Neck Pain Tool-kit: Step 3: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 347: | Line 347: | ||
==== Chiu 2005<ref name="Chiu 2005">Chiu T, Huiu-Chan C, and Cheing G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabil 2005;19:850-60.</ref> ==== | ==== Chiu 2005<ref name="Chiu 2005">Chiu T, Huiu-Chan C, and Cheing G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabil 2005;19:850-60.</ref> ==== | ||
*An intensive neck exercise program using the Multi Cervical Rehabilitation Unit (MCRU) (Pollock et al | *An intensive neck exercise program using the Multi Cervical Rehabilitation Unit (MCRU) (Pollock 1993<ref name="Pollock 1993">Pollock ML, Graves JE, Bamman MM et al.Frequency and volume of resistance training: Effect on cervical extension strength. Arch Phys Med Rehabil 1993;74:1080-86.</ref>) and the exercise protocol of (Jull 1999<ref name="Jull 1999">Jull GA, Barrett C, Magee R, Ho P. Further clarification of musculoskeletal dysfunction in cervical headache. Cephalalgia 1999;19:179-85.</ref>) | ||
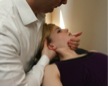
*Activation of the deep neck muscles aimed to enhance their ability for active stabilization for warm-up (a) | *Activation of the deep neck muscles aimed to enhance their ability for active stabilization for warm-up ('''a''') | ||
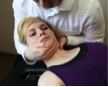
*Flexion and extension of neck using the MCRU as a warm-up exercise for the superficial neck muscles using resistance equal to approximately 20% of the peak isometric muscle strength as warm-up (b) | *Flexion and extension of neck using the MCRU as a warm-up exercise for the superficial neck muscles using resistance equal to approximately 20% of the peak isometric muscle strength as warm-up ('''b''') | ||
*Full flexion and extension within pain tolerance (b) | *Full flexion and extension within pain tolerance ('''b''') | ||
*The dynamic weight load was calculated to be about 30% of the peak isometric muscle strength | **The dynamic weight load was calculated to be about 30% of the peak isometric muscle strength | ||
*The weight load was increased by approximately 5%, when a set of 12 or more repetitions had been achieved. | **The weight load was increased by approximately 5%, when a set of 12 or more repetitions had been achieved. | ||
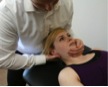
*Activation of the deep neck flexor muscles (c) | *Activation of the deep neck flexor muscles ('''c''') | ||
*the patient lay down in the supine position with the weight of the head and the cervical spine supported by towels under the occiput in a neutral position | **the patient lay down in the supine position with the weight of the head and the cervical spine supported by towels under the occiput in a neutral position | ||
*An air-filled pressure sensor (Stablizer, Chattanooga South Pacific, Australia) was used to monitor the subtle flattening of the cervical lordosis that was expected to occur with contraction of deep neck flexors. | **An air-filled pressure sensor (Stablizer, Chattanooga South Pacific, Australia) was used to monitor the subtle flattening of the cervical lordosis that was expected to occur with contraction of deep neck flexors. | ||
*The sensor was placed suboccipitally behind the neck and inflated to 20 mmHg | **The sensor was placed suboccipitally behind the neck and inflated to 20 mmHg | ||
*The patient was instructed to slowly nod the head in an action indicating 'yes', so as to raise the pressure to a level that could be held steadily for 10 seconds | **The patient was instructed to slowly nod the head in an action indicating 'yes', so as to raise the pressure to a level that could be held steadily for 10 seconds | ||
*A 15 second break was given between each 10 second hold and this pattern was repeated for 10 minutes or until patient was unable to hold the contraction | **A 15 second break was given between each 10 second hold and this pattern was repeated for 10 minutes or until patient was unable to hold the contraction | ||
{| width="600" border="0" cellpadding="1" cellspacing="1" | |||
|- | |||
| [[Image:NeckPainToolkit_Step3_Chron_StrEx_A.jpg|thumb|center|(a) Activation of deep neck flexion muscles in supine ]] | |||
| [[Image:NeckPainToolkit_Step3_Chron_StrEx_B.jpg|thumb|center|(b) MCRU]] | |||
| [[Image:NeckPainToolkit_Step3_Chron_StrEx_C.jpg|thumb|center|(c) Deep neck flexor activation with pressure biofeedback]] | |||
| width="25%" | | |||
|} | |||
==== Bronfort 2001 ==== | ==== Bronfort 2001 ==== | ||
Revision as of 18:19, 30 March 2012
This page is part of the 'Manual Therapy & Exercise for Neck Pain: Clinical Treatment Tool-kit' resource for clinical decision making, which provides evidence, techniques, and dosages for the use of manual therapy and exercise in the treatment of neck pain. Please see the main project page for further information, or to return to Step 1 to identify your patient. Otherwise, proceed to Step 3 below to inform your technique.
