Physical Activity and Injury Prevention in Adolescents
- Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
- If you would like to get involved in this project and earn accreditation for your contributions, please get in touch!
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Charmene Chaudhry, Zoe Rounding, Chelsea Mclene, Kim Jackson, Ewa Jaraczewska, Simisola Ajeyalemi, Kirsten Dippie, Wanda van Niekerk, 127.0.0.1, Rachael Lowe, Katie Laverty, Leah Boudreau, Michelle Lee, Fergal O'Reilly and WikiSysop
Welcome to the Wiki[edit | edit source]
Introduction[edit | edit source]
Regular health benefits of participation in physical activity are well studied[1]. However, physical inactivity remains one of the largest worldwide threats and is the leading preventable cause of morbidity and mortality[2]. Since 1980, the prevalence of obesity worldwide has more than doubled in children and quadrupled in adolescents[3]. In 2012, more than a third of children and adolescents were overweight or obese[4]. Physiotherapists are faced with an ever-growing challenge in efforts to promote physical activity in order for people to live a healthy life.
Physical activity has its drawbacks as well, there are risks of injuries and accidents of participants. Children and adolescents are the largest participants in physical activity and they are at a particular risk for these injuries, because of a high level of exposure, improper technique, poor proprioception, muscle weaknesses, apparatuses not adjusted to their size, absence of fear and understanding of risks[5][6]. Physical activity is the leading cause of injury and hospital room visits in adolescents[7]. Most injuries or accidents resulting from physical activity are non life threatening however they often result in pain, disability, school absence, absence from physical activity, and sometimes in dysfunction in the short and long term[5]. Injuries to joints can accelerate the development of osteoarthritis. Therefore, prevention of physical activity related injuries are essential. Emery[8] showed in a review that injury prevention strategies in children could reduce the risk of physical activity related injuries.
Physiotherapists have an extremely important role in the prevention of injuries and accidents as a result of physical activity in adolescents so they can continue to enjoy the physical, social and emotional benefits of activities without compromising their safety. Therefore the aim of this Wiki is critically evaluate the role of the physiotherapist in the prevention of injury and accident as a result of physical activity in adolescents age 12-18.
This is Reflective Ralph. He will accompany you through this Wiki resource, and help guide your learning by posing questions you are encouraged to think about.
Important Information  [edit | edit source]
[edit | edit source]
Aims of the Wiki[edit | edit source]
Learning Outcomes[edit | edit source]
By the end of this resource, the learner will be able:
- To critically evaluate prevention and prevention strategies of injury and accidents in adolescents age 12-18 participating in physical activity in the context of physiotherapy practice.
- To be able to critically evaluate the level of effectiveness of preventative equipment and education in prevention of injuries and accidents in adolescents age 12-18.
- To be able to justify a prehabilitation programme and promote each component in the prevention of injuries and accidents in adolescents age 12-18.
- To be able to critically reflect upon the challenges and be able to make recommendations that can be implemented to prevent injuries and accidents in adolescents age 12-18 during physical activity.
Intended Audience[edit | edit source]
The following resource is designed for students and recently qualified physiotherapists, looking to enhance their continual professional development, in regards to the prevention of injuries and accidents in adolescents age 12-18. This resource however is not to be exclusive to these groups as other individuals interested in this topic area may be able to extract relevant information as well.
Relevant Definitions[edit | edit source]
Table 1: Definitions of Relevant Terms
Defining the Question[edit | edit source]
Physical Activity and Health[edit | edit source]
The WHO (2016) define physical activity as “any bodily movement produced by skeletal muscles that requires energy expenditure.” This broad definition entails that there are various ways in order to be physically active such as: play, sport, walking, cycling, housework and gardening.
Regular physical activity is known to have many health benefits including:
- Reduce risk of cardiovascular disease
- Reduce risk of type II diabetes
- Reduce risk of certain types of cancers
- Reduce blood pressure
- Improve mental health and wellbeing
- Improve social and moral development
- Improve ability of academic achievements – i.e. ability to concentrate and better classroom discipline
- Contribute to healthy weight maintenance (WHO 2016)
WHO (2016) recommends for children and adolescents to accumulate at least one hour of moderate activity on most days of the week. Three days per week high intensity physical activities should be incorporated. All children and young people should minimise the amount of time being sedentary for extended periods of time.
List three reasons why prevention of injury and accident as a result of physical activity in adolescents is important.
Role of the Physiotherapist[edit | edit source]
The Chartered Society of Physiotherapy (CSP, 2011) define physiotherapy as "a healthcare profession that works with people to identify and maximize their ability to move and function" (p. 4). Physiotherapy helps people of all ages to prevent, manage and rehabilitate injury, illness or disability through education, advice, exercise and manual therapy. It is important to possess the skills required for working within these in demand services.
The Knowledge and Skills Framework – can someone help me with this part.. I don’t get it. She had said to relate to this however I am unsure what to include.
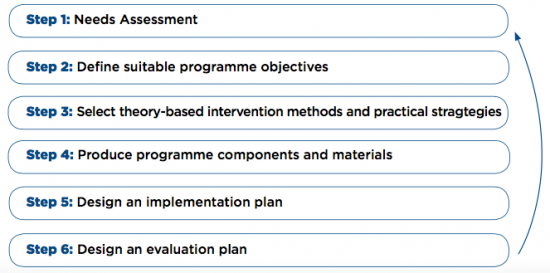
A physiotherapist can develop an injury prevention programme through the use of intervention mapping (IM) protocol. This involves a systematic process that prescribes a series of six steps in order to develop theories and evidence based health promotion programmes (Collard et al 2009). This six-step process can aid physiotherapists in the development of various prevention programmes such as the prevention of injury and accidents in adolescents age 12-18 as a result of physical activity.
