Medial Tibial Stress Syndrome: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Extracorporeal Shockwave Therapy (ESWT)" to "[[Extracorporeal Shockwave Therapy ") |
||
| (167 intermediate revisions by 21 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' - [[User:Karsten De Koster|Karsten De Koster]] | '''Original Editors ''' - [[User:Karsten De Koster|Karsten De Koster]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | ||
</div> | </div> | ||
== | == Introduction == | ||
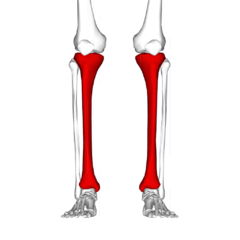
[[File:Tibia - frontal view.png|thumb|Pain generally in the inner and lower 2/3rds of tibia.|alt=|240x240px]] | |||
Medial Tibial Stress Syndrome (MTSS) is a common overuse injury of the lower extremity. It typically occurs in runners and other athletes that are exposed to intensive weight-bearing activities such as jumpers<ref name=":10">Radiopedia Medial tibial stress syndrome Available: https://radiopaedia.org/articles/medial-tibial-stress-syndrome-1<nowiki/>(accessed 2.6.2022)</ref>. It presents as exercise-induced pain over the anterior [[tibia]] and is an early stress injury in the continuum of tibial [[Stress Fractures|stress fractures]].<ref name=":9">McClure CJ, Oh R. Medial Tibial Stress Syndrome. 2019 Available:https://www.ncbi.nlm.nih.gov/books/NBK538479/ (accessed 2.6.2022)</ref>. | |||
It has the layman's moniker of “shin splints.”<ref name=":9" /> | |||
== Epidemiology == | |||
[[File:Runner surface and shoes.jpg|thumb|Risk factor- quick increase in running volume]] | |||
The incidence of MTSS ranges between 13.6% to 20% in runners and up to 35% in military recruits. In dancers it is present in 20% of the population and up to 35% of the new recruits of runners and [[Dancer's Tendonitis|dancers]] will develop it.<ref name=":3">Lohrer, H., Malliaropoulos, N., Korakakis, V., & Padhiar, N. [https://scholar.google.com/scholar_url?url=https://www.tandfonline.com/doi/abs/10.1080/00913847.2018.1537861&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=14631594707254492548&ei=_eU0Y_H8BZCXywTOrbawDQ&scisig=AAGBfm3OdinnrYmQUWLRtFcZkUHgI0G7iA Exercise-induced leg pain in athletes: diagnostic, assessment, and management strategies]. The Physician and sports medicine. 2018</ref> | |||
== | Large increase in [[Load Management|load]], volume and high impact exercise can put at risk individuals to MTSS. Risk factors include being a female, previous history of MTSS, high [[Body Mass Index|BMI]], [[Navicular Drop Test|navicular drop]], reduced hip external rotation [https://www.physio-pedia.com/Range_of_Motion range of motion], muscle imbalance and inflexibility of the [[Triceps Surae|triceps surae]]), muscle weakness of the triceps surae (prone to muscle fatigue leading to altered running mechanics, and strain on the tibia), running on a hard or uneven surface and bad running shoes <ref name=":9" /><ref name=":2">Galbraith, R. M., & Lavallee, M. E. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2848339/pdf/12178_2009_Article_9055.pdf Medial tibial stress syndrome: conservative treatment options]. Current reviews in musculoskeletal medicine. 2009; ''2''(3): 127-133.</ref> <ref name="Broos, 1991">Broos P. Sportletsels : [https://scholar.google.com/scholar_url?url=https://books.google.com/books%3Fhl%3Den%26lr%3D%26id%3D2FpjR04UCa8C%26oi%3Dfnd%26pg%3DPA15%26dq%3DBroos%2BP.%2BSportletsels%25C2%25A0%2B%2Baan%2Bhet%2Blocomotorisch%2Bapparaat.%2BLeuven%2B%2BGarant,%2B1991.%2B(Level%2Bof%2BEvidence%2B%2B5)%26ots%3DOnE9hHIuQQ%26sig%3DSNzM0EcqnaojVd0KEZzcn8C6YQM&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=15174174591971393226&ei=K-Y0Y7uaIo3MyQSdgLaoAw&scisig=AAGBfm006F6JmHsTT0RP_Ek7dEvR0173aw aan het locomotorisch apparaat. Leuven: Garant, 1991]. (Level of Evidence: 5)</ref> | ||
== Pathophysiology == | |||
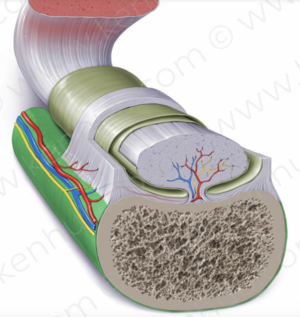
[[File:Periosteum (green).png|thumb|Periosteum, vivid green]] | |||