The techniques utilized in the positive trials investigating the use of manual therapy and exercise for the treatment of neck pain are presented below, organized by patient characteristics
- 3.1 Neck pain alone
- 3.2 Neck pain with cervicogenic headache
- 3.3 Whiplash associated disorder
- 3.4 Neck pain with radiculopathy
Once you have found the techniques most applicable to your patient, click on Step 4-inform your technique to see the techniques utilized in the positive studies for that patient population
3.1 Neck pain alone (non-specific)[edit | edit source]
Acute/subacute neck pain[edit | edit source]
- Click to go back to Step 1: Identify your patient
Thoracic manipulation[edit | edit source]
- Click to continue to Step 4: Consider dosage
Cleland 2007[1][edit | edit source]
- upper thoracic spine thrust manipulation targeting T1-T4(a)
- patient laces hands behind his/her neck
- therapist uses the patients elbow to flex spine down to the upper thoracic levels
- therapist stabilizes the inferior vertebrae using his/her manipulative hand and uses his/her chest to provide the thrust manipulation. If no pop is heard, a second attempt is made
- middle thoracic spine thrust manipulation targeting T5-T8 (b)
- patient clasps hands on opposite shoulder
- therapist flexes spine down to the target levels using the patients arms
- therapist provides the thrust manipulation through his/her chest. If no pop is heard, a second attempt is made
- Advice to maintain usual activities within the limits of pain
- Advice to maintain current medications
- Adjunct exercise
- place fingers over manubrium and place chin on the fingers
- rotate the head and neck as far as possible to alternating sides
- start using 5 fingers and progress to 4, 3, 2, and 1 finger as mobility improves
- 10 repetitions to each side, 3-4 times/day
Gonzalez-Iglesias 2009[2] [edit | edit source]
- seated distraction manipulation (c)
- patient seated with arms crossed over the chest and one hand over opposite shoulder and one hand over rib cage
- therapist places his/her upper chest at the level of the patient’s middle thoracic spine
- therapist grasps the patient’s elbows and flexes the thoracic spine until tension is felt
- a distraction manipulation was applied in an upward direction
- if no pop was heard, a second attempt was made
- adjunct electrothermal therapy
Subacute/chronic[edit | edit source]
Manual therapy and exercise[edit | edit source]
Bronfort 2001[3][edit | edit source]
- Spinal manipulation to the cervical and thoracic spine (Haldeman 1991[4]) with light soft-tissue massage as indicated to facilitate the spinal manipulative therapy
- Warm-up on a stationary bike with arm levers
- Light stretching as part of warm-up (a-c)
- Upper-body strengthening exercises (Dyrssen 1989[5])
- Push-ups (d)
- Dumbbell shoulder exercises (e-k)
- Dynamic neck exercises lying on table with headgear attached to a simple pulley system
- extension (l)
- flexion (m)
- rotation (n)
Hoving 2002[6][edit | edit source]
- An eclectic approach to manual therapy including several techniques used in western Europe, North America, and Australia, including those described by Cyriax, Kaltenborn, Maitland, and Mennel (Basmajian 1993[7]; Cookson 1979[8]; Gross 1996[9]).
