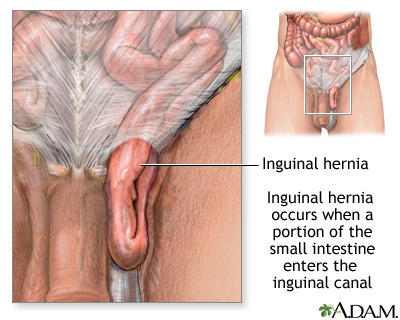
Inguinal Hernia
Original Editors - Lindsey Roederer and Stephanie McCauley from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Prevalence[edit | edit source]
The most common hernia for males and females is the inguinal hernia. Approximately 25% of males and 2% of females have an inguinal hernia during their lifetime. Furthermore, indirect inguinal hernias are more common in both sexes than direct hernias. Children can also have an inguinal hernia. The incident rate for children ranges up to 4.5%.
In the United States, over 1 million abdominal hernia repairs are performed each year. Of those 1 million repairs, it is estimated that 770,000 of them are inguinal hernia repairs. Males receive 90% of all inguinal hernia repairs.[2]
Characteristics/Clinical Presentation[edit | edit source]
add text here
Associated Co-morbidities[edit | edit source]
• Congenital abdominal weakness
• Chronic constipation
• Chronic cough
• Enlarged prostate
• Cystic fibrosis
• Overweight or obesity
• Ascites
• Smoking
• Overexertion
• Undescended testicles
• Any condition that increases pressure on the abdominal wall
Medications[edit | edit source]
Antibiotics are prescribed for strangulated hernias if ischemic bowel or infection is suspected. Over-the counter or prescribed medication for pain relief are utilized following surgical procedures.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
To diagnose inguinal hernia, the doctor obtains a thorough medical history and conducts a physical examination. The patient will be asked to stand and/or cough as the doctor palpates the suspected hernia for movement. Typically, no diagnostic tests are necessary, but an ultrasound or CT scan may be utilized in some cases or for differential diagnosis.
Etiology/Causes[edit | edit source]
add text here
Systemic Involvement[edit | edit source]
add text here
Medical Management (current best evidence)[edit | edit source]
If the hernia is small, it may be managed conservatively with activity modification and observation by the physician. However if the intestines become trapped inside the hernia, it can be life threatening situation. Immediate surgery will be necessary in this case. Additionally, inguinal hernias that continue to enlarge or cause symptoms are treated surgically. In children, inguinal hernias are surgically prepared to prevent entrapment of abdominal contents from occurring. Inguinal hernia repairs are typically treated on an outpatient basis and will be surgically managed by one of the following methods:
• Herniorrhaphy (Open hernia repair)- Local or general anesthesia is administered. The surgeon makes an incision in the groin, moves the hernia back into the abdomen, and reinforces the muscle wall with stitches.
• Laparoscopy- General anesthesia is administered. The surgeon inserts a laparoscope in the lower abdomen and repairs the hernia using synthetic mesh. Typically, patients experience a shorter recovery time and fewer complications.
• Hernioplasty- The area of muscle weakness is reinforced with a synthetic mesh or screen to provide additional support. This method may be utilized in open or laparoscopic repairs.
Medication is prescribed for pain management following surgery. Vigorous activity and heavy lifting are restricted for several weeks.
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis [edit | edit source]
It is critical to differentiate between an inguinal hernia and another condition that may mimic similar signs and symptoms.
| Condition |
Differentiating Signs and Symptoms |
| Undescended testis | • Groin mass • Underdeveloped scrotum with absent testis on affected side • Not associated with cough impulse |
| Enlarged lymph nodes | • May be associated with infection, trauma, or malignancy • Able to palpate above mass and may be moveable • Not associated with cough impulse |
| Psoas abscess | • Rare • Often accompanied with low back and buttock pain • Fever, weight loss, diaphoresis, cough • Recent contact with infection |
| Femoral aneurysm |
• Pulsing mass |
| Epididymitis | • Testicular pain • Discharge • Painful urination • Fever, chills |
| Hydrocele | • Non-tender swollen testicle • May be seen in addition to an inguinal hernia |
| Femoral hernia |
• Contents through femoral canal; difficult to differentiate from inguinal hernia |
| Athletic pubalgia | • Often no palpable mass • Testicular pain |
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NGmwZeh8JwVIzrKgHG1LrDm0izTr7ViJiDkSYAY2BW5hiXsx0|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ Inguinal Hernia. PubMed Health. Available at: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001956/
- ↑ Medscape Reference. Hernias. http://emedicine.medscape.com/article/775630-overview#a0199 (accessed 8 February 2013)