palpation[3].
Proctalgia Fugax[edit | edit source]
For this disorder pain is momentary, present for seconds to minutes and happens sporadically such as once a month or less[4]. Please use the link for more information on this disorder; Proctalgia Fugax.
Epidemiology[edit | edit source]
A symptom specific questionnaire, Rome IV questionnaire, was used in 1990 to conduct a large population based survey to establish the extensiveness of the three types of functional anorectal pain disorders[6]. Pain resulting from the combination of these disorders was 11.6% and levator ani syndrome accounted for 6.6%[6], No physical examination was conducted and therefore, the findings did not separate levator ani syndrome and unspecified functional anorectal pain[3]. In addition, there was little difference in the incidence of anorectal pain or it's types between men and women in this survey[3]. The occurrences of anorectal pain was found to be greater in those under 45 years of age, 14% > 45 years vs 9% </= 45 years). Finally, it was estimated that 8.3% with functional anorectal pain and 11.5% with levator ani syndrome indicated they were currently too disabled to work or attend school[6]
In recent times there is currently 'no published data' (p.532)[3] on the commonness to which chronic anorectal pain is came upon in clinical practice[3].
Pathophysiological Process[edit | edit source]
There is poor insight into the pathophysiology of functional anorectal pain and can happen without of any pathology[7]. Levator ani syndrome is thought to be caused by hypertonic pelvic floor muscles[3], as may be identified by an increase in 'muscle tone of the puborectalis sling' (p.190)[8] . It was found a presence of pelvic floor muscle spasm, raised anal resting pressure[9] and 'dyssynergic defecation' (p.1322)[10] to be contributors of levator ani syndrome. The latter refers to an inefficiency through defecation process in the anorectum[5] but does not include constipation[3].
The Rome IV criteria has highlighted in it's earlier editions that the three types of functional anorectal pain were classified under the title 'chronic proctalgia' (p.533)[3]. However, it is now recognised the symptom of levator ani soreness, relates to a muscular component as opposed to a rectal source for pain. This is now accepted by the definition of levator ani syndrome and the title of chronic proctalgia has been discontinued[3].
Clinical Presentation[edit | edit source]
Patients presenting with levator ani syndrome or unspecified functional anorectal pain often describe the feeling of pain as a dull ache or a sense of pressure upmost in the rectum. This is usually aggravated by a long duration of sitting, such as long distance car journey, and lessened by standing or lying [5][11][12]. The pain rarely occurs at night but it's severity can rise throughout the day. It may be made more severe with sexual intercourse, stress or defecation[13] [14]. Associations have been made between patients presenting with levator ani syndrome, who are also experiencing 'psychosocial distress' (p.1474)[5] and impacted quality of life[15], this includes anxiety disorders, depression and stress[13][16]. Other causative factors to functional anorectal pain can include childbirth[17] and surgery, inclusive of 'herniated lumbar disk, hysterectomy, or low anterior resection' (p.1473)[5].
A digital rectal examination may be performed to ascertain the presence of tenderness when traction is applied to the levator ani muscle[18]. Often a lack of symmetry may be noted on the physical exam and pain is mainly left sided. Presently, there is no logic as to why this side is generally more affected[18][19].
| Variable | Levator ani syndrome |
|---|---|
| Average age | 30-60 years |
| Sex | Men less than women |
| Pain Quality
Pain Duration Typical Pain Location Pain at other sites Precipitating factors |
Vague dull ache or pressure sensation
30 minutes or longer Rectum No Sitting long period, Stress, sexual intercourse, Defecation, Childbirth, Surgical procedure. |
| Urinary symptoms
Sexual dysfunction Psychosocial symptoms |
No
No Possible |
| Internal pelvic tender points
External pelvic tender points |
Yes (Puborectalis) with asymmetry (left side greater than right side). No |
Further clinical investigations conducted to exclude other diseases may include sigmoidoscopy and suitable imaging studies such as defecography, ultrasound, or pelvic CT[18].
Diagnostic Criteria[edit | edit source]
Diagnosis of Levator Ani Syndrome, as per Rome IV criteria (p.533)[3], must present with all symptoms listed below:
- Chronic or recurrent rectal pain or aching.
- Episodes last 30 minutes or longer.
- Soreness during traction on the puborectalis.
- Elimination of other sources of rectal pain, see differential diagnosis below.
- Criteria is to be met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis.
The diagnosis of unspecified functional anorectal pain has the same criteria as that for chronic levator ani syndrome, but there is no soreness during posterior traction on the puborectalis muscle. Again criteria is met for the last 3 months with symptom onset at a minimum of 6 months before diagnosis[3][4].