- Techniques included:
- “hands-on” muscular mobilization techniques (aimed at improving soft tissue function)
- specific articular mobilization techniques (to improve overall joint function and decrease any restrictions in movement at single or multiple segmental levels in the cervical spine) (o-oo)
- coordination or stabilization techniques (to improve postural control, coordination, and movement patterns by using the stabilizing cervical musculature) (Van der 1993[10]) (pp-rr)
Jull 2002[11][edit | edit source]
- Manipulative therapy at the therapist’s discretion (Maitland 2000[12])(y-kk)
- low-velocity cervical joint mobilization techniques (in which the cervical segment is moved passively with rhythmical movements)
- high-velocity manipulation techniques
- Low load endurance exercises to train muscle control of the cervicoscapular region (Jull 1997[13])
- The subjects were first taught to perform a slow and controlled craniocervical flexion action aimed to target the deep neck flexor muscles (pp)
- They then trained to be able to hold progressively increasing ranges of craniocervical flexion using feedback from an air-filled pressure sensor placed behind the neck (qq).
- The muscles of the scapula, particularly the serratus anterior and lower trapezius, were trained using inner range holding exercises of scapular adduction and retraction, practiced initially in the prone lying position (ss)
- Training of these neck and scapular muscles also was incorporated into postural correction exercises performed regularly throughout the day in the sitting position. The subjects were trained to sit with a natural lumbar lordosis while gently retracting and adducting their scapulas and gently elongating their cervical spine to facilitate the longus colli (tt)
- Subsequently, isometric exercises using a low level of rotatory resistance were used to train the cocontraction of the neck flexors and extensors (uu)
- They also could be taught muscle lengthening exercises to address any muscle tightness assessed to be present (a-c)
Skargren 1998[14][edit | edit source]
- Each patient's treatment was at the discretion of the individual physiotherapist
- None of the physiotherapists was a specialist in manipulation.
Ylinen 2003[15][edit | edit source]
Endurance training group
- Neck flexor exercise performed by lifting the head up from the supine position (qq)
- Dynamic exercises for shoulders and upper extremities using dumbbells(2 sets of 20 repetitions with 2kg dumbbells)
- presses (e)
- shrugs (f)
- flyes (h)
- curls (i)
- bent-over rows (j)
- pullovers (k)
- Exercises for trunk and leg muscles against body weight
- squats (vv)
- sit-ups (ww)
- back extensions (xx)
- Stretching for neck, shoulder, and upper limb muscles (a-c, yy-ccc)
- Advice to perform aerobic exercise 3 times a week for a half hour (ddd,eee)
- A common multimodal rehabilitation program, including aspects commonly associated with traditional treatment: relaxation training, aerobic training, behavioral support to reduce fear of pain and improve exercise motivation, and lectures and practical exercises in ergonomics
- 4 sessions of physical therapy, which consisted mainly of massage and mobilization to alleviate neck pain and to enable those with severe neck pain to perform active physical exercises
- Every other session was performed at only half intensity to avoid excessive loading
Strength training group
- Neck exercises with an elastic rubber band performed in a sitting position at 80% of maximum isometric strength recorded at baseline and follow-up visits
- directly forward (fff)
- obliquely toward right and left (ggg)
- directly backward (hhh)
- Dynamic exercises for shoulders and upper extremities using dumbbells (1set of 15 repetitions with highest load possible)
- presses (e)
- shrugs (f)
- flyes (h)
- curls (i)
- bent-over rows (j)
- pullovers (k)
- Exercises for trunk and leg muscles against body weight
- squats (vv)
- sit-ups (ww)
- back extensions (xx)
- Stretching for neck, shoulder, and upper limb muscles (a-c, yy-ccc)
- Advice to perform aerobic exercise 3 times a week for a half hour (ddd, eee)
- A common multimodal rehabilitation program, including aspects commonly associated with traditional treatment: relaxation training, aerobic training, behavioral support to reduce fear of pain and improve exercise motivation, and lectures and practical exercises in ergonomics
- 4 sessions of physical therapy, which consisted mainly of massage and mobilization to alleviate neck pain and to enable those with severe neck pain to perform active physical exercises
- Every other session was performed at only half intensity to avoid excessive loading
Allison 2002[16][edit | edit source]
Neural treatment (Elvey 1997[17]). The treating physiotherapist could use any or all of the following interventions at his/her discretion.