The pathophysiologic process resulting in MTSS is related to unrepaired microdamage accumulation in the cortical bone of the distal tibia, however this has not been definitively established. Two current theories are: | |||
# The pain is secondary to [[Inflammation Acute and Chronic|inflammation]] of the periosteum as a result of excessive traction of the [[Tibialis Posterior|tibialis posterior]] or [[soleus]], supported by bone scintigraphy findings of a broad linear band of increased uptake along the medial tibial [[periosteum]]. But a case-controlled ultrasound based study which compared periosteal and tendinous edema of athletes with and without medial tibial stress syndrome found no difference between the groups. | |||
# Bony overload injury, with resultant microdamage and targeted remodeling. A study evaluating tibia biopsy specimens from the painful area of six athletes suffering from medial tibial stress syndrome gave only equivocal support for this theory. Linear microcracks were found in only three specimens and there was no associated repair reaction<ref name=":11">Milgrom C, Zloczower E, Fleischmann C, Spitzer E, Landau R, Bader T, Finestone AS. [https://sbrate.com.br/wp-content/uploads/2021/01/Artigo-Andr%C3%A9-Pedrinelli-Ot%C3%A1vio-Assis-COMPLEMENTO-JSAMS_MEDIAL_TIBIAL_STRESS_GUIDELINES.pdf Medial tibial stress fracture diagnosis and treatment guidelines]. Journal of science and medicine in sport. 2021 Jun 1;24(6):526-30. (accessed 2.6.2022)</ref>. | |||
== Clinical Presentation and Assessment == | |||
{| class="wikitable" | |||
! colspan="2" |KEY POINTS FOR ASSESSMENT MTSS<ref name=":3" /> | |||
|- | |||
|HISTORY | |||
| | |||
* Increasing pain during exercise related to the medial tibial border in the middle and lower third | |||
* Pain persists for hours or days after cessation of activity | |||
* Pain decreases with running (early stage) | |||
* Differentiate from exertional compartment syndrome, for which pain increases with running | |||
* Earlier onset of pain with more frequent training (later stages) | |||
|- | |||
|PHYSICAL EXAMINATION | |||
| | |||
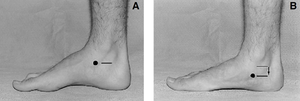
* Intensive tenderness of the involved medial tibial border, more than 5 cm | |||
* Pes planus | |||
* Tight Achilles tendon | |||
* A "one-leg hop test" is a functional test, that can be used to distinguish between medial tibial stress syndrome and a stress fracture: a patient with medial tibial stress syndrome can hop at least 10 times on the affected leg where a patient with a stress fracture cannot hop without severe pain. The sensitivity of the hop test for diagnosing medial tibial stress fracture when pain and tenderness were present was 100%, the specificity 45%, the positive predictive value 74%, and the negative predictive value 100% | |||
* Provocative test: pain on resisted plantar flexion | |||
|- | |||
|IMAGING | |||
|MRI: Periosteal reaction and edema | |||
|- | |||
|TREATMENT | |||
|See later in page | |||
|} | |||
<ref name=":0">Winters, M. [https://scholar.google.com/scholar_url?url=https://bjsm.bmj.com/content/bjsports/early/2018/03/23/bjsports-2017-098907.full.pdf&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=3120398065407133087&ei=eeY0Y9aDG-2KywSS3bH4Bg&scisig=AAGBfm2fh9BOQCGC1Yf8URbtP1putOqQ9Q Medial tibial stress syndrome: diagnosis, treatment and outcome assessment] (PhD Academy Award). Br J Sports Med. 2018</ref><ref name=":1">Thacker, S. B., Gilchrist, J., Stroup, D. F., & Kimsey, C. D. The prevention of shin splints in sports: a systematic review of literature. Medicine & Science in Sports & Exercise. 2002; ''34''(1): 32-40.</ref><ref name=":2" /><ref name=":3" /><ref name=":11" /> | |||
Watch this video on MTSS. | |||
{{#ev:youtube|KrCpFoR5PCY}} | |||
== Management == | |||
[[File:Navicular drop test.png|thumb|Navicular drop test]] | |||
Management of MTSS is conservative, focusing on rest and activity modification with less repetitive, load-bearing exercise. No specific recommendations on the duration of rest required for resolution of symptoms, and it is likely variable depending on the individual. | |||