For an example of this IM protocol used, please read the following article available in the References section: Design of iplay study: systematic development of a physical activity injury prevention program for primary school children. (Collard et al 2009)
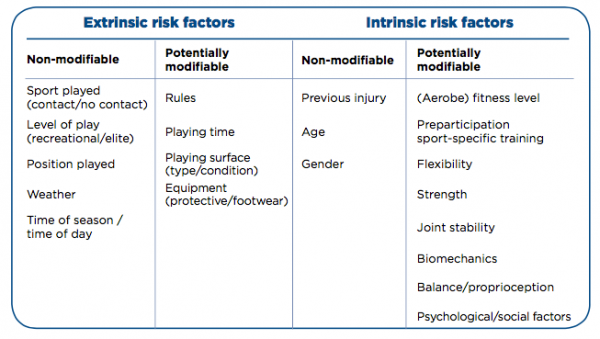
Risk factors are generally the leading guide for preventative measures in physical activity (Collard et al 2009). These risk factors can increase the risk of an injury or accident as a result of physical activity in adolescents age 12-18 and can include both extrinsic and intrinsic factors. Injuries and accidents can also be caused by a combination of these factors. It is important for physiotherapists to identify these risk factors in order to aid in prevention.
Demands on Health Care Services[edit | edit source]
Health benefits of physical activity are extremely important however physical activity also exposes the participant to a risk of injury or accident. Physical activity such as sport and recreation, cycling, skateboarding and playground use is the most common reason for Australian youth aged 0-16 to be in an emergency department and 14% of these presenting injuries require hospitalisation. (Spinks et al 2006). Similar results have been found worldwide in countries such as Norway, France, New Zealand and the United States (Collard et al 2009).
Not only do injuries and accidents related to physical activity affect healthcare services, they also affect school and work time. A study conducted in the Netherlands showed that school absence occurs in 7% of children and adolescents who sustained a sport injury, and the means duration of school missed by these children was 8 days (Collard et al 2009). This means that 0.02% of the total population who visit school and participate in physical activity are absent from school one or more days. With a mean duration of 8 days, the total absence due to sports injuries can be calculated at 794,000 days a year. In addition, 22% of people who sustained an injury were also absent from physical activities. The economic consequences of physical activity-related injuries in adolescents are not known, but direct medical costs were estimated at 170 million euros and indirect costs i.e. school or work absence was estimated at 420 million euros.
These preventable injuries increase the wait time for persons to see a physiotherapist. In the NHS the average wait time to see a physiotherapist in a musculoskeletal outpatient department is approximately six to eight weeks. Therefore if a plan is put in place to prevent these injuries less persons would require rehabilitation from a physiotherapist. Overall, the safety can be improved in many of these activities so that participants are able to continue to enjoy them without their safety being compromised.
What are the main contributing factors that increase strain on health care?
Current Legislation[edit | edit source]
Sport-Specific Laws[edit | edit source]
All sports have their own legislations when it comes to protective equipment, but there are not specific laws for types of physical activity. In this section we will provide links to the laws for a number of sports and types of physical activities and discuss the role of the physiotherapist in enforcing them and ways in which to do so.
Here is a list of a selection of popular sports and activities with links to their laws which include those on protective equipment:
- Football
- Rugby Union
- Rugby League
- Horse-riding
- Hockey
- Boxing: Technical rules, Open boxing competition rules, World series competition rules
Controversial Issues[edit | edit source]
There is more of a debate around cycling and boxing and helmet use so here we will highlight the controversial issues.
Cycling[edit | edit source]
Cycling, classified as both a sport and type of physical activity, is increasing in popularity in the UK as a means of exercise but also of transport. 40% of paediatric hospitalisations and deaths are due to head injury following a bicycle-related trauma (Macpherson and Spinks 2009) Despite this it is currently not required by law to wear a helmet in the majority of the UK (Transport Planning Society 2012), although there have been many calls by different bodies to make helmet wearing compulsory. It is however stated in the Highway Code (Rule 59) that cyclists should wear a helmet which conforms to the current regulations, is the correct size and is securely fastened.
The arguments of cycling advocates against having a mandatory cycle helmet law are that there will be a dramatic decline in the number of people cycling and that will lead to an increase in premature deaths and have a greater impact on the populations’ health than the risks of head injuries from not wearing a helmet. Cycling UK (2016) reports that 7-8% of head injuries in children admitted to English hospitals are due to cycling with a small number of these being to areas of the head that a helmet may protect, but isn’t encouraging anything that could save the lives of our children, or reduce the risk of injury worthwhile when they are the generation that will be looking after us and have the majority of their lives ahead of them?
It has been highlighted by Macpherson and Spinks (2009) that the following are the reasons people choose not use helmets and therefore could cause the supposed decline in number of people cycling if a law was put into place:
- The cost of purchasing one
- The discomfort of wearing one
- The lack in the belief that is necessary
- The unpopular image of helmets, e.g. children not looking ‘cool’ in front of their friends
In 1999 the British Medical Association (BMA) believed in the potential drop in number of cyclists and recommended there be no law on bicycle helmets but still recommended the use of helmets, however in 2004 the BMA changed their position and became in favour of mandatory cycle helmets. This change in stance came about because of their beliefs into the protective effects of cycle helmets in reducing the number and severity of head injuries.
Whilst it is not a legal requirement in the majority of the UK to wear a helmet, Jersey has made it compulsory for children under 13 to wear cycle helmets. You can read about that here. More than 20 countries around the world have made the wearing of cycle helmets compulsory including Finland, Sweden, Australia and some US states and Canadian provinces (Macpherson and Spinks 2009; Gleave 2012). This is section we will explore the impacts of these laws on cycling rates and injuries in some of these countries.
A study in Canada (Macpherson et al. 2002) focussed on cycling related injuries of children admitted to hospital during 1994 and 1998. The rate of head injuries suffered by children when cycling had a significantly greater decline in provinces where legislation regarding a compulsory cycle helmet was adopted when compared to provinces where such legislation was not adopted. This trend was also found in New South Wales, Australia by Walter et al. (2011) where there was a large reduction the rate of head injuries among cyclists following the implementation of legislation. Macpherson et al. (2002) discovered there was also a decline in the rate of other types of injuries however this finding was not statistically significant. Macpherson and Spinks (2009) found the risk of a cyclist suffering a head or facial injury was reduced by 88% and 65% respectively if they were wearing a helmet. A systematic review looking into injuries and use of helmets found there to be reductions in the risk of suffering head injuries (51%), serious head injuries (69%), fatal head injuries (65%) and facial injuries (33%) (Olivier and Creighton 2009).
