Moyamoya Disease: Difference between revisions
Wendy Walker (talk | contribs) No edit summary |
Wendy Walker (talk | contribs) No edit summary |
||
| (11 intermediate revisions by the same user not shown) | |||
| Line 6: | Line 6: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Moyamoya Disease is a disorder of some of the blood vessels in the brain: the internal carotid arteries, and the arteries which branch from them. It is a rare cause of Stroke and TIAs. | Moyamoya Disease [MMD] is a disorder of some of the blood vessels in the brain: the internal carotid arteries, and the arteries which branch from them, the Circle of Willis<ref>Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N. Engl. J. Med. 2009;360(12):1226–1237.</ref>. It is a rare cause of Stroke and TIAs. Moyamoya Syndrome also has the same pathology and presentation. | ||
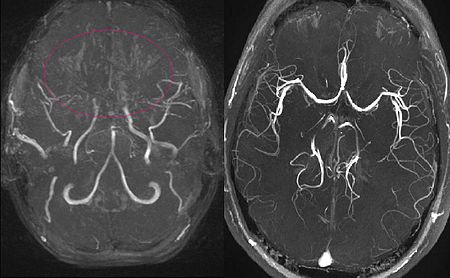
[[File:MRA Moya-moya-disease.JPG|alt=2 images, both MIP reconstructed MR angiographies; one is that of an 11 year old girl with Moyamoya Disease, which shows the characteristic occluded cranial arteries, and the other image shows a healthy subject for comparison. | |||
Moyamoya Disease was named in 1969 by Suzuki and Takaku<ref>Suzuki J., Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch. Neurol. 1969;20(3):288–299.</ref> becuse the appearance on angiography is reminiscent of a "puff of smoke" (the Japanese word moyamoya is tranlated as "something hazy like a puff of smoke") due to the formation of the colateral vessels. | |||
[[File:MRA Moya-moya-disease.JPG|alt=2 images, both MIP reconstructed MR angiographies; one is that of an 11 year old girl with Moyamoya Disease, which shows the characteristic occluded cranial arteries, and the other image shows a healthy subject for comparison.|The image on the left: MIP reconstructed MR angiography of a 11 year old girl with Moyamoya Disease. The image on the right: a healthy subject for comparison. |frame]] | |||
It can also be referred to as Progressive Intracranial Occlusive Arteropathy, or Progressive Intracranial Arterial Occlusion. | It can also be referred to as Progressive Intracranial Occlusive Arteropathy, or Progressive Intracranial Arterial Occlusion. | ||
==== Incidence ==== | |||
The incidence of Moyamoya disease is higher in Asia than in Europe, America, Africa and Latin America, with Japan having the highest incidence<ref>Kuriyama S., Kusaka Y., Fujimura M., Wakai K., Tamakoshi A., Hashimoto S., Tsuji I., Inaba Y., Yoshimoto T. Prevalence and clinicoepidemiological features of moyamoya disease in Japan: Findings from a nationwide epidemiological survey. Stroke. 2008;39(1):42–47.</ref> followed by China and South Korea. | |||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
The affected arteries become increasingly constricted with time, and a collateral circulation develops around the constricted arteries to compensate for the blockages. The condition is | The affected arteries become increasingly constricted with time, and a collateral circulation develops around the constricted arteries to compensate for the blockages. The condition is a non-atherosclerotic progressive vaso-occlusive disease involving the terminal supraclinoid internal carotid arteries and circle of Willis. | ||
The aetiology of Moyamoya Disease is linked to several genes that are involved in formation and structure of blood vessels. Moyamoya Syndrome occurs when another underlying condition causes narrowing and occlusion of the carotid artery; these conditions can include intracranial atherosclerosis, cranial radiation, sickle cell disease, meningitis and has also been linked to several genetic diseases including Down Syndrome, Marfan Disease and Neurofibramatosis.<br> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 18: | Line 25: | ||
The patient often presents either: | The patient often presents either: | ||
* in | * in childhood (two-thirds of patients) OR | ||
* in adults in their 30s or 40s (one-third of patients) | * in adults in their 30s or 40s (one-third of patients) | ||
In children, hemispheric ischaemic strokes are the most common presentation; in adults haemorrhage from the abnormal vessels is more common<ref>Duan, Lian; Bao, Xiang-Yang; Yang, Wei-Zhong; Shi, Wan-Chao; Li, De-Sheng; Zhang, Zheng-Shan; Zong, Rui; Han, Cong; Zhao, Feng; Feng, Jie (2012). [[/doi.org/10.1161/STROKEAHA.111.621300|"Moyamoya Disease in China"]]. ''Stroke''. '''43''' (1): 56–60.</ref>. | In children, hemispheric ischaemic strokes are the most common presentation; in adults haemorrhage from the abnormal vessels is more common<ref>Duan, Lian; Bao, Xiang-Yang; Yang, Wei-Zhong; Shi, Wan-Chao; Li, De-Sheng; Zhang, Zheng-Shan; Zong, Rui; Han, Cong; Zhao, Feng; Feng, Jie (2012). [[/doi.org/10.1161/STROKEAHA.111.621300|"Moyamoya Disease in China"]]. ''Stroke''. '''43''' (1): 56–60.</ref>. | ||
