Intravenous Lines: Difference between revisions
No edit summary |
No edit summary |
||
| Line 45: | Line 45: | ||
== Complications <ref name=":1" /> == | == Complications <ref name=":1" /> == | ||
{| class="sortable" | {| class="wikitable sortable" | ||
!Phlebitis | !Phlebitis | ||
!infla | !infla | ||
Revision as of 05:01, 18 April 2019
Original Editor - Jin Yoo Top Contributors - Jin Yoo and Kim Jackson
Introduction [1][edit | edit source]
In the acute care setting, intravenous (IV) lines have varied functions:
- to infuse fluids, nutrients, electrolytes, and medication
- to obtain venous blood samples
- to insert catheters into the central circulatory system
Common areas of placement are in the forearm or back of the hand.
There are two types of venous access: peripheral and central.
Peripheral IV (PIV) [2][edit | edit source]
Overview:
- Common and preferred method for short-term therapy (< 6 days)
- A short intravenous catheter is inserted by percutaneous venipuncture into a peripheral vein
- Held in place with a sterile transparent dressing to keep site sterile and prevent accidental dislodgement
- Upper extremities are the preferred sites for insertion
- Usually attached to IV extension tubing with a positive pressure cap
Safety Considerations:
- Increased risk of systemic complications in cardiac and renal patients as well as pediatric patients, neonates, and the elderly
Central Venous Catheter (CVC) [2][edit | edit source]
Overview:
- Also known as a central line or central venous access device
- Inserted into a large vein in the central circulation system (guided by ultrasound)
- Tip of catheter terminates in the superior vena cava leading to an area just above the right atrium
- Can remain in place for more than a year
Sub-types:
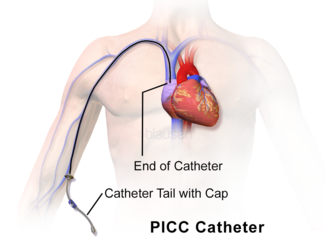
- Peripherally inserted central catheter (PICC)
- Subcutaneous or tunneled central venous catheter ("Hickman", "Broviac", "Groshong")
- Implanted central venous catheter (ICVC, or port-a-cath)
Commonly seen in patients who:
- require antineoplastic, toxic medications, multiple, vesicant/irritant medications
- are seriously/chronically ill
- require central venous pressure monitoring
- require long-term venous access/dialysis
- require total parenteral nutrition
- have poor vasculature
- have had multiple PIV insertions/attempt
Safety Considerations:
- Heightened risk for developing a nosocomial infection (need strict adherence to aseptic technique)
Complications [2][edit | edit source]
| Phlebitis | infla |
|---|---|
Administration Equipment [2][edit | edit source]
Assessment[2][edit | edit source]
- type of CVC and insertion date
- dressing is dry and intact
- lines and sutures are secure
- insertion site is free from redness, pain, or swelling
- positive pressure cap is attached securely
- IV fluids are running through IV pump
- number of lumens and type of fluid running through each lumen
- vital signs
- respiratory/cardiovascular examination to check for signs and symptoms of fluid overload