The introduction of mandatory cycle helmets in Ontario in 1995 (Macpherson et al. 2001) does not appear to have an impact on the cycling participation of children in the East York area of Ontario. Changes were noticed in the pattern of cycling but these were related to the location of where children were cycling and factors including weather. This study shows that introducing legislation that makes cycle helmets mandatory does not have a negative impact on the number of children cycling (Macpherson et al. 2001). In a Cochrane Review Macpherson and Spinks (2009) highlighted that there was not enough evidence to prove or disprove the argument that introducing cycle helmet legislation causes a decline in the cycling population. They did however find that the introduction of legislations increased helmet use and reduced the number of head injuries related to bicycle use.
Many of you may have heard of the story of James Cracknell, the Olympic gold medal winning rower, who suffered a traumatic brain injury whilst cycling in the United States of America. He was wearing a helmet and highlights that his injuries would have been worse, if not fatal, if he was not wearing one:
Physiotherapists, alongside the BMA, have a role in educating the population that while helmets are not mandatory, they do have protective effects against head and facial injuries. While there is currently no law advocating the compulsory use of helmets, physiotherapists can address the reasons people choose to not wear them; this could be undertaken during one-on-one time with patients and combatting these barriers with patients could lead to an increase in those using helmets. With the age group we are focussing on it could prove beneficial to encourage the use of helmets from an early age so it becomes habit for them throughout their life. As physiotherapists we can also take our own advice on board and wear helmets routinely so that the general population see them being used and this becomes the norm.
Boxing[edit | edit source]
Prior to the Summer Olympics (2016) the law permitting amateur boxers to wear protective head gear during a fight was changed. Male boxers were no longer permitted to wear protective however it was still mandatory for female boxers to wear them. Headguards are not allowed during elite male (19+ years) competitions however they are still mandatory within all other categories but the International Boxing Association (AIBA) are able to withdraw the use of headguards during non-elite competitions; this is in preparation for the removal of headguards in all competitions from January 2018 (AIBA 2015a).
What Can We Do?[edit | edit source]
In sports such as rugby union and football there are recognised concussion protocols (e.g. ‘If in doubt, sit them out’) which you can read about here (World Rugy- Concussion Management) and here (Football Association- What is Concussion). Although these protocols are not considered protective equipment there is a question to be asked: is it ok that in these sports we are trying to recognise concussion and reduce the risks to people of having secondary concussions whilst in other types of physical activity such as boxing and cycling they are trying to justify not wearing protective equipment for the head?
An overview of how laws are made is provided by this article here. In the section titled ‘Interested people and groups are consulted’ it explains that those who may be effected by the proposed new law can be met by a minister and it can be discussed. For a law to be passed on making cycle helmets mandatory allied health professionals (AHPs) should be consulted due to them having to deal with aftermath so to speak. AHPs should have a place at the table when discussing laws that have an impact on the health care service and on the wellbeing of the general public. Physiotherapists have a major role in the rehabilitation of cycling injuries from fractures to those requiring surgery; and make up a multi-disciplinary team with occupational therapists and speech and language therapists to work closely with those who have suffered traumatic brain injuries.
Another way physiotherapists can have a role in the wearing of protective equipment is to utilise the time spent with patients during assessments and treatment sessions. Physiotherapists have the advantage of having a longer duration of contact time with people than most other professionals. Physiotherapists can incorporate questioning about whether their patients utilise protective equipment during their subjective assessments and provide education to people during their rehabilitation. This does not necessarily need to be following an injury, however this could be an opportunity to reinforce the need for equipment, but also if the public visit a physiotherapist for advice on how to change their behaviours to gain a healthier lifestyle.
Types of Preventative and Protective Equipment[edit | edit source]
Injuries are a common factor among sports people and physical activity which means protective/preventative equipment may be necessary to reduce the risk of injury. As the diverse and vast nature of today’s sporting activities, it has led to the development of many different sports protective equipment for each specific sport depending on the risk of injury associated respectively.
Among the ages 12-18 there are extra risks associated with taking part in sport, as the body is still growing there is more concern for safety in sport and also among active adolescents who are often involved in more than one sport and age groups meaning they can be quite involved weekly in physical activity of which they must wear protective equipment at all times in dangerous sports to be adequately protected from serious harm (Merkel 2012).
Quiz: Introduction to Protective Equipment[edit | edit source]
Click this link to take an introductory quiz to see what you know about protective equipment.
A Review of Evidence for Prevention[edit | edit source]
Click this link to read a review of evidence for prevention of sports injuries from the UK focal point for violence and injury prevention.
Dangerous Sports and Protective Equipment [edit | edit source]
Below are a few short videos illustrating some of the issues and dangers involved in contact sports.
Hurling vs Ice Hockey: Dangerous sports where protective/preventative equipment is helpful in reducing injuries
The National Football League's concussion crisis
Common Types of Sports Equipment Used in the United Kingdom[edit | edit source]
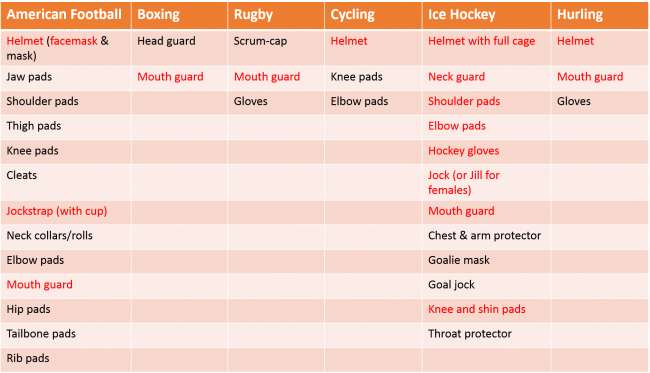
Table 2: Common Types of Sports Preventative Equipment
***Items in red are mandatory for younger adults***
You can click here to read about mandatory and recommended equipment for ice hockey by the International Ice Hockey Federation's Inline Official Rulebook 2015-2018.