Other therapies available (with low-quality evidence) include iontophoresis, phonophoresis, [https://www.physio-pedia.com/Cryotherapy ice] massage, [https://www.physio-pedia.com/Therapeutic_Ultrasound ultrasound therapy], periosteal pecking, and [[Extracorporeal Shockwave Therapy |extracorporeal shockwave therapy]]. A recent study on naval recruits showed prefabricated [[Introduction to Orthotics]] reduced MTSS<ref name=":9" />. | |||
= | Complications: Recurrence common after resumption of heavy activity.<ref name=":4" /> | ||
== Physical Therapy Management == | |||
Patient education and a graded loading exposure program seem the most logical treatments.<ref name=":0" /> Conservative therapy should initially aim to correct functional gait, and biomechanical overload factors.<ref name=":3" />Recently ‘running retraining’ has been advocated as a promising treatment strategy and graded running programme has been suggested as a gradual tissue-loading intervention.<ref name=":3" /> | |||
Prevention of MTSS was investigated in few studies and shock-absorbing insoles, pronation control insoles, and graduated running programs were advocated.<ref name=":3" /> | |||
Over-stress avoidance is the main preventive measure of MTSS or shin-splints. The main goals of shin-splints treatment are pain relieve and return to pain‑free activities.<ref>Alfayez, S. M., Ahmed, M. L., & Alomar, A. Z. [https://scholar.google.com/scholar_url?url=https://journalmsr.com/a-review-article-of-medial-tibial-stress-syndrome/&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=15053537490463950903&ei=puY0Y57SFIHeyQTv06PwDQ&scisig=AAGBfm13OxVYa3JO_AGvF9k0TbYwp3Dqiw A review article of medial tibial stress syndrome]. Journal of Musculoskeletal Surgery and Research. 2017; ''1''(1): 2. (Level of Evidence: 4) </ref> | |||
== | === Acute phase === | ||
2-6 weeks of rest combined with medication is recommended to improve the symptoms and for a quick and safe return after a period of rest. NSAIDs and Acetaminophen are often used for analgesia. Also cryotherapy with Ice-packs and eventually analgesic gels can be used after exercise for a period of 20 minutes. | |||
* There are a number of physical therapy modalities to use in the acute phase but there is no proof that these therapies such as ultrasound, soft tissue mobilization, electrical stimulation<ref name=":6">Beck B. [http://bands.ua.edu/wp-content/uploads/2015/07/Tibial-Stress-Injuries-Review.pdf Tibial stress injuries: an aetiological review for the purposes of guiding management.] Sports Medicine. 1998; 26(4):265-279.</ref> would be effective.<ref name=":2" /> A corticoid injection is contraindicated because this can give a worse sense of health. Because the healthy tissue is also treated. A corticoid injection is given to reduce the pain, but only in connection with rest.<ref name="Broos, 1991" /> | |||
* Prolonged rest is not ideal for an athlete. | |||
=== Subacute phase === | |||
The treatment should aim to modify training conditions and to address eventual biomechanical abnormalities. Change of training conditions could be decreased running distance, intensity and frequency and intensity by 50%. It is advised to avoid hills and uneven surfaces. | |||
== | * During the rehabilitation period the patient can do low impact and cross-training exercises (like running on a hydro-gym machine). After a few weeks athletes may slowly increase training intensity and duration and add sport-specific activities, and hill running to their rehabilitation program as long as they remain pain-free. | ||
