Physical Activity and Injury Prevention in Adolescents
- Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
- If you would like to get involved in this project and earn accreditation for your contributions, please get in touch!
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Charmene Chaudhry, Chelsea Mclene, Zoe Rounding, Ewa Jaraczewska, Kim Jackson, Simisola Ajeyalemi, Kirsten Dippie, Wanda van Niekerk, 127.0.0.1, Rachael Lowe, Michelle Lee, Fergal O'Reilly, Katie Laverty, Leah Boudreau and WikiSysop
Welcome to the Wiki[edit | edit source]
Introduction[edit | edit source]
Regular health benefits of participation in physical activity are well studied (Collard et al 2009). However, physical inactivity remains one of the largest worldwide threats and is the leading preventable cause of morbidity and mortality (NICE 2012). Since 1980, the prevalence of obesity worldwide has more than doubled in children and quadrupled in adolescents (McCormick et al 2007). In 2012, more than a third of children and adolescents were overweight or obese (CDC 2015). Physiotherapists are faced with an ever-growing challenge in efforts to promote physical activity in order for people to live a healthy life.
Physical activity has its drawbacks as well, there are risks of injuries and accidents of participants. Children and adolescents are the largest participants in physical activity and they are at a particular risk for these injuries, because of a high level of exposure, improper technique, poor proprioception, muscle weaknesses, apparatuses not adjusted to their size, absence of fear and understanding of risks (Collard et al 2009; Habelt et al 2011). Physical activity is the leading cause of injury and hospital room visits in adolescents (Brussoni et al 2015). Most injuries or accidents resulting from physical activity are non life threatening however they often result in pain, disability, school absence, absence from physical activity, and sometimes in dysfunction in the short and long term (Collard et al 2009). Injuries to joints can accelerate the development of osteoarthritis. Therefore, prevention of physical activity related injuries are essential. Emery (2005) showed in a review that injury prevention strategies in children could reduce the risk of physical activity related injuries.
Physiotherapists have an extremely important role in the prevention of injuries and accidents as a result of physical activity in adolescents so they can continue to enjoy the physical, social and emotional benefits of activities without compromising their safety. Therefore the aim of this Wiki is critically evaluate the role of the physiotherapist in the prevention of injury and accident as a result of physical activity in adolescents age 12-18.
This is Reflective Ralph. He will accompany you through this Wiki resource, and help guide your learning by posing questions you are encouraged to think about.
Important Information  [edit | edit source]
[edit | edit source]
Aims of the Wiki[edit | edit source]
Learning Outcomes[edit | edit source]
By the end of this resource, the learner will be able:
- To critically evaluate prevention and prevention strategies of injury and accidents in adolescents age 12-18 participating in physical activity in the context of physiotherapy practice.
- To be able to critically evaluate the level of effectiveness of preventative equipment and education in prevention of injuries and accidents in adolescents age 12-18.
- To be able to justify a prehabilitation programme and promote each component in the prevention of injuries and accidents in adolescents age 12-18.
- To be able to critically reflect upon the challenges and be able to make recommendations that can be implemented to prevent injuries and accidents in adolescents age 12-18 during physical activity.
Intended Audience[edit | edit source]
The following resource is designed for students and recently qualified physiotherapists, looking to enhance their continual professional development, in regards to the prevention of injuries and accidents in adolescents age 12-18. This resource however is not to be exclusive to these groups as other individuals interested in this topic area may be able to extract relevant information as well.
Relevant Definitions[edit | edit source]
TABLE
Defining the Question[edit | edit source]
Physical Activity and Health[edit | edit source]
WHO (2016) define physical activity as “any bodily movement produced by skeletal muscles that requires energy expenditure.” This broad definition entails that there are various ways in order to be physically active such as: play, sport, walking, cycling, housework and gardening.
Regular physical activity is known to have many health benefits including:
- Reduce risk of cardiovascular disease
- Reduce risk of type II diabetes
- Reduce risk of certain types of cancers
- Reduce blood pressure
- Improve mental health and wellbeing
- Improve social and moral development
- Improve ability of academic achievements – i.e. ability to concentrate and better classroom discipline
- Contribute to healthy weight maintenance (WHO 2016)
WHO (2016) recommends for children and adolescents to accumulate at least one hour of moderate activity on most days of the week. Three days per week high intensity physical activities should be incorporated. All children and young people should minimise the amount of time being sedentary for extended periods of time.