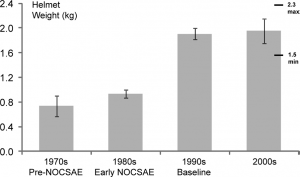
Helmets and Faceguards[edit | edit source]
Helmets are often mandatory or highly advised in a number of sports to reduce the risk of injury from a blow to the head (e.g. American Football, Ice Hockey, Cycling). Faceguards are frequently included in many ball games such as hurling or base ball to prevent facial injuries. In cycling specifically, it has been shown that wearing a helmet can reduce the risk of severe injury from an associated blow to the head by approximately 63-88%. Research is less extensive on the use and impact of helmets in other sports but there are many benefits in association with the wearing of helmets in sports such as ice hockey and rugby. And in other sports such as cricket, in Australia the compulsory wearing of helmets in younger players reduced facial, neck and head injuries from 35% to 4% with its introduction (Thompson 2000).
Knee Braces[edit | edit source]
Knee braces are a specifically designed support made from elastic, foam or plastic which provide assistance to the knee joint during motion and also provide protection against direct blows. They are used throughout the world but their ability is unclear in terms of preventing injuries. Although this may be the case, there is also evidence to show its protective properties to reducing the risk of ligament sprain and giving a larger resistance to blows to the knee (Thacker 2003).
Ankle Braces and Taping[edit | edit source]
Ankle braces fundamentally provide a carbon copy to that of the knee brace with a focus on the ankle which help to reduce range of motion of the ankle. Traditional taping may also be used in sport which also help to limit ankle movement to prevent injury. Ankle ligament sprains are the main preventative area these braces/taping methods aid especially in those who have a history or predisposition to ankle sprains. Evidence suggests braces or taping can reduce ankle sprain by 69% to 71% amongst athletes with previous ankle injuries (Handoll 2001).
Mouth Guards[edit | edit source]
Mouth guards or also called gum shields are used mainly in contact sports where they act as shock absorber and separate the lower and upper teeth as well as teeth from its surrounding tissue. The specific shock absorbing characteristics of this sports protective equipment reduces the force transferred to teeth which therefore helps to prevent orofacial or dental injuries which can be caused by blows to the head in sports such as boxing, rugby and ice hockey (Knapik 2007).
Epidemiology/Statistics of Injury[edit | edit source]
Quiz: Statistics of Sports Injury[edit | edit source]
Click this link to take an prepatory quiz to see what you know about the statistics of sports injuries.
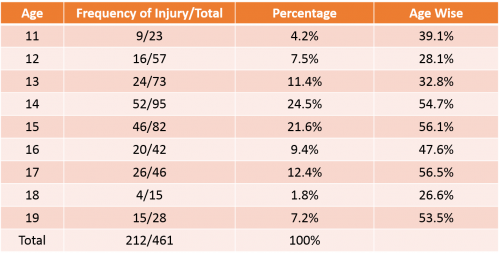
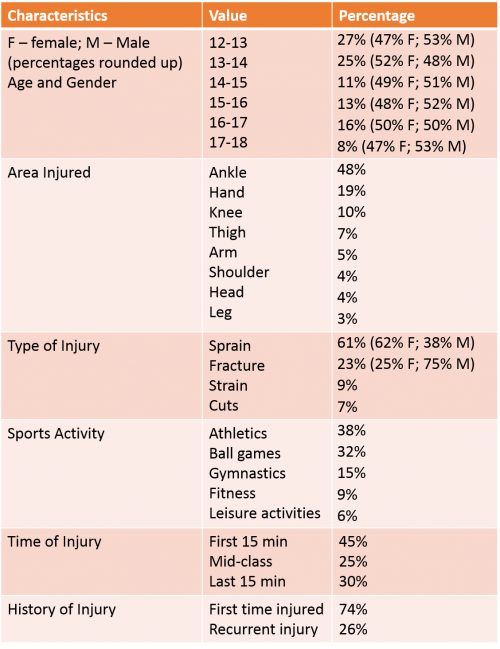
Table 3: Prevalence of Injury in Schoolchildren Among Physical Education Class
Adapted from Sreekaarini (2014)
Table 4: Characteristics of Sports Injuries in Students (n=192)
Adapted from Carmeli (2003)
Potential Mechanisms of Injury in Sport[edit | edit source]
- Lack of Protection: A lack of protection in contact/high velocity sports in particular may cause injury so protective equipment is necessary to reduce risk of injury and reduce the impact of the level of force exerted on the individual.
- Field/Facilities: The terrain/ground may lead to a reduce in grip such as that in ice hockey. Slippery/uneven surfaces can lead to a harder fall during contact.
- Inappropriate Footwear: Inappropriate footwear may lead to reduced protection and control of the ankle and foot.
- Physical Games: Serious injury may result from contact such as a direct blow or as a resultant from falling to the ground.
- Lack of Knowledge/Facilities Surrounding Appropriate Equipment Use: If particular sports protective equipment, such as a helmet, is not worn correctly/snugly in place it can lead to a reduction in its effectiveness in reducing serious injury.
- Rules/Regulatory Bodies: In sports such as ice hockey, there is player contact where one player fends another off the play which can result in serious harm to the individual involved.
- Age: If an individual is much younger than a fellow player it can have a massive influence in the development of injuries for contact sports in particular. A person playing at a young age is also more vulnerable as their bones are still growing until the age of adulthood.
Issues in Specific Sports[edit | edit source]
Hurling[edit | edit source]
Hurling (or Camogie) is an Irish national sport where two teams consisting of 15 players each use a 1-m long ash stick (hurley) to strike a hard leather ball (sliotar). It is one of the fastest field sports and due to the nature and rules of the game such as swinging of the hurley and the weight of the sliotar, as one can imagine the likelihood of injury is very high. In previous years helmets were not regularly worn or mandatory. More recently, this changed and helmets have greatly reduced common head injuries.
The proportion of hurling-related head injuries among A&E treated players are reduced 10-fold when full head protection is available by wearing both a helmet and faceguard.
Evidence was discovered of iatrogenic-like consequences in terms of hand injuries when full head protective equipment was used (Crowley 2014; O'Connor 2016).
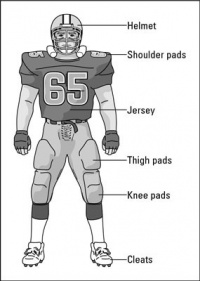
American Football[edit | edit source]
American Football is arguably one of the most dangerous sports where players of different weights, sizes, speeds and strengths depending on their position face off to tackle the player on the opposition. Because of this, protection is vital especially for smaller players or ones who are playing in positions such as quarter back where more skill and precision is needed over size. In 12-18 year olds there can be huge discrepancies in builds, weights and sizes within this population when playing against their counterparts and this therefore means a vast array of protection must be worn to prevent serious harm.