* A stretching and strengthening (eccentric) calf exercise program can be introduced to prevent muscle fatigue. <ref name=":8">Dugan S, Weber K. [https://pubmed.ncbi.nlm.nih.gov/17678759/ Stress fracture and rehabilitation.] Phys Med Rehabil Clin N Am. 2007;18(3):401–416. (Level of evidence 3A)</ref><ref>Couture C, Karlson K. [https://scholar.google.com/scholar_url?url=https://www.tandfonline.com/doi/abs/10.3810/psm.2002.06.337&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=9979500497343675539&ei=A-c0Y76OIoHeyQTv06PwDQ&scisig=AAGBfm1oGFVoivU0Ez5hJtHPoQEQiDgZbA Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints]’. Phys Sportsmed. 2002;30(6):29–36.(Level of Evidence: 3a)</ref><ref name=":7">DeLee J, Drez D, Miller M. DeLee and Drez’s orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders. 2003:2155–2159.(Level of Evidence: 5)</ref> Patients may also benefit from [https://www.physio-pedia.com/Strength_Training strengthening] core hip muscles. Developing core stability with strong abdominal, gluteal, and hip muscles can improve running mechanics and prevent lower-extremity overuse injuries. <ref name=":7" /> | |||
* Proprioceptive [https://www.physio-pedia.com/Balance_Training balance training] is crucial in neuromuscular education. This can be done with a one-legged stand or balance board. Improved [https://www.physio-pedia.com/Proprioception proprioception] will increase the efficiency of joint and postural-stabilizing muscles and help the body react to running surface incongruities, also key in preventing re-injury.<ref name=":7" /> | |||
* Choosing good shoes with good shock absorption can help to prevent a new or re-injury. Therefore it is important to change the athlete's shoes every 250-500 miles, a distance at which most shoes lose up to 40% of their shock-absorbing capabilities.<br>In case of biomechanical problems of the foot, individuals may benefit from [[Introduction to Orthotics]]. An over-the-counter orthosis (flexible or semi-rigid) can help with excessive foot pronation and pes planus. A cast or a pneumatic brace can be necessary in severe cases.<ref name=":2" /> | |||
* [https://www.physio-pedia.com/Manual_Therapy Manual therapy] can be used to control several biomechanical abnormalities of the spine, sacro-illiacal joint and various muscle imbalances. They are often used to prevent relapsing to the old injury. | |||
* There is also acupuncture, ultrasound therapy injections and extracorporeal shock-wave therapy but their efficiency is not yet proved. | |||
== Differential Diagnosis == | |||
{| class="wikitable" | |||
== | | colspan="0" |'''Condition''' | ||
| colspan="0" |'''Characteristics''' | |||
| colspan="0" |'''Tissue origin''' | |||
|- | |||
| colspan="0" |Anterior tibial stress syndrome | |||
| colspan="0" |Vague, diffuse pain along anterolateral tibia, worse at beginning of exercise that decreases during training | |||
| rowspan="2" |Periosteum | |||
|- | |||
= | | colspan="0" |Medial tibial stress syndrome | ||
| colspan="0" |Vague, diffuse pain along middle-distal tibia, worse at beginning of exercise, that decreases during training | |||
|- | |||
| colspan="0" |Tibial/fibular stress fracture | |||
= | | colspan="0" |Pain with running, point tenderness over fracture site, "dreaded black line" on lateral x-ray | ||
| colspan="0" |Bone | |||
|- | |||
| colspan="0" |Exertional compartment syndrome | |||
== | | colspan="0" |Symptoms begin 10min into exercise andresolve 30min after exercise, sensory or motor loss, elevated anterior compartment pressures | ||
| colspan="0" |Muscle and fascia | |||
|- | |||
| colspan="0" |Leg Tendinopathy | |||
= | | colspan="0" |May be Achilles tendon, peroneal tendon, or tibialis posterior | ||
| colspan="0" |Tendon | |||
|- | |||
| colspan="0" |Sural or SPN entrapment | |||
| colspan="0" |Dermatomal distribution of symptoms | |||
| rowspan="2" |Nerve | |||
|- | |- | ||
| | | colspan="0" |Lumbar radiculopathy | ||
| | | colspan="0" |Worse with lumbar tension position (sitting) | ||
|- | |- | ||
| | | colspan="0" |Popliteal artery entrapment | ||
| | | colspan="0" |Diagnosed with vascular studies | ||
| colspan="0" |Blood vessel | |||
|} | |} | ||
