Oculomotor Nerve
Original Editor - Innocent Abugu
Top Contributors - Innocent Abugu, Uchechukwu Chukwuemeka, Kim Jackson, Vidya Acharya and Joseph Ayotunde Aderonmu
Description[edit | edit source]
The oculomotor nerve is the third cranial nerve (CNIII). It has somatic motor (general somatic efferent) and visceral motor (general visceral efferent-parasympathetic) functions.[2]
Root[edit | edit source]
It originates from the oculomotor nucleus and the Edinger-Westphal nucleus within the midbrain of the brainstem.
Branches[edit | edit source]
Superior branch innervates the superior rectus and the levator palpabrae superioris
Inferior branch innervates the medial rectus, inferior rectus and inferior oblique.
Function[edit | edit source]
Motor[edit | edit source]
The oculomotor nerve is the chief motor nerve to the ocular and extraocular muscles. [2] The oculomotor nerves send somatic motor fibres to all extraocular muscles, except the superior oblique and lateral rectus. The superior branch supplies the superior rectus which elevates the eyeball, and the levator palpabrae superioris which raises the upper eyelid.
The inferior branch innervates the medial rectus which adducts the eyeball, the inferior rectus which depresses the eyeball and the inferior oblique which elevates, abducts and laterally rotates the eyeball. The superior oblique and the lateral rectus are supplied by the trochlear and abducens nerves respectively.
Parasympathetic[edit | edit source]
There are two primary functions of the autonomic parasympathetic (involuntary) oculomotor nerve. It constricts the pupil (miosis) by innervating the smooth muscle (sphincter pupillae) near the pupil. It also innervates the ciliary muscles.[3] The sphincter pupillae causes narrowing of the pupil in order to prevent diverging light rays from the corneal periphery creating a blurred image.[4] The ciliary muscle changes the shape of the lens during accomodation.
Sympathetic[edit | edit source]
The oculomotor nerve has no direct function, but sympathetic fibres run with the oculomotor nerve to innervate the superior tarsal muscle (helps to raise the eyelid).[5]
Clinical relevance[edit | edit source]
Damage to the oculomotor nerve or any of its branches could lead to oculomotor motor nerve palsy (Third nerve palsy). Some of the causes include:
- Vascular ischemia
- Trauma
- Intracranial neoplasm
- Hemorrhage
- Congenital
- Idiopathic[6]
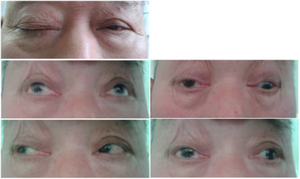
With unilateral third cranial nerve palsy (ie, oculomotor nerve palsy), the involved eye usually is deviated "down and out" (ie, infraducted and abducted), and there may be partial or complete ptosis. In addition, pupillary dilatation can cause anisocoria (greater in the light), symptomatic glare in bright light, and accommodation deficit that may cause blurred vision for near objects.[7] A complete third nerve palsy presents with ipsilateral mydriasis, bilateral ptosis, contralateral elevation deficit, and ipsilateral adduction and depression deficits.[8]
Assessment[edit | edit source]
Draw an ‘H-shape’ with a finger or the tip of a pen and ask the patient to follow your finger (or the pen) with their eyes. The head of the patient should be still during this process and the patient is asked to report any blurring of vision or double vision(diplopia). Total oculomotor nerve palsy implies involvement of all muscles innervated by the oculomotor nerve with pupillary involvement. There will be limitation of movements in all fields of gaze except abduction and intorsion. Incomplete palsy implies either partial limitation (paresis) of elevation, depression or abduction or even full movement in one or more of these directions.[9]
Treatment[edit | edit source]
Treatment initially involves medical management of systemic predisposing factors and conservative measures to obviate symptoms followed later by surgical intervention in nonresolving oculomotor nerve palsy.[9]
Physiotherapy can be an effective treatment of choice after failed pharmacological treatment in patients with damage to cranial nerves III and VI.[11] Physiotherapy management of oculomotor nerve palsy include neuromuscular re-education, kinesiotaping, laser therapy, trigger point therapy and electrostimulation.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 3D4Medical From Elsevier. Anatomy Dissected: Cranial Nerve III (oculomotor nerve). Available from: https://youtu.be/IfEnt4ulzb8
- ↑ 2.0 2.1 Keith LM, Arthur FD, Anne MR. Clinically Oriented Anatomy.
- ↑ Joyce C, Le PH, Peterson DC. Neuroanatomy, Cranial Nerve 3 (Oculomotor). Available from: https://www.ncbi.nlm.nih.gov/books/NBK537126/
- ↑ Bloom J, Motlagh M, Czyz CN. Anatomy, Head and Neck, Eye Iris Sphincter Muscle. Available from:https://www.ncbi.nlm.nih.gov/books/NBK532252/
- ↑ Navin L. The Oculomotor Nerve (CN III). Available from:https://teachmeanatomy.info/head/cranial-nerves/oculomotor/
- ↑ Modi P, Arsiwalla T. Cranial Nerve III Palsy. Available from:https://europepmc.org/article/NBK/nbk526112
- ↑ James G, Andrew GL. Third Nerve Palsy (Oculomotor Nerve Palsy) Treatment & Management. E_Medicine.
- ↑ Grover SK. Revisiting Third Nerve Palsy.DJO [serial online] 2020[cited 2021 Mar 31];31:18-22. Available from: https://www.djo.org.in/articles/31/1/Revisiting-Third-Nerve-Palsy.html
- ↑ 9.0 9.1 Sadagopan KA, Wasserman BN. Managing the patient with oculomotor nerve palsy. Current opinion in ophthalmology. 2013 Sep 1;24(5):438-47.
- ↑ Physiotutors. Cranial Nerves 3, 4, 6 | Oculomotor, Trochlear, Abducens Nerve Assessement for Physiotherapists. Available from: https://youtu.be/wtUBAD--fVI
- ↑ Rongies W, Bojakowski J, Koktysz L, Dolecki W, Lewinska AO, Krzeski A. Physiotherapy in Postinfection Injury to Cranial Nerves III, IV, and VI: A Case Study. American journal of physical medicine & rehabilitation. 2019 Jun 1;98(6):e57-9.