Helmet/face mask:
Due to the unforgiving, aggressive nature of American football it is necessary to wear a helmet to prevent a serious head injury. Along with this, players may decide to wear a mouth guard and other added protection to further equip themselves for protection such as:
- Chin straps: This allows the helmet to be secured correctly allowing a snug fit.
- Air-filled interior pockets: This design of air-filled pockets works as a preventative measure against serious concussions which are of regular occurrence in the game.
- Face masks: Face masks can also comprise of a bar which comes down past the nose area and joins 2 or 3 bars from both sides which as its name ‘cage’ suggests it precludes an opponent reaching into the facial area with their hand.
Pads:
There are many different pads which can be used to absorb blows from another player due to contact such as shoulder pads, thigh pads, elbow pads, hip pads, tail pads and knee pads. Shoulder pads as the name suggests protect the individual’s shoulder but also give protection to the sternum region where some may also provide shield to the rotator cuff and top of the arm.
Football boots/cleats can come with studs of varying sixes from ½ inch to 1 inch. The reason behind this is the traction to the ground where the field may differ in its surface from hard to soft ground and with proper selectivity of cleats it therefore prevents injury from falls to the ground.
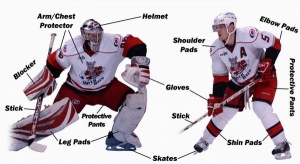
Ice Hockey[edit | edit source]
Ice hockey is a game played in many parts of the world and is a highly contact team sport where two teams use their individual stick to hit a puck into the other’s net. As well as it being a contact sport it is a high-speed game (~20-30mph) where injuries are quite common so protective equipment is of high importance to prevent serious injury. A lot of the game focuses on physicality among players and other influences such as hockey pucks, skate blades and hockey sticks all have an impact in causing serious harm to an individual. Injuries that occur usually include: concussions, muscle strains, broken bones, contusions, hyperextensions and ligament tears (Council on Sports Medicine and Fitness 2014).
According to Rule 1026 regarding mandatory equipment of the Hockey IIHF Rule Book 2015-2018: For players 18 years of age and younger, mandatory equipment includes helmet, full facemask, elbow pads, gloves, internal mouth guard, and knee and shin protection. You can read this and other mandatory and suggested equipment information in the IIHF Rule Book 2015-2018 by clicking this link here. Below are two videos illustrating how to put on protective hockey gear and how ice hockey equipment protects you.
Role of Physiotherapists for this Population[edit | edit source]
Protective equipment in general is on the rise as it is of vital importance for individuals involved in sport and physical activity but it is even more crucially important for younger adults who are still developing as an injury such as a fall where you hit your head may cause even more damage to a 12 year old than a 20 year old.
The reason younger age individuals are required to wear more equipment than their adult counterparts is the facts that will be mentioned below such that they are still growing and their bones are still developing which also means they are more susceptible to injuries as a result (Merkel 2012).
Injuries Which May Occur:
[edit | edit source]
- Overuse injuries
- Strains
- Contusions
- Dislocations (shoulder)
- Physeal plate injuries
Areas Commonly Affected:[edit | edit source]
- Extensor mechanism of the knee from increased stresses when running, jumping and squatting.
- Achilles tendon
- Muscles: mainly of Lower limb
- Shoulder (labrum-ligament complex)
- Physis
Long-Term Effects on Adolescents:[edit | edit source]
- Can affect normal physical growth and maturation
- Osgood-Schlatter disease- traction apophysitis of the tibial tubercle
- Sinding-Larsen-Johansson- occurs at distal pole of patella
- Myositis ossificans
- Instability of the shoulder, Bankart lesion
- Physeal plates-causing deformities by affecting normal growth (Merkel 2012)
Causes:[edit | edit source]
- Excessive stresses
- Forceful contraction of muscle
- Improper warm-up before sports, fatigue, previous injury
- Physical contact, falls
- Acute mechanical overload
Possible Role/Treatment of Physiotherapists:[edit | edit source]
- To manage injury and educate to prevent overtraining and exposure to excessive levels of physical activity.
- Rest, ice, hamstring stretching, quadriceps strengthening, patellar tendon taping
- Achilles and plantar fascia stretching, or cast immobilisation in extreme cases
- To try and educate teams and individuals of importance of warm-up and stretch before sporting activities
- Early initial immobilization of muscle under considerable stretch to reduce oedema and accumulation of scar tissue and earlier recovery of strength
- Preventative/protective equipment such as helmets, pads, etc.
- Overuse injuries: From repetitive application of submaximal stresses to otherwise normal tissue. This is common among organised sports such as American Football, compared with recreational/backyard games. Overtraining and exposure to excessive levels of physical activity can present an increased risk of injury. If not managed properly and efficiently, overuse injuries can affect normal physical growth and maturation. Prevention is key, gradual rather than sudden increases and intensity can usually avoid physical breakdown.
- Strains: occur to the muscle due to forceful contraction of the specific area. Strains are commonly arranged among severity making up of 3 degrees of strains with the third being a complete tear of the musculotendinous junction.
- Contusions: most commonly occur from contact sports such as previously mentioned ice hockey or hurling.
- Dislocations: Dislocations wouldn’t be considered very common among younger athletes but of these ones affecting the shoulder are the most incapacitating injury as in a younger individual it can lead to a Bankart lesion (90%) resulting in long-term disability and instability among the labrum-ligament complex.
- Physeal plate injuries: The most vulnerable part of a younger, immature athlete is that of the physis where physeal plate injuries can have devastating effects on growth. Physeal plate injuries/fractures are often caused by acute mechanical overload often associated with collision/contact sports such as American Football or rugby. (Merkel 2012)
Considerations of Preventative Equipment[edit | edit source]
There are some criticisms of using certain protective equipment in sports. Why would people be against wearing protection to prevent injury? Below are some arguments against the use of protective equipment in sport.
- Players: not used to it, may slow them down or affect vision/performance
- Regulatory bodies possibly lenient and not wanting change in the sport which may have been played somewhat successfully for a number of years.
- In skiing it has been demonstrated that although helmets provide protection, by wearing them they may also increase the risk of concussion from impact.
Childrens' Participation in Dangerous Contact Sports[edit | edit source]
Experts seek ban on tackling in school rugby to prevent child injuries
Rugby is a high impact collision sport, said the letter, which was published in the Guardian newspaper on 2 March, and studies have shown that the risk of injury from rugby in under 18s is high and that the injuries are often serious. Currently, many secondary schools in the UK insist on contact rugby as a compulsory part of the physical education (PE) curriculum from age 11. The letter said, “The majority of all injuries occur during contact or collision, such as the tackle and the scrum. These injuries which include fractures, ligamentous tears, dislocated shoulders, spinal injuries, and head injuries can have short term, life long, and life ending consequences for children” (O'Dowd 2016).
Physiotherapist Advice[edit | edit source]
It is only in recent years that the Physiotherapist is seen as more of an asset where their guidance and opinion is taken into great consideration and it is becoming more of the case that they have the final say whether a player is fit to play or is able to continue due to injury or accident.
It is becoming quite common to have players wearing more equipment no matter what sport they are playing due to the growth in technology and greater knowledge now learned from extensive research.
Most Chartered Physiotherapists/Physical Therapists would take a preventative approach in terms of sport and will think of the worst case scenario as they realise from certain sports/physical activities that particular injuries are quite common and any type of protection is greatly welcome.
Market Harborough Physiotherapy & Sports Injury Clinic, to reduce the risk of injury the following may help:
“Wear the right gear. Players should wear appropriate and properly fitting footwear and clothing. Protective equipment such as protective pads, helmets, mouthpieces, face guards, protective cups, and/or eyewear should be worn for particular sports”.
You can read more about it here.
Prehabilitation[edit | edit source]
Introduction[edit | edit source]
“Intellectuals solve problems; geniuses prevent them” Albert Einstein (Brukner and Khan 2009)
Physiotherapists are often involved with the aftermath of injury or accident, which then usually consists of starting the patient on a rehabilitation programme (that can vary significantly depending on the circumstances). However, “prehabilitation” (or prehab) is a current and emerging strategy that is used both in sporting and clinical settings to help reduce injury, help maintain physical status or to improve recovery time after surgery. While there have been many studies discussing the effects of prehab in post-operative patients regarding total knee replacements (Swank et al, 2011) spinal surgery (Nielsen et al, 2010), cardiac procedures (Alkarmi, 2010), and colectomies (Gillis et al, 2014), this part of the Wiki will predominantly focus on the effects of prehabilitation to reduce injury occurrence in a sport and physical activity context, particularly in adolescents (aged 12-18). We will also discuss the physiotherapist’s role for implementing prehab programmes and the scope for more collaboration with coaches, clubs and schools to help prevent injury in adolescents when taking part in sport and physical activity.
What is Prehabilitation?[edit | edit source]
While there is no actual definition of “prehabilitation”, it is generally recognised as an injury prevention programme that is specific to the individual and chosen sport or activity. Essentially, it is specific training to prevent an injury from occurring. Meir et al (2007) suggests that “prehabilitation describes a systematic approach to identifying common injuries within a specific sport and then designing an appropriate series of exercises that work toward minimizing their incidence”. This is supported by Brukner and Khan (2009) who explain that the first step of injury prevention is to understand the incidence and severity of injuries eg. when working with a team the physiotherapist should record all injuries within the squad. This may easily be done when working with a specific sports team or club, however presents barriers for individuals who participate in sport and physical activity with no club affiliation or access to a physiotherapist. This highlights research by Castiglia (1995) who suggested that up to half of all injuries that children sustain in sport are preventable. Furthermore, Meir et al (2007) suggested that common injuries sustained in rugby might be preventable or the severity lessened if the affected area of the body goes through a specific preventative conditioning program. Perhaps if physiotherapists have a more collaborative relationship with schools and other organisations it would be possible to reach those adolescents who do not get prehabilitation/ injury prevention programmes elsewhere.
Prehabilitation programmes usually consist of strength and conditioning training, proprioception exercises, and sport specific drills. Occasionally psychological skills training may be incorporated. Below explains how these aspects of prehab can help reduce the incidence and severity of injury within adolescents.
Strength and Conditioning Training in Adolescents[edit | edit source]
Strength and conditioning is the most common type of prehabilitation used within young athletes. Studies have found that programmes that include strength, flexibility, balance, and sport‐specific fitness and technique training prevent lower limb injury (Abernethy & Bleakley, 2007). It is also thought that the benefit is continued when the prehab is performed throughout the playing season. This agrees with adult studies which used preventive programmes in volleyball resulting in significant reductions in ankle sprains (Bahr and Bahr, 1997; Stasinopoulos, 2004; Verhagen, Van der Beek et al 2004). Similarly conditioning programmes in football have shown a 50–75% reduction in injuries in general and a significant decrease in ACL injuries (Ekstand & Gillquist, 1984).
Resistance Training for Adolescents[edit | edit source]
The literature regarding resistance training in adolescents has been conflicted over the last 20 years. Studies have suggested that resistance training in youth can be harmful (Pearce, 2006). However, as well as reducing the incidence of injury, these programs can benefit children and preadolescents by improving their strength, bone density, balance, lipid profiles, fat-free mass, and personal self-esteem (Webster, Bayliss & Spadaro, 1999; 18- (Olsen et al 2005; Wedderkopp et al, 1999; Kaminski & Perrin, 1996; Caraffa et al 1996).
Additionally, strength training can help reduce injury by improving joint integrity, therefore reducing the risk of subluxation, dislocation, and strains.
Current Guidelines[edit | edit source]
The current guidelines put forward by the National Strength and Conditioning Association (NSCA) for resistance training are (Faigenbaum et al 2009):
- A properly designed and supervised resistance training program is relatively safe for youth.
- A properly designed and supervised resistance training program can enhance the muscular strength and power of youth.
- A properly designed and supervised resistance training program can improve the cardiovascular risk profile of youth.
- A properly designed and supervised resistance training program can improve motor skill performance and may contribute to enhanced sports performance of youth.
- A properly designed and supervised resistance training program can increase a young athlete's resistance to sports-related injuries.
- A properly designed and supervised resistance training program can help improve the psychosocial well-being of youth.
- A properly designed and supervised resistance training program can help promote and develop exercise habits during childhood and adolescence.
Stretching[edit | edit source]
It has long been believed that increased flexibility attained through stretching decreases injury incidence (Brukner & Khan, 2001). However, recent research by Magnusson (DATE) has suggested that “pre-exercise stretching in isolation (with or without warm up) does not reduce overall injury rates” (Brukner & Khan, 2001). Despite this, there is also research suggesting that regular stretching decreases injury incidence by 32% (Shrier, 2004). While there is conflicting research in this area, stretching is often used to help attain muscle balance within the body which may be able to help reduce injury.
Proprioceptive Training[edit | edit source]
Proprioception is the term used to describe the sensory information that contributes to the sense of body position and movement ). Proprioceptive and balance training helps the body to control the position of a joint. A common example of proprioceptive training is the use of a wobble board to improve sensory input from the ankle. It is becoming more common to incorporate proprioceptive training in prehab programmes to reduce the incidence of injury. There is good evidence for this. A systematic review by Aberneth & Bleakley (2007) looked that three studies that examined the effectiveness of various proprioceptive training. A study that investigated a home‐based proprioceptive training programme using a wobble board showed improved static and dynamic balance in healthy adolescents and reduced the incidence of injury over a 6‐month period (Emery et al, DATE). Similarly, a study by Wedderkopp et al (1999) found that female handball players using an ankle disc were less likely to be injured than a control group.
It has also been suggested that proprioception training can help with increased signals to the CNS leading to faster, ankle-stabilising and injury-preventing actions of the joints and muscles. Therefore including proprioceptive training in a prehab program could help prevent injury in adolescents.
Sport Specific Drills[edit | edit source]
- Helps prepare the body for the specific skills performed in the sport
- Helps psychologically prepare the athlete which can help reduce injuries
Common Injuries in Children Between 12-18[edit | edit source]
Osgood-Schlatters disease Sever's disease
Preventative strategies Preventative Strategies
• Stretching • Stretching
• Controlled loading • Identifying podiatry imbalances
• Minimize plyometrics
Here is a case study to get you thinking. Should prehabilitation be incorporated into a physiotherapists role? Why or why not? Should physiotherapists collaborate more with other organisations/coaches/individuals about prehabilitation? Clubs often have Strength and Conditioning coaches but not always.
Education[edit | edit source]
Introduction[edit | edit source]
A physiotherapist can use many approaches within their role to treat individuals. Some of these approaches include manual therapy, exercises, physical activity advise and educational advice (NHSa, 2016). The CSP states that a physiotherapist looks at the person as a whole, including the patient in their own care through education, awareness, empowerment and participation in their own treatment (CSP, 2013). As a physiotherapist we realise that one of our main roles is to educate patients during the treatment process. Reasons why patient education is so important are:
- Develops credibility – by educating patients it will demonstrate your knowledge and reveal you as the best resource for information and treatments.
- Develops trust – by providing information to the patient that is specific to their problem will aid in developing trust and making them feel better.
- Increases understanding – if education is provided patients will have a better understanding of their problem and how your treatment is going to help them.
- Improve compliancy – When a patient is discharged it is normal practice to provide educational materials that are informative and specific. This will leave the patient with a positive reaction to the treatment as a whole making them more likely to follow through.
That being said not all physiotherapists provide education to the best of their ability. This can be for a number of reasons such as physiotherapists are busy, lack of affordable education materials or the verbal education provided is not enough (Physical therapy web, 2016).
This section of the wiki will explore some of the areas that physiotherapists can educate patients. These areas are:
- hydration
- nutrition
- skill acquisition
- posture
- rest
Hydration[edit | edit source]
Staying hydrated is essential as your body is composed of 60% water on average (Benelam and Wyness, 2010). The water is distributed between extracellular (water in between cells and in the blood) and intercellular (inside cells) and is a main component of body fluids such as blood and synovial fluid (Benelam and Wyness, 2010). A breakdown of fluid is represented in figure 1. The concentration of body fluids is controlled by stimulating thirst or by adapting urinary output. However, if the water loss is not replaced dehydration can set in.
Dehydration can occur if you loss as little as 2% body mass. The individual can develop impaired cognitive function, headaches, decreases in physical performance and develop symptoms of fatigue (Benelam and Wyness, 2010; Ritz and Berrut; 2005, Shirreffs 2005). If an individual was to become fatigued or not able to perform at their best they increase their chance of injury whether the individual is an adult or child. As well as becoming dehydrated it is also possible to over drink where in rare cases can result in hyponatraemia, low levels of sodium (Benelam and Wyness, 2010).
The volume of water required can depends on the individual and a few factors.
- How much physical activity
- Age
- Weather
- Body composition
It is recommended that male adolescents get at least 1.9 litres per day and females need at least 1.6 litres per day (Healthy kids, 2016). However, this recommendation can change if the individual is taking part in physical activity. During physical activity you need to consume fluids to replace the fluids lost through sweat. Water is a good source of fluid for moderate physical activity although for high intensity activities lasting over 40 minutes it is suggested that drinks with a little sugar and salt would be advised (Benelam and Wyness, 2010). Some of the benefits of staying hydrated are illustrated in figure 2 (Forsythe, 2016).
Therefore, the need for physiotherapists to educate their patients to stay hydrated is a must. It can help to prevent dehydration which could reduce injury occurrences.
Nutrition
[edit | edit source]
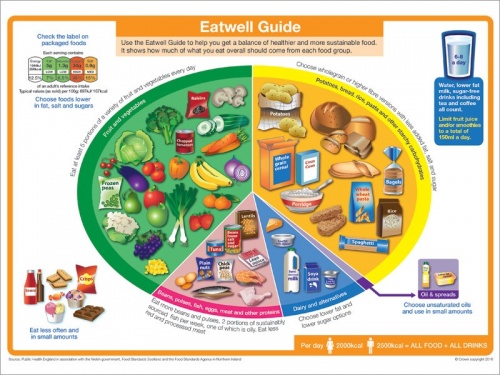
Good nutrition is important to anyone taking part in physical activity. It may not be the first common effect that you think of but your diet can help with muscle recovery. A good diet is what helps to build a strong body structure. The eatwell guide demonstrates how to maintain a well-balanced diet focussing on the five main food groups (Gov.uk,2016; NHSb, 2016). Within the guide it advises to include:
- eat at least 5 portions of fruit and vegetables a day
- Base meals on starchy carbohydrates, whole grain preferably
- Small amounts of dairy
- Protein aiming for fish two times a week
- Unsaturated oils and spreads in small amounts
- Foods high in fat, salt and sugar should be kept to a minimum
- Drink plenty of water six to eight glasses a day
To look at the eatwell guide in more detail click the picture below.