Stroke or Transient Ischaemic Attack are the most common presentations, although some patients present with headaches or seizures<ref>Kleinloog, R (May 2012). "Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review". ''J Neurol Neurosurg Psychiatry''. '''83''' (5): 531–6.</ref>. | [[Stroke]] or [[Transient Ischaemic Attack (TIA)|Transient Ischaemic Attack]] are the most common presentations, although some patients present with headaches or seizures<ref>Kleinloog, R (May 2012). "Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review". ''J Neurol Neurosurg Psychiatry''. '''83''' (5): 531–6.</ref>. | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
< | * Digital subtraction angiography (DSA) is the criterion standard for diagnosis of Moyamoya Disease<ref>Hwang I., Cho W.S., Yoo R.E., Kang K.M., Yoo D.H., Yun T.J., Choi S.H., Kim J.H., Kim J.E., Sohn C.H. Revascularization evaluation in adult-onset moyamoya disease after bypass surgery: superselective arterial spin labeling perfusion mri compared with digital subtraction angiography. Radiology. 2020;297(3):630–637. </ref>. Digital subtraction angiography is able to evaluate the stenosis in the terminal section of the internal carotid artery, as well as the degree of compensation from the external carotid artery and the posterior circulation<ref>onasia S., Ciccio G., Smajda S., Weil A.G., Chaalala C., Blanc R., Reinert M., Piotin M., Bojanowski M., Robert T. | ||
[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6975369/ Angiographic analysis of natural anastomoses between the posterior and anterior cerebral arteries in moyamoya disease and syndrome]. AJNR Am. J. Neuroradiol. 2019;40(12):2066–2072. doi: 10.3174/ajnr.A6291.</ref>. | |||
* Various different types of MRI scanning can also give information in cases of Moyamoya Disease<ref>Lin Y.H., Kuo M.F., Lu C.J., Lee C.W., Yang S.H., Huang Y.C., Liu H.M., Chen Y.F., | |||
[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7028633/ Standardized MR perfusion scoring system for evaluation of sequential perfusion changes and surgical outcome of moyamoya disease]. AJNR Am. J. Neuroradiol. 2019;40(2):260–266.</ref>. | |||
== Physiotherapy Intervention == | |||
Physiotherapy techniques, particularly neurological physiotherapy interventions, are appropriate for patients with stroke caused by Moyamoya Disease. Please see the following pages for more information: | |||
* [[Stroke: physiotherapy treatment approaches]] | |||
* [[Stroke: hand rehabilitation]] | |||
* [[Gait training in Stroke]] | |||
== Management / Interventions<br> == | == Management / Interventions<br> == | ||
Moyamoya Disease is progressive, and surgical revascularisation is the only effective therapy for patients to reduce the risk of subsequent strokes<ref>Acker G, Fekonja L, Vajkoczy P. | |||
Surgical management of moyamoya disease. Stroke 2018;49:476–82 10.1161</ref><ref>Teo MK, Madhugiri VS, Steinberg GK. | |||
Editorial: direct versus indirect bypass for moyamoya disease—ongoing controversy. J Neurosurg 2017;126:1520–22</ref><ref>Macyszyn L, Attiah M, Ma TS, et al.. Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg 2017;126:1523–29</ref><ref>Uchino H, Kim JH, Fujima N, et al.. | |||
Synergistic interactions between direct and indirect bypasses in combined procedures: the significance of indirect bypasses in moyamoya disease. Neurosurgery 2017;80:201–09 10.1227</ref>. | |||
In Moyamoya syndrome, medical therapeutic techniques can be used to help manage the condition, particularly anti-platelet medications. | |||
== Resources <br> == | == Resources <br> == | ||
A very useful summary of the aetiology, diagnosis and surgical treatment of Moyamoya: | |||
{{#ev:youtube|VYiUbbmbk0Y}} | |||
This video gives details of a patient with Moyamoya disease, and includes interviews with the patient and her surgeon: | |||
{{#ev:youtube|A6nb-kM9xNc}} | |||
== References == | == References == | ||
<references /> | <references /> | ||
Latest revision as of 20:42, 18 April 2024
Clinically Relevant Anatomy[edit | edit source]
Moyamoya Disease [MMD] is a disorder of some of the blood vessels in the brain: the internal carotid arteries, and the arteries which branch from them, the Circle of Willis[1]. It is a rare cause of Stroke and TIAs. Moyamoya Syndrome also has the same pathology and presentation.
Moyamoya Disease was named in 1969 by Suzuki and Takaku[2] becuse the appearance on angiography is reminiscent of a "puff of smoke" (the Japanese word moyamoya is tranlated as "something hazy like a puff of smoke") due to the formation of the colateral vessels.
It can also be referred to as Progressive Intracranial Occlusive Arteropathy, or Progressive Intracranial Arterial Occlusion.
Incidence[edit | edit source]
The incidence of Moyamoya disease is higher in Asia than in Europe, America, Africa and Latin America, with Japan having the highest incidence[3] followed by China and South Korea.
