Piriformis Syndrome: Difference between revisions
No edit summary |
(Undo revision 83462 by Daphne Jackson (talk)) |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Marlies Verbruggen|Marlies Verbruggen]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | </div> | ||
== Definition/Description == | |||
< | Piriformis syndrome (PS) is a painful musculoskeletal condition, characterized by a constellation of symptoms that include buttock or hip pain. [<ref name="Kirschner">Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve Jul 2009 ; 40(1) : 10-18</ref>,<ref name="Cramp">Cramp F, Bottrell O et al. Non – surgical management of piriformis syndrome : A systematic review. Physical Therapy Reviews 2007 ; 12 : 66-72. ( A1)</ref>,<ref name="Lori">Lori A, Boyajian- O’ Neill et al. Diagnosis and Management of Piriformis syndrome : an osteopathic approach. The journal of the American and osteopathic association Nov 2008; 108(11): 657-664.</ref>] In several articles, piriformis syndrome is defined as a peripheral neuritis of the branches of the sciatic nerve caused by an abnormal condition of the piriformis muscle (PM), such as an injured or irritated muscle.[<ref name="Tonley">Tonley JC, Yun SM et al. Treatment of an Individual With Piriformis syndrome Focusing on Hip Muscle Strengthening and Movement Reeducation : A case report. Journal of Orthopaedic Sports Physical Therapy 2010; 40(2): 103-111.</ref>,<ref name="Lori" />] There are more women diagnosed with Piriformis syndrome than men, the female–to–male ratio is 6:1. This ratio can be explained by the wider quadriceps femoris muscle angle in the os coxae of women. [<ref name="Shah">Shah S,Wang TW. Piriformis syndrome. eMedicine specialities :Sports medicine : hip 2009fckLRhttp://emedicine.medscape.com/article/87545-overview</ref>,<ref name="Klein">Klein MJ. Piriformis syndrome. eMedicine Specialities :Physical Medicine and Rehabilitation :Lower limb Musculoskeletal conditions 2010 fckLRhttp://emedicine.medscape.com/article/308798-overview</ref>,<ref name="Lori" />] There are two types of piriformis syndrome. The first type is called “Primary piriformis syndrome” : it is caused by an anatomic variation, like a split piriformis muscle, a split sciatic nerve or an anomalous sciatic nerve path. The second type is called “Secondary piriformis syndrome” : it is the result of a precipitating cause, such as a macrotrauma, microtraumata, ischemic mass effect and local ischemia.[<ref name="Klein" />,<ref name="Lori" />]<br> | ||
<br> | |||
== Clinically Relevant Anatomy == | |||
[[Image:Piriformis Anatomy.PNG|center|600x400px]] | |||
<br> | |||
< | |||
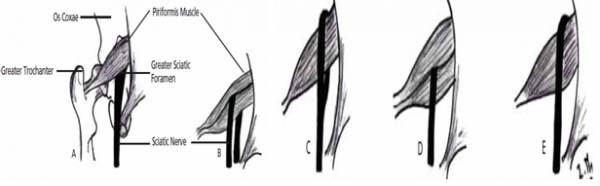
< | Variations in the relationship of the sciatic nerve to the piriformis muscle: (A) the sciatic nerve exiting the greater sciatic foramen along the inferior surface of the piriformis muscle; the sciatic nerve splitting as it passes through the piriformis muscle with the tibial branch passing (B) inferiorly or (C) superiorly; (D) the entire sciatic nerve passing through the muscle belly; (E) the sciatic nerve exiting the greater sciatic foramen along the superior surface of the piriformis muscle. | ||
< | |||
== Epidemiology /Etiology == | |||
PS is often caused by shortening or spasm of the piriformis muscle, this can result in compression or irritation of the sciatic nerve.[<ref name="Tonley" />,<ref name="Klein" />,<ref name="Hopa">Hopayian K, Song F, Riera R, Sambandan S, The clinical features of the piriformis syndrome: a systematic review. European spine Journal Jan 2010.fckLR(A1)</ref>] The spasm of the PM is mostly caused by direct trauma, post surgical injury, lumbar and sacroiliac joint pathologies and overuse.[<ref name="Tonley" />,<ref name="Shah" />,<ref name="Klein" />,<ref name="Hopa" />,<ref name="Cramp" />,<ref name="Lori" />] In 50 % of the cases, PS is caused by a (macro)trauma to the buttock(s). Therefore we can consider trauma to the buttock(s) as the main cause of PS.[<ref name="Klein" />,<ref name="Cramp" />] This direct trauma can cause inflammation of soft tissue or muscle spasm or both, which can result in nerve compression. [<ref name="Lori" />] When there is a dysfunction of the piriformis muscle, it can cause signs and symptoms of pain in the sciatic nerve distribution, such as the gluteal area, posterior thigh, posterior leg and lateral aspect of the foot. [<ref name="Shah" />] When there is an overuse of the piriformis muscle, like in long- distance walking or running or by direct compression, it can lead to microtrauma. “Wallet neuritis” is an example of direct compression : it’s a repetitive trauma from sitting on hard surfaces. [<ref name="Lori" />] | |||
Other causative factors are anatomic variations of the divisions of the sciatic nerve, anatomic variations or hypertrophy of piriformis muscle, repetitive trauma, sacro-iliac arthritis and total hip replacement.[<ref name="Shah" />,<ref name="Klein" />,<ref name="Hopa" />,<ref name="Cramp" />][[Morton's Toe|A Morton foot]] can predispose the patient to developing piriformis syndrome. A fraction of the population is at high risk, particularly skiers, truck drivers, tennis players and long-distance bikers. [<ref name="Shah" />] | |||
<br>Tonley JC [<ref name="Tonley" />] had another view about the cause of PS. He said:” The piriformis muscle may be functioning in an elongated position or subjected to high eccentric loads during functional activities secondary to weak agonist muscles. For example, if the hip excessively adducts and internally rotates during weight-bearing tasks, due to weakness of the gluteal maximus and / or the gluteus medius, a greater eccentric load may be shifted to the piriformis muscle. Perpetual loading of the piriformis muscle through overlengthening and eccentric demand may result in sciatic nerve compression or irritation”. [<ref name="Tonley" />]<br><br><br> | |||
== Characteristics/Clinical Presentation == | |||
Patients with piriformis syndrome have many symptoms that typically consist of (chronic) buttock pain, difficulty with walking and other functional activities, pain with sitting, pain with bowel movements and dyspareunia in women. [<ref name="Tonley" />,<ref name="Shah" />,<ref name="Kirschner" />,<ref name="Hopa" />,<ref name="Lori" />]. The buttock pain can radiate into the hip, the posterior aspect of the thigh and the proximal portion of the lower leg. [<ref name="Tonley" />] The pain in the buttock can also copy the low back pain. [<ref name="Shah" />] There is an aggravation of pain with activity, prolonged sitting or walking, squatting, hip adduction and internal rotation and maneuvers that increase the tension of the piriformis muscle. [<ref name="Tonley" />,<ref name="Shah" />,<ref name="Kirschner" />,<ref name="Hopa" />] It is possible that the patient walks with a limp and that he is holding his leg in a shortened and externally rotated position while supine. [<ref name="Kirschner" />] Piriformis syndrome is not characterized by neurological deficits typical for a radicular syndrome, such as declined deep tendon reflexes and myotomal weakness. Sometimes, when the patient is lying on his back, his ipsilateral foot is externally rotated. This can be a positive piriformis sign, also called a splayfoot. It can be the result of a contracted piriformis muscle. [<ref name="Klein" />,<ref name="Lori" />]<br> | |||
== Differential Diagnosis == | |||
• Lumbosacral radiculopathies | |||
• Sacroiliac joint dysfunction | |||
• Degenerative disc disease | |||
• Compression fractures | |||
< | |||
• Spinal stenosis | |||
• Sacroiliitis | |||
<br> | |||
== Pathology == | |||
There are two types of piriformis syndrome- primary and secondary. | |||
< | |||
• Primary piriformis syndrome has an anatomic cause, such as a split piriformis muscle, split sciatic nerve, or an anomalous sciatic nerve path. | |||
< | |||
< | • Secondary piriformis syndrome occurs as a result of a precipitating cause, including macrotrauma, microtrauma, ischemic mass effect, and local ischemia. | ||
Among patients with piriformis syndrome, fewer than 15% of cases have primary causes. Piriformis syndrome is most often caused by macrotrauma to the buttocks, leading to inflammation of soft tissue, muscle spasm, or both, with resulting nerve compression. Microtrauma may result from overuse of the piriformis muscle, such as in long-distance walking or running or by direct compression. An example of this kind of direct compression is “wallet neuritis” (ie, repetitive trauma from sitting on hard surfaces). | |||
< | |||
== Investigations == | |||
• Radiographic studies have limited application to the diagnosis of piriformis syndrome. Although magnetic resonance imaging and computed tomography may reveal enlargement of the piriformis muscle. • EMG results will be normal for muscles proximal to the piriformis muscle and abnormal for muscles distal to it. | |||
<br> | |||
== Outcome Measures == | |||
add links to outcome measures here (also see [[Outcome Measures|Outcome Measures Database]]) | |||
== Examination == | |||
The examination in order to diagnose piriformis syndrome consists of palpation and several clinical tests. The patient reports sensitivity during palpation at the greater sciatic notch or over the piriformis muscle belly. It is possible to detect the spasm of the PM by careful, deep palpation. [<ref name="Klein" />,<ref name="Kirschner" />,<ref name="Hopa" />]<br> | |||
The pace maneuver provokes pain in the buttock and weakness by resisted abduction and externally rotation of the hip. [<ref name="Shah" />,<ref name="Kirschner" />,<ref name="Lori" />] <br> | |||
[[Lasègue sign|Lasègue sign]], the [[Freiberg's test|Freiberg's test]] and the [[FAIR test|FAIR test]] are also tests to diagnose piriformis syndrome. | |||
< | Finally we also have another active test called : the Beatty maneuver. The patient is lying on the unaffected side and abducts the painful side upwards. The abduction causes deep buttock pain in those with PS. [<ref name="Shah" />,<ref name="Klein" />,<ref name="Lori" />]<br> | ||
Hip Adbuction Test: The patient lies on the side with lower leg flexed to provide support and the upper leg straight, in line with the trunk. The practitioner stands in front of the patient at the level of the feet and observes (no hands on) as the patient is asked to abduct the leg slowly. | |||
<br>Figure [[Image:Hip Abduction Test.png|center|350x400px]] | |||
Normal – Hip abduction to 45°.<br>Abnormal – if hip flexion occurs (indicating TFL shortness) and/or leg externally rotates (indicating piriformis shortening) and/or ‘hiking’ of the hip occurs at the outset of the movement (indicating quadratus overactivity and therefore, by implication, shortness) (Fig.)<br><br> | |||
== Medical Management <br> == | |||
add text here <br> | |||
== Physical Therapy Management <br> == | |||
[[Therapy Exercises for the Hip|Therapy Exercises for the Hip]]<br> | |||
<br> | |||
The physical therapy protocol for patients diagnosed with piriformis syndrome include several treatments performed in a specific order. To achieve a 60 – 70% improvement, the patient usually follows 2 – 3 treatments by the week for 2-3 months. [<ref name="Fishman">5.Fishman LM, Dombi GW et al. Piriformis syndrome : Diagnosis, treatment , and outcome a 10-Year study. Archives of Physical Medicine and Rehabilitation March 2002; 83 : 295-301</ref>,<ref name="Anders">Fishman LM, Anderson C, Rosner B. Botox and physical therapy in the treatment of the piriformis syndrome. American journal of physical medicine and rehabilitation 2002; 81 (12): 936-942. (A2)</ref>] | |||
<br>First of all the patient must be placed in contralateral decubitus and FAIR position (Flexed Adducted Internally Rotated). We start with an ultrasound treatment: 2.0-2.5 W/cm2, for 10-14 minutes. We apply the ultrasound gel in broad strokes longitudinally along the piriformis muscle from the conjoint tendon to the lateral edge of the greater sciatic foramen. [<ref name="Tonley" />,<ref name="Shah" />,<ref name="Fishman" />,<ref name="Cramp" />,<ref name="Anders" />,<ref name="Lori" />] Before we start with stretching of the piriformis muscle, we treat the same location with hot packs or cold spray for 10 minutes. The use of hot and cold before stretching is very useful to decrease pain. [<ref name="Tonley" />,<ref name="Shah" />,<ref name="Fishman" />,<ref name="Anders" />,<ref name="Lori" />] After that we begin with stretching of the piriformis which can be executed in different ways. We can stretch the piriformis muscle by applying manual pressure to the muscle’s inferior border. It is important not to press downward, rather directing pressure tangentially, toward the ipsilateral shoulder. Because when we press downward, we will compress the sciatic nerve against the tendinous edge of the gemellus superior. When we apply tangential pressure, we will weaken the muscle’s grip on the nerve and relieve the pain of the syndrome. [<ref name="Tonley" />,<ref name="Fishman" />,<ref name="Anders" />,<ref name="Lori" />] | |||
Another way to stretch this muscle is the FAIR position. The patient lies in supine. The hip is flexed, adducted and internally rotated. Then the patient brings his foot of the involved side across and over the knee of the other not involved leg. We can enhance the stretch, by letting the physical therapist perform a muscle–energy technique. This contains that the patient abduct his limb against light resistance, which is provided by the therapist for 5-7 seconds, with 5-7 repetitions. [ <ref name="Shah" />,<ref name="Klein" />,<ref name="Fishman" />,<ref name="Anders" />] | |||
After the stretching part we continue with myofascial release at lumbosacral paraspinal muscles and Mc Kenzie exercises. When the patient lies in FAIR position, we can use the lumbosacral corset. [<ref name="Fishman" />,<ref name="Anders" />,<ref name="Lori" />] | |||
The therapist can also give several tips to avoid an aggrevation of the symptoms. This includes : avoid sitting for a long period, stand and walk every 20 minutes, make frequent stops when driving to stand and stretch, prevent trauma to the gluteal region and avoid further offending activities. Daily stretching is recommended to avoid the recurrence of the piriformis syndrome.[ <ref name="Shah" />,<ref name="Klein" />,<ref name="Lori" />] | |||
The patient can also perform several exercises at home like : rolling side to side with flexion and extension of the knees while lying on each side, rotate side to side while standing with the arms relaxed for 1 minute every few hours, take a warm bath, lie flat on the back and raise the hips with your hands and pedal with the legs like you are riding a bicycle and finally you can execute knee bends, with as many as 6 repetitions every few hours. [<ref name="Shah" />]<br><br> | |||
== Key Research == | |||
add links and reviews of high quality evidence here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | |||
== Resources <br> == | |||
add appropriate resources here <br> | |||
== Clinical Bottom Line == | |||
add text here <br> | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | |||
<div class="researchbox"> | <div class="researchbox"> | ||
< | <rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XMgV6jliA8MRN6Ua6n63XW3D9Ftry5eh7-4zQdX9jwP5alwkA|charset=UTF-8|short|max=10</rss> | ||
</div> | </div> | ||
== References and quality level of evidence<br> == | |||
<references /> | |||
< | |||
see [[Adding References|adding references tutorial]]. | |||
<br> | |||
<br> <br> <br> | |||
[[Category:Condition]] [[Category:Hip]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Vrije_Universiteit_Brussel_Project]] | |||
Revision as of 07:43, 1 December 2013
Original Editors - Marlies Verbruggen
Top Contributors - Marlies Verbruggen, Vidya Acharya, Admin, Kudzanayi Ronald Muzenda, Kim Jackson, Ajay Upadhyay, Rachael Lowe, Nupur Smit Shah, Maëlle Cormond, Carolie Siffain, WikiSysop, Wendy Snyders, Daphne Jackson, Claire Knott, Heba El Saeid, Kai A. Sigel, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Wanda van Niekerk and Ahmed M Diab
Definition/Description[edit | edit source]
Piriformis syndrome (PS) is a painful musculoskeletal condition, characterized by a constellation of symptoms that include buttock or hip pain. [[1],[2],[3]] In several articles, piriformis syndrome is defined as a peripheral neuritis of the branches of the sciatic nerve caused by an abnormal condition of the piriformis muscle (PM), such as an injured or irritated muscle.[[4],[3]] There are more women diagnosed with Piriformis syndrome than men, the female–to–male ratio is 6:1. This ratio can be explained by the wider quadriceps femoris muscle angle in the os coxae of women. [[5],[6],[3]] There are two types of piriformis syndrome. The first type is called “Primary piriformis syndrome” : it is caused by an anatomic variation, like a split piriformis muscle, a split sciatic nerve or an anomalous sciatic nerve path. The second type is called “Secondary piriformis syndrome” : it is the result of a precipitating cause, such as a macrotrauma, microtraumata, ischemic mass effect and local ischemia.[[6],[3]]
Clinically Relevant Anatomy[edit | edit source]
Variations in the relationship of the sciatic nerve to the piriformis muscle: (A) the sciatic nerve exiting the greater sciatic foramen along the inferior surface of the piriformis muscle; the sciatic nerve splitting as it passes through the piriformis muscle with the tibial branch passing (B) inferiorly or (C) superiorly; (D) the entire sciatic nerve passing through the muscle belly; (E) the sciatic nerve exiting the greater sciatic foramen along the superior surface of the piriformis muscle.
Epidemiology /Etiology[edit | edit source]
PS is often caused by shortening or spasm of the piriformis muscle, this can result in compression or irritation of the sciatic nerve.[[4],[6],[7]] The spasm of the PM is mostly caused by direct trauma, post surgical injury, lumbar and sacroiliac joint pathologies and overuse.[[4],[5],[6],[7],[2],[3]] In 50 % of the cases, PS is caused by a (macro)trauma to the buttock(s). Therefore we can consider trauma to the buttock(s) as the main cause of PS.[[6],[2]] This direct trauma can cause inflammation of soft tissue or muscle spasm or both, which can result in nerve compression. [[3]] When there is a dysfunction of the piriformis muscle, it can cause signs and symptoms of pain in the sciatic nerve distribution, such as the gluteal area, posterior thigh, posterior leg and lateral aspect of the foot. [[5]] When there is an overuse of the piriformis muscle, like in long- distance walking or running or by direct compression, it can lead to microtrauma. “Wallet neuritis” is an example of direct compression : it’s a repetitive trauma from sitting on hard surfaces. [[3]]
Other causative factors are anatomic variations of the divisions of the sciatic nerve, anatomic variations or hypertrophy of piriformis muscle, repetitive trauma, sacro-iliac arthritis and total hip replacement.[[5],[6],[7],[2]]A Morton foot can predispose the patient to developing piriformis syndrome. A fraction of the population is at high risk, particularly skiers, truck drivers, tennis players and long-distance bikers. [[5]]
Tonley JC [[4]] had another view about the cause of PS. He said:” The piriformis muscle may be functioning in an elongated position or subjected to high eccentric loads during functional activities secondary to weak agonist muscles. For example, if the hip excessively adducts and internally rotates during weight-bearing tasks, due to weakness of the gluteal maximus and / or the gluteus medius, a greater eccentric load may be shifted to the piriformis muscle. Perpetual loading of the piriformis muscle through overlengthening and eccentric demand may result in sciatic nerve compression or irritation”. [[4]]
Characteristics/Clinical Presentation[edit | edit source]
Patients with piriformis syndrome have many symptoms that typically consist of (chronic) buttock pain, difficulty with walking and other functional activities, pain with sitting, pain with bowel movements and dyspareunia in women. [[4],[5],[1],[7],[3]]. The buttock pain can radiate into the hip, the posterior aspect of the thigh and the proximal portion of the lower leg. [[4]] The pain in the buttock can also copy the low back pain. [[5]] There is an aggravation of pain with activity, prolonged sitting or walking, squatting, hip adduction and internal rotation and maneuvers that increase the tension of the piriformis muscle. [[4],[5],[1],[7]] It is possible that the patient walks with a limp and that he is holding his leg in a shortened and externally rotated position while supine. [[1]] Piriformis syndrome is not characterized by neurological deficits typical for a radicular syndrome, such as declined deep tendon reflexes and myotomal weakness. Sometimes, when the patient is lying on his back, his ipsilateral foot is externally rotated. This can be a positive piriformis sign, also called a splayfoot. It can be the result of a contracted piriformis muscle. [[6],[3]]
Differential Diagnosis[edit | edit source]
• Lumbosacral radiculopathies
• Sacroiliac joint dysfunction
• Degenerative disc disease
• Compression fractures
• Spinal stenosis
• Sacroiliitis
Pathology[edit | edit source]
There are two types of piriformis syndrome- primary and secondary.
• Primary piriformis syndrome has an anatomic cause, such as a split piriformis muscle, split sciatic nerve, or an anomalous sciatic nerve path.
• Secondary piriformis syndrome occurs as a result of a precipitating cause, including macrotrauma, microtrauma, ischemic mass effect, and local ischemia.
Among patients with piriformis syndrome, fewer than 15% of cases have primary causes. Piriformis syndrome is most often caused by macrotrauma to the buttocks, leading to inflammation of soft tissue, muscle spasm, or both, with resulting nerve compression. Microtrauma may result from overuse of the piriformis muscle, such as in long-distance walking or running or by direct compression. An example of this kind of direct compression is “wallet neuritis” (ie, repetitive trauma from sitting on hard surfaces).
Investigations[edit | edit source]
• Radiographic studies have limited application to the diagnosis of piriformis syndrome. Although magnetic resonance imaging and computed tomography may reveal enlargement of the piriformis muscle. • EMG results will be normal for muscles proximal to the piriformis muscle and abnormal for muscles distal to it.
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
The examination in order to diagnose piriformis syndrome consists of palpation and several clinical tests. The patient reports sensitivity during palpation at the greater sciatic notch or over the piriformis muscle belly. It is possible to detect the spasm of the PM by careful, deep palpation. [[6],[1],[7]]
The pace maneuver provokes pain in the buttock and weakness by resisted abduction and externally rotation of the hip. [[5],[1],[3]]
Lasègue sign, the Freiberg's test and the FAIR test are also tests to diagnose piriformis syndrome.
Finally we also have another active test called : the Beatty maneuver. The patient is lying on the unaffected side and abducts the painful side upwards. The abduction causes deep buttock pain in those with PS. [[5],[6],[3]]
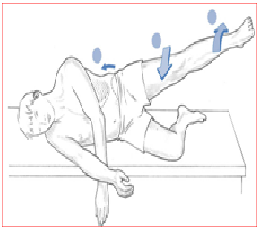
Hip Adbuction Test: The patient lies on the side with lower leg flexed to provide support and the upper leg straight, in line with the trunk. The practitioner stands in front of the patient at the level of the feet and observes (no hands on) as the patient is asked to abduct the leg slowly.
Figure
Normal – Hip abduction to 45°.
Abnormal – if hip flexion occurs (indicating TFL shortness) and/or leg externally rotates (indicating piriformis shortening) and/or ‘hiking’ of the hip occurs at the outset of the movement (indicating quadratus overactivity and therefore, by implication, shortness) (Fig.)
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
The physical therapy protocol for patients diagnosed with piriformis syndrome include several treatments performed in a specific order. To achieve a 60 – 70% improvement, the patient usually follows 2 – 3 treatments by the week for 2-3 months. [[8],[9]]
First of all the patient must be placed in contralateral decubitus and FAIR position (Flexed Adducted Internally Rotated). We start with an ultrasound treatment: 2.0-2.5 W/cm2, for 10-14 minutes. We apply the ultrasound gel in broad strokes longitudinally along the piriformis muscle from the conjoint tendon to the lateral edge of the greater sciatic foramen. [[4],[5],[8],[2],[9],[3]] