Metacarpal Fractures: Difference between revisions
No edit summary |
No edit summary |
||
| Line 50: | Line 50: | ||
== Resources <br> == | == Resources <br> == | ||
[http://www.wheelessonline.com/ortho/hand_and_metacarpal_fractures Hand and Metacarpal Fractures] | |||
== Case Studies == | == Case Studies == | ||
Revision as of 02:39, 15 July 2013
Original Editor - Tim Yun and Andrew Slegel as part of the Temple University EBP Project
Top Contributors - Tim Yun, Debby Decock, Chrysolite Jyothi Kommu, Admin, Lucinda hampton, Andrew Slegel, Marie Avau, Kim Jackson, Rachael Lowe, Scott A Burns, Johnathan Fahrner, Shreya Pavaskar, 127.0.0.1, Anas Mohamed, Mila Andreew, Naomi O'Reilly and WikiSysop
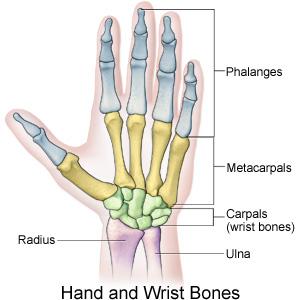
Clinically Relevant Anatomy
[edit | edit source]
The five metacarpal bones form the skeleton of the palm of the hand between the carpal bones and the phalanges. Each are comprised of a base, shaft, and head. The proximal bases of the metacarpals articulate with the carpal bones, and the distal heads of the metacarpals articulate with the proximal phalanges and form the knuckles. The 1st metacarpal (of the thumb) is the thickest and shortest of these bones. The 3rd metacarpal is distinguished by a styloid process on the lateral side of its base. Soft tissues generally involved with fractures include cartilage, joint capsule, ligaments, fascia, and the dorsal hood fibers. With severe polytrauma cases, the tendons and nerves adjacent to the fracture can also be injured[1].
Mechanism of Injury / Pathological Process
[edit | edit source]
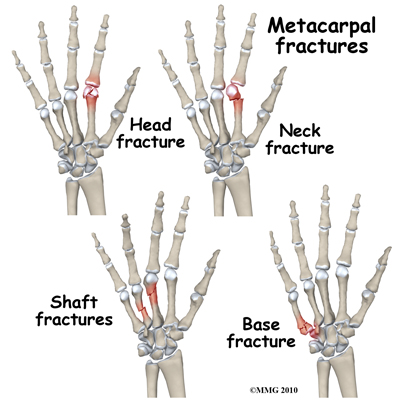
Metacarpal Base Fractures: These fractures are intra-articular and result from high forces (violent accidents), direct blows, or crushing injuries that disrupt the rigid carpal ligaments, or overwhelm the normal flexibility of the ulnar metacarpals. They also occur with an avulsion of the wrist flexors or extensors, that insert on the metacarpal base, resulting from a direct blow or torsional injury. The most common occurrence is at the 5th metacarpal-hamate articulation. The healing rate varies from three to six weeks[1].
Metacarpal Shaft Fractures: These fractures are extra-articular and are caused by longitudinal compression, torsion, or direct impact that may result from a fall, blow, or crushing force that usually angulates dorsally. They are described by the fracture configuration as transverse, oblique, spiral, or comminuted. Metacarpal shaft fractures are slower to heal than the more distal or proximal locations because of the predominantly cortical bone found there. The healing rate varies from three to seven weeks[1].
Metacarpal Neck Fractures: Most common metacarpal fracture. The weakest point of the metacarpal bone is the extra-articular neck. These fractures result from a compression force such as a direct blow with a closed fist. The 4th and 5th metacarpals are most often involved and are referred to as a “fighter’s” or “boxer’s” fracture. Trauma causes the fractured metacarpal head to displace with volar angulation. The healing rate is three to five weeks[1].
Metacarpal Head Fractures: These fractures are intra-articular and are caused by direct impact and high axial loads that can involve avulsion of the collateral ligaments, including a fracture fragment, fracture of one or both condyles, or shattering of the joint surface into many small, comminuted pieces[1].
Clinical Presentation[edit | edit source]
Metacarpal fractures represent 35% of all hand fractures and up to 85% occur in men2,3. Sports account for 12.8% of all fractures, with simple falls among elderly people (45.3%) and direct blows/assault (14.1%) being the two major causes[2]. Due to their good blood supply, metacarpal fractures heal rapidly with osseous restoration in six weeks1. Fractures of these bones are described at four distinct locations: the base, shaft, neck and head. Of all hand fractures, fractures of the 5th metacarpal bone at the level of the neck are the most common, accounting for 16-34%[3],[4]. Patients with metacarpal fractures generally present with pain, swelling, ecchymosis or discoloration, limitation of movement, and often deformity. Knuckle asymmetry may be observed, and the knuckle may appear to be missing. Finger misalignment may also be noted. In patients with a metacarpal head fracture, axial compression of the extended digit causes severe discomfort. In patients with a metacarpal base fracture, movement of the wrist or longitudinal compression exacerbates the pain. Any metacarpal fracture angulation can produce a pseudo-claw deformity.