- Cervical lateral glide (iii)
- The subject was positioned in supine, the shoulder slightly abducted with a few degrees of medial rotation, and the elbow flexed to approximately 90 such that the hands were resting on the subject’s chest or abdomen
- The physiotherapist gently supported the shoulder over the acromial region with one hand while holding and supporting the head and neck
- The technique involved a gentle controlled lateral glide to the contralateral side of pain in a slow oscillating manner up to a point in range where the first perception of resistance was felt by the therapist (and before the onset of pain).
- Shoulder girdle oscillation (jjj)
- The subject was positioned prone with the involved arm comfortably supported by the physiotherapist towards a position of hand behind the back.
- The physiotherapist placed the other hand over the acromial area.
- The technique involved a gentle oscillation of the shoulder girdle in a caudad cephalad direction. The range of oscillation was governed by the onset of first resistance perceived by the therapist in the caudad direction.
- The technique was progressed by performing the oscillation in gradually increased amounts of hand behind the back position.
- Muscle re-education
- Contract-relax techniques were performed into shoulder abduction and external rotation.
- This was progressed from a shoulder position of flexion/ adduction towards a position of abduction/external rotation comparable to a quadrant position in the scapular plane (Elvey and Hall, 1997).
- Home mobilisation
- Cervical spine side flexion was performed contralateral to the painful side with the shoulder in a position of abduction, and elbow resting on a table in a flexed position
- Active movements of shoulder abduction and/or external rotation in the same starting position as above was carried out if appropriate (kkk)
Brodin 1985[18]
[edit | edit source]
- superficial massage
- slight and relaxing traction (q)
- electrical stimulation
- 'cervical mobilization (Stoddard 1959[19]) (lll-rrr)
- ‘cervical school’
- education on anatomy and mechanical problems
- how to deal with practical problems such as lifting, carrying, and relaxation
- movements with the aim of improving muscular control of the cervical spine and shoulder girdle
Karlberg 1996[20][edit | edit source]
- Physiotherapy methods were chosen by the therapist based on analysis of different functions such as mobility, stability, muscle tension and tone, postural alignment and body awareness (Feldenkrais, 1987; Jacobson, 1938; Kaltenborn, 1993; Lewit, 1991)
- The purpose of the treatment was to reduce cervical discomfort, and it included soft tissue treatment, stabilization exercises of the trunk and cervical spine (pp,qq), passive (u-ff) and active mobilization (sss-vvv), relaxation techniques (www), home training programs and minor ergonomic changes at work
- The majority of the patients underwent several treatment modalities, depending on findings from the analysis mentioned above
Palmgren 2006[21][edit | edit source]
- Patients received information regarding basic anatomy and physiology of the spine, principles of ergonomics for neck pain patients, and basic instructions on how to exercise and cope with the pain. The clinical findings were explained and potential causes of pain were clarified
- The patients were told that neck pain generally has a benign, self-limiting natural course and that the healing process could be accelerated by simple, regular exercises and by avoiding immobility
- The choice of therapy and modality was pragmatic and based on the analysis of different functions such as mobility, muscle tension and tone, and each patient’s symptoms, but might include:
- high-velocity and low-amplitude techniques
- myofascial techniques
- spine-stabilizing exercises targeted toward hypomobile zygapophyseal joints in the cervical region and the cervicothoracic junction
- The spine stabilizing exercises consisted of:
- 4-5 minutes of jogging for a warm-up was performed (eee)
- Stretching of cervical and shoulder region (a-c, yy-ccc)
- Cervical isometrics in supine and seated (xxx-ffff)
Strengthening exercise[edit | edit source]
Chiu 2005[22][edit | edit source]
- An intensive neck exercise program using the Multi Cervical Rehabilitation Unit (MCRU) (Pollock 1993[23]) and the exercise protocol of (Jull 1999[24])
- Activation of the deep neck muscles aimed to enhance their ability for active stabilization for warm-up (a)
- Flexion and extension of neck using the MCRU as a warm-up exercise for the superficial neck muscles using resistance equal to approximately 20% of the peak isometric muscle strength as warm-up (b)
- Full flexion and extension within pain tolerance (b)
- The dynamic weight load was calculated to be about 30% of the peak isometric muscle strength
- The weight load was increased by approximately 5%, when a set of 12 or more repetitions had been achieved.