<ref name=":4">Ortho bullets [https://www.orthobullets.com/knee-and-sports/3108/tibial-stress-syndrome-shin-splints Tibial Stress Syndrome] (Shin Splints) Available: https://www.orthobullets.com/knee-and-sports/3108/tibial-stress-syndrome-shin-splints<nowiki/>(accessed 2.6.2022)</ref> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
‘Shin splints’ is a vague term that implicates pain and discomfort in the lower leg, caused by repetitive loading stress. There can be all sorts of causes to this pathology according to different researches. Therefore, a good knowledge of the anatomy is always important, but it’s also important you know the other disorders of the lower leg to rule out other possibilities, which makes it easier to understand what’s going wrong. Also a detailed screening of known’s risk factors, intrinsic as well as extrinsic, to recognize factors that could add to the cause of the condition and address these problems. | |||
== References == | |||
== References | |||
<references /> | <references /> | ||
[[Category:Vrije_Universiteit_Brussel_Project| | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Sports_Injuries]] | |||
[[Category:Ankle]] [[Category:Ankle - Conditions]] | |||
[[Category:Knee]] [[Category:Knee - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Primary Contact]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 18:25, 9 January 2024
Original Editors - Karsten De Koster
Top Contributors - Karsten De Koster, Claudia Karina, Nick Van Doorsselaer, Alex Palmer, Lucinda hampton, Admin, Kenza Mostaqim, Arno Van Hemelryck, Kim Jackson, Luna Antonis, Bieke Bardyn, Sally Ngo, WikiSysop, Wanda van Niekerk, Naomi O'Reilly, 127.0.0.1, Claire Knott, Venus Pagare, Chelsea Mclene, Daniele Barilla, Kai A. Sigel and Fitz Van Roy
Introduction[edit | edit source]
Medial Tibial Stress Syndrome (MTSS) is a common overuse injury of the lower extremity. It typically occurs in runners and other athletes that are exposed to intensive weight-bearing activities such as jumpers[1]. It presents as exercise-induced pain over the anterior tibia and is an early stress injury in the continuum of tibial stress fractures.[2].
It has the layman's moniker of “shin splints.”[2]
Epidemiology[edit | edit source]
The incidence of MTSS ranges between 13.6% to 20% in runners and up to 35% in military recruits. In dancers it is present in 20% of the population and up to 35% of the new recruits of runners and dancers will develop it.[3]
Large increase in load, volume and high impact exercise can put at risk individuals to MTSS. Risk factors include being a female, previous history of MTSS, high BMI, navicular drop, reduced hip external rotation range of motion, muscle imbalance and inflexibility of the triceps surae), muscle weakness of the triceps surae (prone to muscle fatigue leading to altered running mechanics, and strain on the tibia), running on a hard or uneven surface and bad running shoes [2][4] [5]
Pathophysiology[edit | edit source]
The pathophysiologic process resulting in MTSS is related to unrepaired microdamage accumulation in the cortical bone of the distal tibia, however this has not been definitively established. Two current theories are:
- The pain is secondary to inflammation of the periosteum as a result of excessive traction of the tibialis posterior or soleus, supported by bone scintigraphy findings of a broad linear band of increased uptake along the medial tibial periosteum. But a case-controlled ultrasound based study which compared periosteal and tendinous edema of athletes with and without medial tibial stress syndrome found no difference between the groups.
- Bony overload injury, with resultant microdamage and targeted remodeling. A study evaluating tibia biopsy specimens from the painful area of six athletes suffering from medial tibial stress syndrome gave only equivocal support for this theory. Linear microcracks were found in only three specimens and there was no associated repair reaction[6].