List three reasons why prevention of injury and accident as a result of physical activity in adolescents is important.
Role of the Physiotherapist[edit | edit source]
The Chartered Society of Physiotherapy (CSP, 2011) define physiotherapy as "a healthcare profession that works with people to identify and maximize their ability to move and function" (p. 4). Physiotherapy helps people of all ages to prevent, manage and rehabilitate injury, illness or disability through education, advice, exercise and manual therapy. It is important to possess the skills required for working within these in demand services.
The Knowledge and Skills Framework – can someone help me with this part.. I don’t get it. She had said to relate to this however I am unsure what to include.
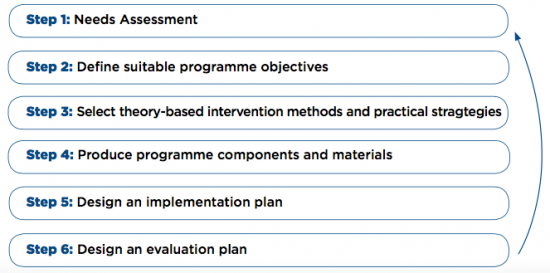
A physiotherapist can develop an injury prevention programme through the use of intervention mapping (IM) protocol. This involves a systematic process that prescribes a series of six steps in order to develop theories and evidence based health promotion programmes (Figure 2) (Collard et al 2009). This six-step process can aid physiotherapists in the development of various prevention programmes such as the prevention of injury and accidents in adolescents age 12-18 as a result of physical activity.
For an example of this IM protocol used, please read the following article available in the References section: Design of iplay study: systematic development of a physical activity injury prevention program for primary school children. (Collard et al 2009)
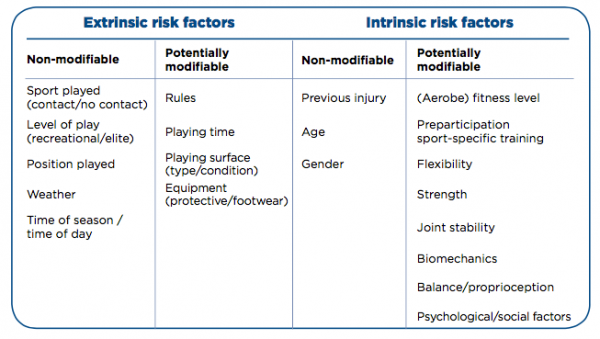
Risk factors are generally the leading guide for preventative measures in physical activity (Collard et al 2009). These risk factors can increase the risk of an injury or accident as a result of physical activity in adolescents age 12-18 and can include both extrinsic and intrinsic factors. Injuries and accidents can also be caused by a combination of these factors. It is important for physiotherapists to identify these risk factors in order to aid in prevention.
Demands on Health Care Services[edit | edit source]
Health benefits of physical activity are extremely important however physical activity also exposes the participant to a risk of injury or accident. Physical activity such as sport and recreation, cycling, skateboarding and playground use is the most common reason for Australian youth aged 0-16 to be in an emergency department and 14% of these presenting injuries require hospitalisation. (Spinks et al 2006). Similar results have been found worldwide in countries such as Norway, France, New Zealand and the United States (Collard et al 2009).
Not only do injuries and accidents related to physical activity affect healthcare services, they also affect school and work time. A study conducted in the Netherlands showed that school absence occurs in 7% of children and adolescents who sustained a sport injury, and the means duration of school missed by these children was 8 days (Collard et al 2009). This means that 0.02% of the total population who visit school and participate in physical activity are absent from school one or more days. With a mean duration of 8 days, the total absence due to sports injuries can be calculated at 794,000 days a year. In addition, 22% of people who sustained an injury were also absent from physical activities. The economic consequences of physical activity-related injuries in adolescents are not known, but direct medical costs were estimated at 170 million euros and indirect costs i.e. school or work absence was estimated at 420 million euros.
These preventable injuries increase the wait time for persons to see a physiotherapist. In the NHS the average wait time to see a physiotherapist in a musculoskeletal outpatient department is approximately six to eight weeks. Therefore if a plan is put in place to prevent these injuries less persons would require rehabilitation from a physiotherapist. Overall, the safety can be improved in many of these activities so that participants are able to continue to enjoy them without their safety being compromised.