In order to prevent injuries during physical activity you should be providing adolescents with information about diet. In adolescents, healthy diets and physical activity have been proven to provide many short and long term health benefits (Biddle et al 2004; Pearson et al 2009). Despite the known benefits of eating regular well balanced meals adolescents are more likely to skip breakfast than any other meal (Dwyer et al 2001; Pearson et al 2009). According to data from the Health Behaviour in School-aged Children nearly three fifths of young people don’t meet the required fruit intake and only a third will eat vegetables (Pearson et al 2009). This is less than the recommended intake and if these adolescents were to take part in physical activity they could be increasing their chance of injury due to the body not being prepared with the adequate requirements.
There are three eating habits that have been suggested to help prevent injuries in adults (Triathlete 2011) taking part in physical activity however these habits can also relate to adolescents.
- Eat enough: If you are taking part in regular physical activity it is important to make sure that calorie intake is sufficient. If not, then the body’s ability to repair tissue damage and muscle recovery will decrease
- Keep fat in the diet: although fat has a bad name it is actually required to keep cells healthy and some fats are essential for the inflammation process.
- Calcium intake: Calcium is needed in to keep bones healthy and strong. Especially in adolescents that are still growing the need for calcium is important to reduce risk of bone strains or stress fractures
It is important for a physiotherapist to have an input in nutrition as it will coincide with the treatment process that you have come up with. Although you may feel like the easier job would be to pass this type of work over to a dietician or nutritionist this may not be the case. It may take a short conversation during treatment to change the individuals views which would be more time effective. That being said if it was a more complex case then working alongside other health professionals may be the better option.
Skill acquisition
[edit | edit source]
Posture
[edit | edit source]
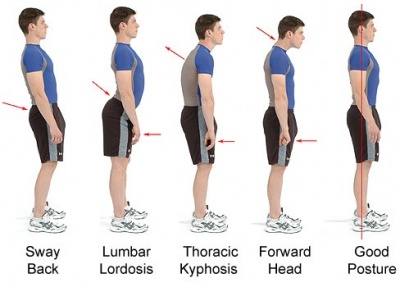
Posture can have a big effect on the prevalence of injuries in physical activity. Most adolescents are still at school where they are required to sit in a chair for periods of time resulting in slouching in a chair for example. Although this is not directly related to physical activity the same rules apply and what someone does when they are not taking part in physical activity can affect them when they do.
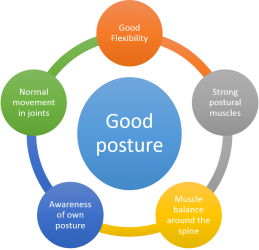
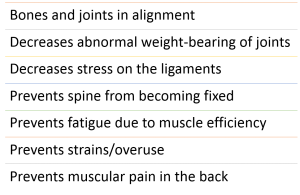
Good posture involves being able to train your body to lie, sit, walk and stand in positions where the least amount of strain is placed on ligaments and muscles (Mayfield Clinic 2016). The Mayfield Clinic has created a document that provides a detailed overview of good posture for sitting, standing and even driving. You can access that document from here. They suggest that in order to maintain a good posture you need to have certain requirements and they suggest some benefits from having a good posture:
Examples of different postures are illustrated below. The picture includes arrows to show where the change in posture has occurred. If an adolescent was to take part in exercise with bad posture they are more likely to injury themselves.
Conditions/Environment
[edit | edit source]
Rest
[edit | edit source]
Gradual progress
[edit | edit source]
Respect pain[edit | edit source]
Scenarios[edit | edit source]
Case Studies[edit | edit source]
Conclusion and Summary[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Collard D, Paw C, Van Mechelen W, Verhagen R. Design of iplay study: systematic development of a physical activity injury prevention program for primary school children. Sports Medicine 2009;39(11):889-901. https://www.ncbi.nlm.nih.gov/pubmed/19827858 (accessed 3 Nov 2016).
- ↑ National Institute for Health and Care Excellence (NICE). Obesity Clinical Knowledge Summary. http://cks.nice.org.uk/obesity#!topicsummary (accessed 25 Oct 2016).
- ↑ McCormick B, Stone I. Economic costs of obesity and the case for government intervention. Obesity reviews. 2007 Mar 1;8(s1):161-4. http://onlinelibrary.wiley.com/doi/10.1111/j.1467-789X.2007.00337.x/full (accessed 27 Oct 2016).
- ↑ Centres for Disease Control and Prevention (CDC). Childhood obesity facts. http://www.cdc.gov/obesity/data/childhood.html (accessed 26 Oct 2016).
- ↑ 5.0 5.1 Collard DC, Chinapaw MJ, Van Mechelen W. Design of the iPlay Study. Sports medicine. 2009 Nov 1;39(11):889-901. https://www.ncbi.nlm.nih.gov/pubmed/19827858 (accessed 29 Oct 2016).
- ↑ Habelt S, Hasler CC, Steinbrück K, Majewski M. Sport injuries in adolescents. Orthopedic reviews. 2011 Nov 7;3(2):18.
- ↑ Brussoni M, Brunelle S, Pike I, Sandseter EB, Herrington S, Turner H, Belair S, Logan L, Fuselli P, Ball DJ. Can child injury prevention include healthy risk promotion?. Injury prevention. 2014 Dec 22:injuryprev-2014. http://injuryprevention.bmj.com/content/21/5/344.full.pdf+html (accessed 26 Oct 2016).
- ↑ Emery CA. Injury prevention and future research. InEpidemiology of Pediatric Sports Injuries 2005 Mar 1 (Vol. 48, pp. 179-200). Karger Publishers.