Mechanism of Injury / Pathological Process
[edit | edit source]
The affected arteries become increasingly constricted with time, and a collateral circulation develops around the constricted arteries to compensate for the blockages. The condition is a non-atherosclerotic progressive vaso-occlusive disease involving the terminal supraclinoid internal carotid arteries and circle of Willis.
The aetiology of Moyamoya Disease is linked to several genes that are involved in formation and structure of blood vessels. Moyamoya Syndrome occurs when another underlying condition causes narrowing and occlusion of the carotid artery; these conditions can include intracranial atherosclerosis, cranial radiation, sickle cell disease, meningitis and has also been linked to several genetic diseases including Down Syndrome, Marfan Disease and Neurofibramatosis.
Clinical Presentation[edit | edit source]
The patient often presents either:
- in childhood (two-thirds of patients) OR
- in adults in their 30s or 40s (one-third of patients)
In children, hemispheric ischaemic strokes are the most common presentation; in adults haemorrhage from the abnormal vessels is more common[4].
Stroke or Transient Ischaemic Attack are the most common presentations, although some patients present with headaches or seizures[5].
Diagnostic Procedures[edit | edit source]
- Digital subtraction angiography (DSA) is the criterion standard for diagnosis of Moyamoya Disease[6]. Digital subtraction angiography is able to evaluate the stenosis in the terminal section of the internal carotid artery, as well as the degree of compensation from the external carotid artery and the posterior circulation[7].
- Various different types of MRI scanning can also give information in cases of Moyamoya Disease[8].
Physiotherapy Intervention[edit | edit source]
Physiotherapy techniques, particularly neurological physiotherapy interventions, are appropriate for patients with stroke caused by Moyamoya Disease. Please see the following pages for more information:
Management / Interventions
[edit | edit source]
Moyamoya Disease is progressive, and surgical revascularisation is the only effective therapy for patients to reduce the risk of subsequent strokes[9][10][11][12].
In Moyamoya syndrome, medical therapeutic techniques can be used to help manage the condition, particularly anti-platelet medications.
Resources
[edit | edit source]
A very useful summary of the aetiology, diagnosis and surgical treatment of Moyamoya:
This video gives details of a patient with Moyamoya disease, and includes interviews with the patient and her surgeon:
References[edit | edit source]
- ↑ Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N. Engl. J. Med. 2009;360(12):1226–1237.
- ↑ Suzuki J., Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch. Neurol. 1969;20(3):288–299.
- ↑ Kuriyama S., Kusaka Y., Fujimura M., Wakai K., Tamakoshi A., Hashimoto S., Tsuji I., Inaba Y., Yoshimoto T. Prevalence and clinicoepidemiological features of moyamoya disease in Japan: Findings from a nationwide epidemiological survey. Stroke. 2008;39(1):42–47.
- ↑ Duan, Lian; Bao, Xiang-Yang; Yang, Wei-Zhong; Shi, Wan-Chao; Li, De-Sheng; Zhang, Zheng-Shan; Zong, Rui; Han, Cong; Zhao, Feng; Feng, Jie (2012). "Moyamoya Disease in China". Stroke. 43 (1): 56–60.
- ↑ Kleinloog, R (May 2012). "Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review". J Neurol Neurosurg Psychiatry. 83 (5): 531–6.
- ↑ Hwang I., Cho W.S., Yoo R.E., Kang K.M., Yoo D.H., Yun T.J., Choi S.H., Kim J.H., Kim J.E., Sohn C.H. Revascularization evaluation in adult-onset moyamoya disease after bypass surgery: superselective arterial spin labeling perfusion mri compared with digital subtraction angiography. Radiology. 2020;297(3):630–637.
- ↑ onasia S., Ciccio G., Smajda S., Weil A.G., Chaalala C., Blanc R., Reinert M., Piotin M., Bojanowski M., Robert T. Angiographic analysis of natural anastomoses between the posterior and anterior cerebral arteries in moyamoya disease and syndrome. AJNR Am. J. Neuroradiol. 2019;40(12):2066–2072. doi: 10.3174/ajnr.A6291.
- ↑ Lin Y.H., Kuo M.F., Lu C.J., Lee C.W., Yang S.H., Huang Y.C., Liu H.M., Chen Y.F., Standardized MR perfusion scoring system for evaluation of sequential perfusion changes and surgical outcome of moyamoya disease. AJNR Am. J. Neuroradiol. 2019;40(2):260–266.
- ↑ Acker G, Fekonja L, Vajkoczy P. Surgical management of moyamoya disease. Stroke 2018;49:476–82 10.1161
- ↑ Teo MK, Madhugiri VS, Steinberg GK. Editorial: direct versus indirect bypass for moyamoya disease—ongoing controversy. J Neurosurg 2017;126:1520–22
- ↑ Macyszyn L, Attiah M, Ma TS, et al.. Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg 2017;126:1523–29
- ↑ Uchino H, Kim JH, Fujima N, et al.. Synergistic interactions between direct and indirect bypasses in combined procedures: the significance of indirect bypasses in moyamoya disease. Neurosurgery 2017;80:201–09 10.1227