Differential Diagnosis[edit | edit source]
- Anal fissures
- Fistulas
- Inflammatory bowel disease
- Prostatitis
- Coccygodynia
- Major structural changes of the pelvic floor.
- Pudendal neuralgia
- Anorectal or intramuscular abscesses
- Viral/bacterial infections in the rectum area
- Haemorrhoids or thrombosed haemorrhoids
- Rectal foreign body
- Disorders associated with thrombosis, or necrosis that can result in pain[3][4][20]
Outcome Measures[edit | edit source]
The Rome IV Diagnostic Questionnaires were comprised to scan for functional gastrointestinal disorders, create an inclusion criteria in clinical trials, and provide for epidemiologic surveys. Individual questionnaires have been devised for adults, children and adolescents, and infants and toddlers[21].
Management/Interventions[edit | edit source]
The first line of treatment most commonly provided is reassurance that pain is benign. Conservative lines of treatment are used first in the management of functional anorectal pain, this may include life style adaptations, diet changes, fibers, laxatives, and pelvic floor physiotherapy. However, if conservative management is unsuccessful, these functional disorders can be difficult to treat[20]. In the instance of levator ani syndrome a range of treatments aimed at relaxing the levator ani muscles may be implemented[18];
- digital massage of the levator ani muscles[22]
- sitz baths[19]
- muscle relaxants such as methocarbamol, diazepam[19], and cyclobenzeprine
- electrogalvanic stimulation (EGS)
- sacral nerve stimulation[23]
- biofeedback training
A randomized controlled study unveiled that biofeedback is markedly more effective than EGS or digital massage[10]. Patients were grouped as 'highly likely' to have levator ani syndrome if traction on the levator muscles produced soreness or as 'possible' levator ani syndrome if they did not (p.1321)[10]. All 157 patients were treated for 9 sessions that included psychologic counselling along side biofeedback, EGS, or massage. Results were monitored at 1, 3, 6, and 12 months. The results demonstrated sufficient relief as 87% for biofeedback, 45% for EGS, and 22% for massage. Pain days per month declined from 14.7 at initial to 3.3 post biofeedback, 8.9 post EGS, and 13.3 post massage. Pain levels reduced from 6.8 (0–10 scale) at beginning to 1.8 post biofeedback, 4.7 post EGS, and 6.0 post massage. Improvements were preserved for 12 months[10]. The pathophysiology of levator ani syndrome is alike to that of dyssynergic defecation[10]. In a more recent review it was reported biofeedback improves the defecation manner and attested effective for above 90% of patients in the short term[24].
Where conservative management has been unsuccessful botox may be considered as an alternative. In a study conservative management was given for 3 months then treatment with Botulinum toxin type A (BTX-A), as well as ongoing physiotherapy by a pelvic floor physiotherapist. BTX-A was found to give a prolonged remedy in 47% of patients with chronic functional anorectal pain. A further 20% had an initial response to treatment, but reverted within 3 months[20]. Patient sample size in this study was small, 113 total. It was noted in patients with solitary hypertonia of the levator ani appeared to present worse than those with only hypertonia of the anal sphincter or a mixture of both, but this difference was not statistically significant (p=0.06)[20]. In comparison, another earlier study found injection of botulinum toxin into anal sphincter did not relieve anorectal pain present in levator ani syndrome[26]. This earlier study did not include the combined management of pelvic floor physiotherapy and botox for these patients[20], thus highlighting the value of physiotherapy pelvic health intervention for this patient group.
References[edit | edit source]
- ↑ Simren M, Palsson OS, Whitehead WE. Update on Rome IV criteria for colorectal disorders: implications for clinical practice. Current gastroenterology reports. 2017 Apr 1;19(4):15.
- ↑ Drossman DA, Thompson WG, Talley NJ, Funch-Jensen P, Janssens J, Whitehead WE. Identification of sub-groups of functional gastrointestinal disorders. Gastroenterology International. 1990;3(4):159-72.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 Drossman DA, Chang L, Chey WD, Kellow J, Tack J, Whitehead WE and the Rome IV Committees, editors. Rome IV—functional GI disorders: disorders of gut-brain interaction. 4th Edition. Vol 2. Rome Foundation Inc, 2016. p531-535
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A. Anorectal disorders. Gastroenterology. 2016 May 1;150(6):1430-42.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Bharucha AE, Lee TH. Anorectal and pelvic pain. InMayo Clinic Proceedings 2016 Oct 1 (Vol. 91, No. 10, pp. 1471-1486). Elsevier.
- ↑ 6.0 6.1 6.2 Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E, Richter JE. US householder survey of functional gastrointestinal disorders. Digestive diseases and sciences. 1993 Sep 1;38(9):1569-80.
- ↑ Iqbal F, Beggs AD, Holt T, Bowley DM. A pain in the bottom. Bmj. 2013 Jul 1;347:f4192.
- ↑ Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. Biofeedback for intractable rectal pain. Diseases of the colon & rectum. 1997 Feb 1;40(2):190-6.
- ↑ Grimaud JC, Bouvier M, Naudy B, Guien C, Salducci J. Manometric and radiologic investigations and biofeedback treatment of chronic idiopathic anal pain. Diseases of the colon & rectum. 1991 Aug 1;34(8):690-5.
- ↑ 10.0 10.1 10.2 10.3 10.4 Chiarioni G, Nardo A, Vantini I, Romito A, Whitehead WE. Biofeedback is superior to electrogalvanic stimulation and massage for treatment of levator ani syndrome. Gastroenterology. 2010 Apr 1;138(4):1321-9.
- ↑ Drossman DA, Corazzairi E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, Whitehead WE, and Rome III Committees, editors. Rome III: The Functional Gastrointestinal Disorders. 3rd Edition. Degnon Associates, 2006. p639–685.
- ↑ Drossman DA, Corazziari E, Talley NJ, Thompson WG, Whitehead WE and the Rome II Multinational working teams, editors. Rome II: The Functional Gastrointestinal Disorders. 2nd Edition. Degnon Associates Inc, 2000. p483-542
- ↑ 13.0 13.1 Wald A. Functional anorectal and pelvic pain. Gastroenterology Clinics of North America. 2001 Mar 1;30(1):243-52.
- ↑ Gilliland R, Heymen JS, Altomare DF, Vickers D, Wexner SD. Biofeedback for intractable rectal pain. Diseases of the colon & rectum. 1997 Feb 1;40(2):190-6.
- ↑ Heymen S, Wexner SD, Gulledge AD. MMPI assessment of patients with functional bowel disorders. Diseases of the colon & rectum. 1993 Jun 1;36(6):593-6.
- ↑ Renzi C, Pescatori M. Psychologic aspects in proctalgia. Diseases of the colon & rectum. 2000 Apr 1;43(4):535-9.
- ↑ Salvati EP. The levator syndrome and its variant. Gastroenterology Clinics of North America. 1987 Mar 1;16(1):71-8.
- ↑ 18.0 18.1 18.2 18.3 Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SS. Functional disorders of the anus and rectum. Gut. 1999 Sep 1;45(suppl 2):II55-9.
- ↑ 19.0 19.1 19.2 Grant SR, Salvati EP, Rubin RJ. Levator syndrome: an analysis of 316 cases. Diseases of the Colon & Rectum. 1975 Mar 1;18(2):161-3.
- ↑ 20.0 20.1 20.2 20.3 20.4 Ooijevaar RE, Felt-Bersma RJ, Han-Geurts IJ, van Reijn D, Vollebregt PF, Molenaar CB. Botox treatment in patients with chronic functional anorectal pain: experiences of a tertiary referral proctology clinic. Techniques in Coloproctology. 2019 Mar 1;23(3):239-44.
- ↑ Palsson OS, Whitehead WE, Van Tilburg MA, Chang L, Chey W, Crowell MD, Keefer L, Lembo AJ, Parkman HP, Rao SS, Sperber A. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology. 2016 May 1;150(6):1481-91.
- ↑ Salvati EP. The levator syndrome and its variant. Gastroenterology Clinics of North America. 1987 Mar 1;16(1):71-8.
- ↑ Dudding TC, Thomas GP, Hollingshead JR, George AT, Stern J, Vaizey CJ. Sacral nerve stimulation: an effective treatment for chronic functional anal pain?. Colorectal Disease. 2013 Sep;15(9):1140-4.
- ↑ Carrington EV, Popa SL, Chiarioni G. Proctalgia Syndromes: Update in Diagnosis and Management. Current Gastroenterology Reports. 2020 Jun 9;22(7):35-
- ↑ Mayo Clinic. Pelvic Floor Training. Available from: https://www.youtube.com/watch?v=37a_CXKEj5M [last accessed 25/09/2020]
- ↑ Rao SS, Paulson J, Mata M, Zimmerman B. Clinical trial: effects of botulinum toxin on levator ani syndrome–a double‐blind, placebo‐controlled study. Alimentary pharmacology & therapeutics. 2009 May;29(9):985-91.