Clinical Presentation and Assessment[edit | edit source]
| KEY POINTS FOR ASSESSMENT MTSS[3] | |
|---|---|
| HISTORY |
|
| PHYSICAL EXAMINATION |
|
| IMAGING | MRI: Periosteal reaction and edema |
| TREATMENT | See later in page |
Watch this video on MTSS.
Management[edit | edit source]
Management of MTSS is conservative, focusing on rest and activity modification with less repetitive, load-bearing exercise. No specific recommendations on the duration of rest required for resolution of symptoms, and it is likely variable depending on the individual.
Other therapies available (with low-quality evidence) include iontophoresis, phonophoresis, ice massage, ultrasound therapy, periosteal pecking, and extracorporeal shockwave therapy. A recent study on naval recruits showed prefabricated Introduction to Orthotics reduced MTSS[2].
Complications: Recurrence common after resumption of heavy activity.[9]
Physical Therapy Management[edit | edit source]
Patient education and a graded loading exposure program seem the most logical treatments.[7] Conservative therapy should initially aim to correct functional gait, and biomechanical overload factors.[3]Recently ‘running retraining’ has been advocated as a promising treatment strategy and graded running programme has been suggested as a gradual tissue-loading intervention.[3]
Prevention of MTSS was investigated in few studies and shock-absorbing insoles, pronation control insoles, and graduated running programs were advocated.[3]
Over-stress avoidance is the main preventive measure of MTSS or shin-splints. The main goals of shin-splints treatment are pain relieve and return to pain‑free activities.[10]
Acute phase[edit | edit source]
2-6 weeks of rest combined with medication is recommended to improve the symptoms and for a quick and safe return after a period of rest. NSAIDs and Acetaminophen are often used for analgesia. Also cryotherapy with Ice-packs and eventually analgesic gels can be used after exercise for a period of 20 minutes.
- There are a number of physical therapy modalities to use in the acute phase but there is no proof that these therapies such as ultrasound, soft tissue mobilization, electrical stimulation[11] would be effective.[4] A corticoid injection is contraindicated because this can give a worse sense of health. Because the healthy tissue is also treated. A corticoid injection is given to reduce the pain, but only in connection with rest.[5]
- Prolonged rest is not ideal for an athlete.
Subacute phase[edit | edit source]
The treatment should aim to modify training conditions and to address eventual biomechanical abnormalities. Change of training conditions could be decreased running distance, intensity and frequency and intensity by 50%. It is advised to avoid hills and uneven surfaces.
- During the rehabilitation period the patient can do low impact and cross-training exercises (like running on a hydro-gym machine). After a few weeks athletes may slowly increase training intensity and duration and add sport-specific activities, and hill running to their rehabilitation program as long as they remain pain-free.
- A stretching and strengthening (eccentric) calf exercise program can be introduced to prevent muscle fatigue. [12][13][14] Patients may also benefit from strengthening core hip muscles. Developing core stability with strong abdominal, gluteal, and hip muscles can improve running mechanics and prevent lower-extremity overuse injuries. [14]
- Proprioceptive balance training is crucial in neuromuscular education. This can be done with a one-legged stand or balance board. Improved proprioception will increase the efficiency of joint and postural-stabilizing muscles and help the body react to running surface incongruities, also key in preventing re-injury.[14]
- Choosing good shoes with good shock absorption can help to prevent a new or re-injury. Therefore it is important to change the athlete's shoes every 250-500 miles, a distance at which most shoes lose up to 40% of their shock-absorbing capabilities.
In case of biomechanical problems of the foot, individuals may benefit from Introduction to Orthotics. An over-the-counter orthosis (flexible or semi-rigid) can help with excessive foot pronation and pes planus. A cast or a pneumatic brace can be necessary in severe cases.[4] - Manual therapy can be used to control several biomechanical abnormalities of the spine, sacro-illiacal joint and various muscle imbalances. They are often used to prevent relapsing to the old injury.
- There is also acupuncture, ultrasound therapy injections and extracorporeal shock-wave therapy but their efficiency is not yet proved.
