Hemothorax
The term hemothorax can be defined as the entry of pleural fluid and blood into the pleural cavity. It needs to be pleural fluid with a hematocrit of 25% - 50% of the patient’s blood to be diagnosed as a hemothorax.[1]
Mechanism of Injury / Pathological Process[edit | edit source]
There are two layers of pleura. One of which covers the lung surface (visceral pleura) and the other the inside of the chest wall (parietal pleura). These layers of pleura adhere to each other to keep the lung from collapsing, even with the expiration of air from the lung. If air or fluid enters the pleural cavity in between these layers of pleura, it causes the lung to collapse due to its elastic recoil. If it is only air entering the pleural cavity it causes a pneumothorax. If it is fluid or blood entering the pleural cavity it could cause a pleural effusion or hemothorax. A hemothorax could be caused by trauma, coagulopathy or iatrogenic causes (through procedures like central line insertion or pleural biopsies).[1]
Clinical Presentation[edit | edit source]
- fever
- pallor
- chest pain
- chest heaviness
- dyspnea
- tachycardia
- cold sweats
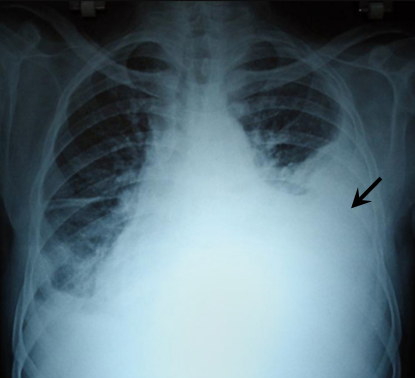
Diagnostic Procedures[edit | edit source]
- Chest X-ray
- Ultrasound
- CT scan
- MRI scan
Management / Interventions[edit | edit source]
Draining the blood as quickly as possible usually through a chest tube. Surgery could also be an option, depending on the clinical picture.
Differential Diagnosis[edit | edit source]
Through imaging, the diagnosis of a pneumothorax needs to be cancelled out. The hematocrit of the fluid from the pleural cavity could also be tested to see if it could be diagnosed as a pleural effusion or a hemothorax.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Patrini D, Panagiotopoulos N, Pararajasingham J, Gvinianidze L, Iqbal Y, Lawrence DR. Etiology and management of spontaneous haemothorax. Journal of thoracic disease. 2015 Mar;7(3):520.