What are the main contributing factors that increase strain on health care?
Current Legislation[edit | edit source]
Sport-Specific Laws[edit | edit source]
All sports have their own legislations when it comes to protective equipment, but there are not specific laws for types of physical activity. In this section we will provide links to the laws for a number of sports and types of physical activities and discuss the role of the physiotherapist in enforcing them and ways in which to do so.
Here is a list of a selection of popular sports and activities with links to their laws which include those on protective equipment:
- Football
- Rugby Union
- Rugby League
- Horse-riding
- Hockey
- Boxing: Technical rules, Open boxing competition rules, World series competition rules
Controversial Issues[edit | edit source]
There is more of a debate around cycling and boxing and helmet use so here we will highlight the controversial issues.
Cycling[edit | edit source]
Cycling, classified as both a sport and type of physical activity, is increasing in popularity in the UK as a means of exercise but also of transport. 40% of paediatric hospitalisations and deaths are due to head injury following a bicycle-related trauma (Macpherson and Spinks 2009) Despite this it is currently not required by law to wear a helmet in the majority of the UK (Transport Planning Society 2012), although there have been many calls by different bodies to make helmet wearing compulsory. It is however stated in the Highway Code (Rule 59) that cyclists should wear a helmet which conforms to the current regulations, is the correct size and is securely fastened.
The arguments of cycling advocates against having a mandatory cycle helmet law are that there will be a dramatic decline in the number of people cycling and that will lead to an increase in premature deaths and have a greater impact on the populations’ health than the risks of head injuries from not wearing a helmet. Cycling UK (2016) reports that 7-8% of head injuries in children admitted to English hospitals are due to cycling with a small number of these being to areas of the head that a helmet may protect, but isn’t encouraging anything that could save the lives of our children, or reduce the risk of injury worthwhile when they are the generation that will be looking after us and have the majority of their lives ahead of them?
It has been highlighted by Macpherson and Spinks (2009) that the following are the reasons people choose not use helmets and therefore could cause the supposed decline in number of people cycling if a law was put into place:
- The cost of purchasing one
- The discomfort of wearing one
- The lack in the belief that is necessary
- The unpopular image of helmets, e.g. children not looking ‘cool’ in front of their friends
In 1999 the British Medical Association (BMA) believed in the potential drop in number of cyclists and recommended there be no law on bicycle helmets but still recommended the use of helmets, however in 2004 the BMA changed their position and became in favour of mandatory cycle helmets. This change in stance came about because of their beliefs into the protective effects of cycle helmets in reducing the number and severity of head injuries.
Whilst it is not a legal requirement in the majority of the UK to wear a helmet, Jersey has made it compulsory for children under 13 to wear cycle helmets. You can read about that here. More than 20 countries around the world have made the wearing of cycle helmets compulsory including Finland, Sweden, Australia and some US states and Canadian provinces (Macpherson and Spinks 2009; Gleave 2012). This is section we will explore the impacts of these laws on cycling rates and injuries in some of these countries.
A study in Canada (Macpherson et al. 2002) focussed on cycling related injuries of children admitted to hospital during 1994 and 1998. The rate of head injuries suffered by children when cycling had a significantly greater decline in provinces where legislation regarding a compulsory cycle helmet was adopted when compared to provinces where such legislation was not adopted. This trend was also found in New South Wales, Australia by Walter et al. (2011) where there was a large reduction the rate of head injuries among cyclists following the implementation of legislation. Macpherson et al. (2002) discovered there was also a decline in the rate of other types of injuries however this finding was not statistically significant. Macpherson and Spinks (2009) found the risk of a cyclist suffering a head or facial injury was reduced by 88% and 65% respectively if they were wearing a helmet. A systematic review looking into injuries and use of helmets found there to be reductions in the risk of suffering head injuries (51%), serious head injuries (69%), fatal head injuries (65%) and facial injuries (33%) (Olivier and Creighton 2009).
The introduction of mandatory cycle helmets in Ontario in 1995 (Macpherson et al. 2001) does not appear to have an impact on the cycling participation of children in the East York area of Ontario. Changes were noticed in the pattern of cycling but these were related to the location of where children were cycling and factors including weather. This study shows that introducing legislation that makes cycle helmets mandatory does not have a negative impact on the number of children cycling (Macpherson et al. 2001). In a Cochrane Review Macpherson and Spinks (2009) highlighted that there was not enough evidence to prove or disprove the argument that introducing cycle helmet legislation causes a decline in the cycling population. They did however find that the introduction of legislations increased helmet use and reduced the number of head injuries related to bicycle use.
Many of you may have heard of the story of James Cracknell, the Olympic gold medal winning rower, who suffered a traumatic brain injury whilst cycling in the United States of America. He was wearing a helmet and highlights that his injuries would have been worse, if not fatal, if he was not wearing one:
Physiotherapists, alongside the BMA, have a role in educating the population that while helmets are not mandatory, they do have protective effects against head and facial injuries. While there is currently no law advocating the compulsory use of helmets, physiotherapists can address the reasons people choose to not wear them; this could be undertaken during one-on-one time with patients and combatting these barriers with patients could lead to an increase in those using helmets. With the age group we are focussing on it could prove beneficial to encourage the use of helmets from an early age so it becomes habit for them throughout their life. As physiotherapists we can also take our own advice on board and wear helmets routinely so that the general population see them being used and this becomes the norm.
Boxing[edit | edit source]
Prior to the Summer Olympics (2016) the law permitting amateur boxers to wear protective head gear during a fight was changed. Male boxers were no longer permitted to wear protective however it was still mandatory for female boxers to wear them. Headguards are not allowed during elite male (19+ years) competitions however they are still mandatory within all other categories but the International Boxing Association (AIBA) are able to withdraw the use of headguards during non-elite competitions; this is in preparation for the removal of headguards in all competitions from January 2018 (AIBA 2015a).
What Can We Do?[edit | edit source]
In sports such as rugby union and football there are recognised concussion protocols (e.g. ‘If in doubt, sit them out’) which you can read about here (World Rugy- Concussion Management) and here (Football Association- What is Concussion). Although these protocols are not considered protective equipment there is a question to be asked: is it ok that in these sports we are trying to recognise concussion and reduce the risks to people of having secondary concussions whilst in other types of physical activity such as boxing and cycling they are trying to justify not wearing protective equipment for the head?
An overview of how laws are made is provided by this article here. In the section titled ‘Interested people and groups are consulted’ it explains that those who may be effected by the proposed new law can be met by a minister and it can be discussed. For a law to be passed on making cycle helmets mandatory allied health professionals (AHPs) should be consulted due to them having to deal with aftermath so to speak. AHPs should have a place at the table when discussing laws that have an impact on the health care service and on the wellbeing of the general public. Physiotherapists have a major role in the rehabilitation of cycling injuries from fractures to those requiring surgery; and make up a multi-disciplinary team with occupational therapists and speech and language therapists to work closely with those who have suffered traumatic brain injuries.
Another way physiotherapists can have a role in the wearing of protective equipment is to utilise the time spent with patients during assessments and treatment sessions. Physiotherapists have the advantage of having a longer duration of contact time with people than most other professionals. Physiotherapists can incorporate questioning about whether their patients utilise protective equipment during their subjective assessments and provide education to people during their rehabilitation. This does not necessarily need to be following an injury, however this could be an opportunity to reinforce the need for equipment, but also if the public visit a physiotherapist for advice on how to change their behaviours to gain a healthier lifestyle.
Types of Preventative and Protective Equipment[edit | edit source]
Individual Sports[edit | edit source]
Evidence and Efficacy Studies of Preventative Equipment[edit | edit source]
Physiotherapist Advice[edit | edit source]
Prehabilitation[edit | edit source]
Warm Up[edit | edit source]
S&C[edit | edit source]
SAQ[edit | edit source]
Pre season Testing[edit | edit source]
Cool down/stretches[edit | edit source]
Past injuries
[edit | edit source]
Education[edit | edit source]
Hydration[edit | edit source]
Nutrition
[edit | edit source]
Skill acquisition
[edit | edit source]
Posture
[edit | edit source]
Conditions/environment
[edit | edit source]
Rest
[edit | edit source]
Gradual progress
[edit | edit source]
Respect pain[edit | edit source]
Scenarios[edit | edit source]
Case Studies[edit | edit source]
Conclusion and Summary[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.