Differential Diagnosis[edit | edit source]
| Condition | Characteristics | Tissue origin |
| Anterior tibial stress syndrome | Vague, diffuse pain along anterolateral tibia, worse at beginning of exercise that decreases during training | Periosteum |
| Medial tibial stress syndrome | Vague, diffuse pain along middle-distal tibia, worse at beginning of exercise, that decreases during training |
| Tibial/fibular stress fracture | Pain with running, point tenderness over fracture site, "dreaded black line" on lateral x-ray | Bone |
| Exertional compartment syndrome | Symptoms begin 10min into exercise andresolve 30min after exercise, sensory or motor loss, elevated anterior compartment pressures | Muscle and fascia |
| Leg Tendinopathy | May be Achilles tendon, peroneal tendon, or tibialis posterior | Tendon |
| Sural or SPN entrapment | Dermatomal distribution of symptoms | Nerve |
| Lumbar radiculopathy | Worse with lumbar tension position (sitting) |
| Popliteal artery entrapment | Diagnosed with vascular studies | Blood vessel |
Clinical Bottom Line[edit | edit source]
‘Shin splints’ is a vague term that implicates pain and discomfort in the lower leg, caused by repetitive loading stress. There can be all sorts of causes to this pathology according to different researches. Therefore, a good knowledge of the anatomy is always important, but it’s also important you know the other disorders of the lower leg to rule out other possibilities, which makes it easier to understand what’s going wrong. Also a detailed screening of known’s risk factors, intrinsic as well as extrinsic, to recognize factors that could add to the cause of the condition and address these problems.
References[edit | edit source]
- ↑ Radiopedia Medial tibial stress syndrome Available: https://radiopaedia.org/articles/medial-tibial-stress-syndrome-1(accessed 2.6.2022)
- ↑ 2.0 2.1 2.2 2.3 McClure CJ, Oh R. Medial Tibial Stress Syndrome. 2019 Available:https://www.ncbi.nlm.nih.gov/books/NBK538479/ (accessed 2.6.2022)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Lohrer, H., Malliaropoulos, N., Korakakis, V., & Padhiar, N. Exercise-induced leg pain in athletes: diagnostic, assessment, and management strategies. The Physician and sports medicine. 2018
- ↑ 4.0 4.1 4.2 4.3 Galbraith, R. M., & Lavallee, M. E. Medial tibial stress syndrome: conservative treatment options. Current reviews in musculoskeletal medicine. 2009; 2(3): 127-133.
- ↑ 5.0 5.1 Broos P. Sportletsels : aan het locomotorisch apparaat. Leuven: Garant, 1991. (Level of Evidence: 5)
- ↑ 6.0 6.1 Milgrom C, Zloczower E, Fleischmann C, Spitzer E, Landau R, Bader T, Finestone AS. Medial tibial stress fracture diagnosis and treatment guidelines. Journal of science and medicine in sport. 2021 Jun 1;24(6):526-30. (accessed 2.6.2022)
- ↑ 7.0 7.1 Winters, M. Medial tibial stress syndrome: diagnosis, treatment and outcome assessment (PhD Academy Award). Br J Sports Med. 2018
- ↑ Thacker, S. B., Gilchrist, J., Stroup, D. F., & Kimsey, C. D. The prevention of shin splints in sports: a systematic review of literature. Medicine & Science in Sports & Exercise. 2002; 34(1): 32-40.
- ↑ 9.0 9.1 Ortho bullets Tibial Stress Syndrome (Shin Splints) Available: https://www.orthobullets.com/knee-and-sports/3108/tibial-stress-syndrome-shin-splints(accessed 2.6.2022)
- ↑ Alfayez, S. M., Ahmed, M. L., & Alomar, A. Z. A review article of medial tibial stress syndrome. Journal of Musculoskeletal Surgery and Research. 2017; 1(1): 2. (Level of Evidence: 4)
- ↑ Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Medicine. 1998; 26(4):265-279.
- ↑ Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–416. (Level of evidence 3A)
- ↑ Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints’. Phys Sportsmed. 2002;30(6):29–36.(Level of Evidence: 3a)
- ↑ 14.0 14.1 14.2 DeLee J, Drez D, Miller M. DeLee and Drez’s orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders. 2003:2155–2159.(Level of Evidence: 5)