Inguinal Hernia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 91: | Line 91: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
<br>It is critical to differentiate between an inguinal hernia and another condition that may mimic similar signs and symptoms<ref name="BMJ">British Medical Journal. Inguinal Hernia Differential Diagnosis. http://bestpractice.bmj.com/best-practice/monograph/723/diagnosis/differential.html (accessed | <br>It is critical to differentiate between an inguinal hernia and another condition that may mimic similar signs and symptoms<ref name="BMJ">British Medical Journal. Inguinal Hernia Differential Diagnosis. http://bestpractice.bmj.com/best-practice/monograph/723/diagnosis/differential.html (accessed 2 Feb 2013)</ref><ref name="medscape">Medscape. Hernias Differential Diagnoses. http://emedicine.medscape.com/article/775630-differential (accessed 2 Feb 2013)</ref> . | ||
<br> | <br> | ||
Revision as of 00:45, 13 February 2013
Original Editors - Lindsey Roederer and Stephanie McCauley from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
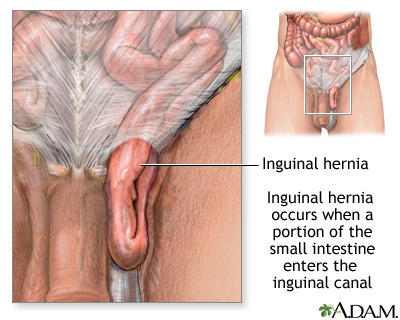
Inguinal hernias occur when soft tissue, usually intestines, protrudes from the abdominal cavity. There are two types of inguinal hernias that occur in the groin region - direct and indirect.
A direct hernia occurs when a portion of the intestine protrudes directly outward through a weak point in the abdominal wall. This weak point could be caused by a deficiency in the number of transversus abdominus aponeurotic fibers. The inguinal triangle (Hesselbach's triangle) is a common location for direct hernias to occur.
An indirect hernia occurs when a portion of the intestine pushes downward through the internal inguinal ring into the inguinal canal where the testes descend into the scrotum before birth (males) or to the labia (females) [1]
Prevalence[edit | edit source]
Rougly 5 million Americans of all ages have some type of abdominal hernia. Inguinal hernias account for 75% of all hernias. They affect 2% of men in the United States. [1] It is estimated that approximately 25% of males and 2% of females will have an inguinal hernia during their lifetime. Children can also have inguinal hernias. The incident rate for children ranges up to 4.5%.[3] Direct inguinal hernias are more common in older adults, whereas indirect inguinal hernias occur more often in infants, males, and young people. [1]
In the United States, over 1 million abdominal hernia repairs are performed each year. Of those 1 million repairs, it is estimated that 770,000 of them are inguinal hernia repairs. Males receive 90% of all inguinal hernia repairs.[3]
Characteristics/Clinical Presentation
[edit | edit source]
Associated Co-morbidities[edit | edit source]
Inguinal hernia may be associated with the following co-morbidities[4]:
• Congenital abdominal weakness
• Chronic constipation
• Chronic cough
• Enlarged prostate
• Cystic fibrosis
• Overweight, obesity, or pregnancy
• Ascites
• Smoking
• Overexertion
• Undescended testicles
• Any condition that increases pressure on the abdominal wall
Medications[edit | edit source]
Antibiotics are prescribed for strangulated hernias if ischemic bowel or infection is suspected. Over-the counter or prescribed medication for pain relief are utilized following surgical procedures[5].
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
To diagnose inguinal hernia, the doctor obtains a thorough medical history and conducts a physical examination. The patient will be asked to stand and/or cough as the doctor palpates the suspected hernia for movement. Typically, no diagnostic tests are necessary, but an ultrasound or CT scan may be utilized in some cases or for differential diagnosis.
Etiology/Causes
[edit | edit source]
Herniations can be caused by a multitude of factors. A direct inguinal hernia is caused by an acquired weakness such as obesity, pregnancy, muscle atrophy, chronic cough, ascities, heavy lifting, straining during bowel movements or urination, surgical incision, or blunt pressure from a trauma. An indirect inguinal hernia can be congenital or acquired.
There are several factors that can predispose a person to a hernia such as situational stress, degenerative changes associated with an increase in abdominal pressure, producing several offspring during one gestation, altered collagen synthesis in middle age, and simply the wear and tear of living. [1]
Systemic Involvement[edit | edit source]
Gastrointestinal-
Cardiovasular-
Integumentary-
Reproductive-
Medical Management (current best evidence)[edit | edit source]
If the hernia is small, it may be managed conservatively with activity modification and observation by the physician. However if the intestines become trapped inside the hernia, it can be life threatening situation. Immediate surgery will be necessary in this case. Additionally, inguinal hernias that continue to enlarge or cause symptoms are treated surgically. In children, inguinal hernias are surgically prepared to prevent entrapment of abdominal contents from occurring. Inguinal hernia repairs are typically treated on an outpatient basis and will be surgically managed by one of the following methods[6]:
• Herniorrhaphy (Open hernia repair)- Local or general anesthesia is administered. The surgeon makes an incision in the groin, moves the hernia back into the abdomen, and reinforces the muscle wall with stitches.
• Laparoscopy- General anesthesia is administered. The surgeon inserts a laparoscope in the lower abdomen and repairs the hernia using synthetic mesh. Typically, patients experience a shorter recovery time and fewer complications.
• Hernioplasty- The area of muscle weakness is reinforced with a synthetic mesh or screen to provide additional support. This method may be utilized in open or laparoscopic repairs.
Medication is prescribed for pain management following surgery. Vigorous activity and heavy lifting are restricted for several weeks[5].
Physical Therapy Management (current best evidence)[edit | edit source]
Education- Physical therapists educate clients on work strategies, including body mechanics, proper breathing, and lifting technique. By reducing straining and increased intraabdominal pressure, one may decrease the risk of developing a hernia or worsening an already existing hernia[1].
Screening- Obtaining a thorough medical history and conducting a physical examination is critical in determining the need for potential referral to a physician for diagnosis of an inguinal hernia. To palpate for an inguinal hernia, place hand at the location of the inguinal canal, superior to inguinal ligament and just lateral to the scrotum. Have the patient strain down or cough in standing to feel for a palpable mass.
Postoperative Rehabilitation- Often, patients are not seen for post-operative rehabilitation of an inguinal hernia repair. However, patients may require physical therapy services in order to return to prior level of function. A rehabilitation program will include posture exercises, education of body mechanics, and core stabilization strengthening. The program will be progressed as appropriate to include sport or work-specific functional activities[1].
Alternative/Holistic Management (current best evidence)[edit | edit source]
With inguinal hernias that present with minimal symptoms, it is acceptible to watch and wait instead of opting for surgical repair. Supports and trusses can be used as a short term option to contain the hernia and prevent it from increasing in size and further complications. Also, there are strapping techniques available to contain the hernia; however, they are not recommended for use because the tape could cause an ulceration of the skin covering the hernia.[1]
During the acute phase when the hernia is small in size, it can be reduced by pushing it back in place. A person could manually push it back into place using their hands. If swelling is an issue, one could place ice over the affected area prior to pushing the contents back into the abdominal cavity. Additionally, one could lie with their pelvis higher than their head to assist them in pushing it back in place.[7]
Differential Diagnosis [edit | edit source]
It is critical to differentiate between an inguinal hernia and another condition that may mimic similar signs and symptoms[8][9] .
| Condition |
Differentiating Signs and Symptoms |
| Undescended testis | • Groin mass • Underdeveloped scrotum with absent testis on affected side • Not associated with cough impulse |
| Enlarged lymph nodes | • May be associated with infection, trauma, or malignancy • Able to palpate above mass and may be moveable • Not associated with cough impulse |
| Psoas abscess | • Rare • Often accompanied with low back and buttock pain • Fever, weight loss, diaphoresis, cough • Recent contact with infection |
| Femoral aneurysm |
• Pulsing mass |
| Epididymitis | • Testicular pain • Discharge • Painful urination • Fever, chills |
| Hydrocele | • Non-tender swollen testicle • May be seen in addition to an inguinal hernia |
| Femoral hernia |
• Contents through femoral canal; difficult to differentiate from inguinal hernia |
| Athletic pubalgia | • Often no palpable mass • Testicular pain |
Case Reports/ Case Studies[edit | edit source]
DeSantana JM, et al. Hypoalgesic Effect of the Transcutaneous Electrical Nerve Stimulation Following Inguinal Herniorrhaphy: A Randomized, Controlled Trial. The Journal of Pain [Internet]. 2008 [cited 2013 Feb 9]; 9(7): 623-629. Available from: http://www.sciencedirect.com.echo.louisville.edu/science/article/pii/S1526590008003878#
Glindvad J, Jorgensen, M. Postoperative education and pain in patients with inguinal hernia. Journal of Advanced Nursing [Internet]. 2007 [cited 2013 Feb 9]; 57(6), 649–657. Available from: http://web.ebscohost.com/ehost/pdfviewer/pdfviewer?vid=6&sid=342420cc-cf02-4c37-8d2c-84c413d89c82%40sessionmgr14&hid=120
Pesanelli KE, Cigna JA, Basu SG, Morin AR. Occupational rehabilitation following open mesh surgical repair of an inguinal hernia. Phys Ther [Internet]. 2003 Jan [cited 2013 Feb 2]; 83(1): 58-66. Available from: ptjournal.apta.org/content/83/1/58.full
Unverzagt CA, Schuemann T, Mathisen J. Differential diagnosis of a sports hernia in a high-school athlete. J of Orthop Sports Phys Ther [Internet]. 2008 [cited 2013 Feb 2]; 38(2): 63-70. Available from: ejournals.ebsco.com.libproxy.bellarmine.edu/Direct.asp
Resources
[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Goodman CC, Fuller KS, Pathology: Implications for the Physical Therapist. The Gastrointestinal System. Saunders, Elsevier Inc., 2009. p870-74.
- ↑ Inguinal Hernia. PubMed Health. Available at: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001956/
- ↑ 3.0 3.1 Medscape Reference. Hernias. http://emedicine.medscape.com/article/775630-overview#a0199 (accessed 8 February 2013)
- ↑ U.S. National Library of Medicine. Hernia. http://www.nlm.nih.gov/medlineplus/ency/article/000960.htm (accessed 2013 Feb 2)
- ↑ 5.0 5.1 U.S. National Library of Medicine. Inguinal Hernia- discharge. http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000274.htm (accessed 2012 Feb 2)
- ↑ U.S. Department of Health and Human Services. Inguinal Hernia. http://digestive.niddk.nih.gov/ddiseases/pubs/inguinalhernia/index.aspx (accessed 2012 Feb 2)
- ↑ Mayo Clinic. Inguinal Hernia. http://www.mayoclinic.com/health/inguinal-hernia/DS00364/DSECTION=symptoms (accessed 10 February 2013)
- ↑ British Medical Journal. Inguinal Hernia Differential Diagnosis. http://bestpractice.bmj.com/best-practice/monograph/723/diagnosis/differential.html (accessed 2 Feb 2013)
- ↑ Medscape. Hernias Differential Diagnoses. http://emedicine.medscape.com/article/775630-differential (accessed 2 Feb 2013)