Diagnostic Procedures[edit | edit source]
Physical examination and radiographs can be considered the definitive standard for diagnosis of metacarpal fractures. Physical examination of a suspected metacarpal fracture should concentrate on hand deformity, tenderness, digit malrotation, and presence of open wounds. Painful range of motion, point specific bone tenderness and ecchymosis should be considered red flags for fractures during a clinical physical examination. Routine radiographs include three views: anteroposterior, lateral, and oblique. These views assist in properly assessing angulation of fracture fragments as well as involved joint surfaces. Computed Tomography scans, or CT scans, may be ordered to evaluate complicated fractures[3],[5].
Outcome Measures[edit | edit source]
-Grip Strength
-Range of motion
-Disabilities of the Arm, Shoulder, and Hand score (QuickDASH)
-Michigan Hand Outcome Questionnaire (MHO)
-Patient Evaluation Measure (PEM)
Management / Interventions
[edit | edit source]
Fracture must be stable in order to heal.
Stable fractures are those that will maintain their position at rest and will not lose approximation with muscle tension or controlled motion. These fractures only require protective immobilization to allow healing. Closed methods of supports for 2-3 weeks, then use removable splint for controlled motion.
Potential unstable fractures are those that are aligned, but may get misaligned with certain positions or tension. These are treated with immobilization that maintains reduction or restriction of motion towards position of instability. As healing occurs, immobilization can be modified to allow incremental increases in ROM.
Unstable fractures are those that do not maintain reduction. Displacement occurs even with immobilization. Fixation devices are warranted[1],[6].
Two facts must be provided with therapy referral: date of fracture and method of fixation. Date of fracture provides a timetable on where the bone healing process is. Knowing the method of fixation will determine when motion can be introduced. Open reduction fixations can begin AROM earlier[1].
Edema Control: Patient should be educated on edema control early on in treatment. Rest, ice, compression, and elevation should be emphasized. MP joint flexion exercises while fingers are adducted will promote venous return via intrinsic muscle pumping[1].
Tendon glides: Flexor differential gliding of the digitorum superficialis and profundus tendons are important in order to prevent adhesions and maintain AROM are recommended[1],[6].
Specific Fracture Regions
Metacarpal Base Fractures: 4-6 weeks of closed reduction casting for non-displaced or minimally displaced fractures. ORIF for displaced fractures to restore approximation. Prolonged immobilization is necessary in order to prevent deformity from force from wrist tendon insertions[1].
Metacarpal Shaft Fractures: Stable, non-displaced fractures can be treated closed. Incorporate 3 points of reduction pressure and allow for free active joint motion. Unstable fractures require additional support such as radial/ulnar gutter splints on displaced metacarpal and adjacent uninvolved metacarpal. Early motion is key[1].
Metacarpal Neck Fractures: Once head is properly aligned with shaft, hold MP joint in over 70 degrees flexion, in order that collateral ligaments will help secure head in place. For unstable fractures, a closed reduction with percutaneous pining with K-wires is recommended. At 4-6 weeks when K-wires are removed, full AROM should be regained[1].
Metacarpal Head Fractures: For collateral ligament avulsions, if non-displaced, splint for 4-6 weeks with MP joint in 50-70 degrees flexion. If displaced, ORIF with fixation that allows for early protected motion is recommended. Comminuted fractures can be treated with closed immobilization in a radial/ulnar gutter splint with MP joints flexed at 70 degrees[1].
Differential Diagnosis
[edit | edit source]
Hand dislocation
Metacarpophalangeal joint dislocation
Skiers’ Thumb
Key Evidence[edit | edit source]
Hardy MA. Principles of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation Concepts. Journal of Orthopedic and Sports Physical Therapy. 2004; 34:781-791.
Resources
[edit | edit source]
Case Studies[edit | edit source]
Boulton CL, Salzler M, Mudgal CS. Intramedullary Cannulated Headless Screw Fixation of a Comminuted Subcapital Metacarpal Fracture: Case Report. J Hand Surg 2010;
35A:1260 –1263.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NYYLF8F8KblIH5S1MPLpP-NG_uMgg7Tmbfbm_ghG1wxIOdEE2|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Hardy MA. Principles of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation Concepts. Journal of Orthopedic and Sports Physical Therapy. 2004; 34:781-791.
- ↑ Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury, Int. J. Care Injured (2008) 39, 1377-1383.
- ↑ 3.0 3.1 Freidrich, JB, Vedder, NB. An Evidence-Based Approach to Metacarpal Fractures. Plast. Reconstr. Surg. 126: 2205, 2010.
- ↑ Gudmundsen TE, Borgen L. Fractures of the fifth metacarpal. Acta Radiol 2009;50:fckLR296-300.
- ↑ Kozin SH, Thoder JJ, Leiberman G. Operative Treatment of Metacarpal and Phalangeal Shaft Fractures. J Am Acad Orthop Surg 2000;8:111-121.
- ↑ 6.0 6.1 Lastayo PC, Winters KM, Hardy M. Fracture Healing: Bone Healing, Fracture Management, and Current Concepts Related to the Hand. J Hand Ther. 2003;16:81 - 93.