- Activation of the deep neck flexor muscles (c)
- the patient lay down in the supine position with the weight of the head and the cervical spine supported by towels under the occiput in a neutral position
- An air-filled pressure sensor (Stablizer, Chattanooga South Pacific, Australia) was used to monitor the subtle flattening of the cervical lordosis that was expected to occur with contraction of deep neck flexors.
- The sensor was placed suboccipitally behind the neck and inflated to 20 mmHg
- The patient was instructed to slowly nod the head in an action indicating 'yes', so as to raise the pressure to a level that could be held steadily for 10 seconds
- A 15 second break was given between each 10 second hold and this pattern was repeated for 10 minutes or until patient was unable to hold the contraction
Bronfort 2001[edit | edit source]
- Stretching for warm-up (d-f)
- Aerobic exercise using dual action stationary bike for warm-up
- Strengthening of shoulders and upper back using MedX variable resistance equipment (g)
- Patients were stabilized with torso restraints to isolate and specifically exercise the cervical musculature.
- They were encouraged to perform repetitions to volitional muscle fatigue (maximum 20 reps) even if pain was exacerbated, and resistance was increased periodically. (Highland et al, 1992 ; Nelson et al, 1999)
Franca 2008[edit | edit source]
Strengthening exercise (Hall and Brody, 1999)
- Stretching exercise of the muscles of the neck and upper limbs regions (d-f, h-l)
- Recruitment exercise of the deep cervical flexion muscles (wave movement of the head) (a)
- Strengthening exercise of the deep cervical flexion muscles (c)
- Strengthening of upper limbs (o-l)
Martel 2011[edit | edit source]
- Advised to perform a home exercise program 3 times/week
- All participants were instructed in the same routine
- Exercise volume was tailored to each participant’s strength, flexibility and ability to complete the routine with minimal neck pain
- Each patient received a written copy of the program and exercises were checked every 2 months by a kinesiologist
- Exercises included
- Range of motion exercises (sss-vvv)
- 4 stretching/mobilisation exercises (d-f)
- 4 strengthening exercises (concentric and isometric contractions) of the cervical and upper thoracic spine (primarily flexion, extension, lateral flexion and rotation of the cervical spine) (xxx-bbbb).
Unspecified/mixed duration neck pain[edit | edit source]
Exercise[edit | edit source]
Manual therapy[edit | edit source]
3.2 Neck pain with cervicogenic headache[edit | edit source]
Acute/subacute neck pain with cervicogenic headache[edit | edit source]
Manual therapy and exercise
Exercise
Manual therapy
Chronic neck pain with cervicogenic headache[edit | edit source]
Manual therapy and exercise
Exercise
Manual therapy
3.3 Whiplash associated disorder[edit | edit source]
Acute/subacute whiplash associated disorder[edit | edit source]
Manual therapy and exercise
Exercise
Manual therapy
Chronic whiplash associated disorder[edit | edit source]
Manual therapy and exercise
3.4 Neck pain with radiculopathy[edit | edit source]
Acute neck pain with radiculopathy
[edit | edit source]
Exercise
Manual therapy
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedCleland 2007 - ↑ Gonzalez-Iglesias J, Fernandez-De-Las-Penas C, Cleland JA, Del Rosario Gutierrez-Vega M. Thoracic spine manipulation for the management of paitents with neck pain: a randomized clinical trial. J Orthop Sports Phys There 2009;39(1):20–7.
- ↑ Bronfort G, Evan R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine 2001;26(7):788-99.
- ↑ Haldeman S, Phillips RB. Spinal manipulative therapy in the management of low back pain. In: Frymoyer JW, Ducker TB, Hadler NM, et al, eds. The Adult Spine: Principles and Practice. New York: Raven Press, 1991:1581-605.
- ↑ Dyrssen T, Svedenkrans M, Paasikivi J. Muskeltraning vid besvar i nacke och skuldror effektiv behandling for att minska smartan. Lakartidningen 1989;86:2116-20.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedHoving 2002 - ↑ Basmajian JV, Nyberg R, eds. Rational Manual Therapies. Baltimore: Williams &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Wilkins; 1993.
- ↑ Cookson JC. Orthopedic manual therapy—an overview. Part II: the spine. Phys Ther 1979;59:259-67.
- ↑ Gross AR, Aker PD, Quartly C. Manual therapy in the treatment of neck pain. Rheum Dis Clin North Am 1996;22:579-98.
- ↑ Van der EL, Lunacek PB, Wagemaker AJ. Manuele Therapie: wervelkolom behandeling [Manual Therapy: Treatment of the Spine]. 2nd ed. Rotterdam: Manuwel; 1993.
- ↑ Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 2002;27(17):1835-43.
- ↑ Maitland GD, Hengeveld E, Banks K, et al. Maitland’s Vertebral Maniplation. 6th ed. London: Butterworth, 2000.
- ↑ Jull GA. The management of cervicogenic headache. Manual Ther 1997;2:182–90.
- ↑ Skargren EI, Carlsson PG, Oberg BE. One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Spine 1998;23(17):1875-84.
- ↑ Ylinen J, Takala EP, Nykanen M, Hakkinen A, Malkia E, Pohjolainen T, et al. Active neck muscle training in the treatment of chronic neck pain in women. JAMA 2003;289(19):2509-16.
- ↑ Allison GT, Nagy BM, Hall T. A randomized clinical trial of manual therapy for cervico-brachial pain syndrome e a pilot study. Manual Therapy 2002;7(2):95-102.
- ↑ Elvey RL, Hall TM (1997). Neural tissue evaluation and treatment. Physical Therapy of the Shoulder. Churchill Livingstone,New York.
- ↑ Brodin H. Cervical pain and mobilization. Manual Medicine 1985;2:18-22.
- ↑ Stoddard A (1959). Manual of osteopathic technique. Hutchinson, London.
- ↑ Karlberg M, Magnusson M, Eva-Maj M, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil 1996;77:874-82.
- ↑ Palmgren PJ, Sandstrom PJ, Lundqvist FJ, Heikkila H. Improvement after chiropractic care in cervicocephalic kinesthetic sensibility and subjective pain intensity in patients with nontraumatic chronic neck pain. J Manipulative Physiol Ther 2006;29:100-6.
- ↑ Chiu T, Huiu-Chan C, and Cheing G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabil 2005;19:850-60.
- ↑ Pollock ML, Graves JE, Bamman MM et al.Frequency and volume of resistance training: Effect on cervical extension strength. Arch Phys Med Rehabil 1993;74:1080-86.
- ↑ Jull GA, Barrett C, Magee R, Ho P. Further clarification of musculoskeletal dysfunction in cervical headache. Cephalalgia 1999;19:179-85.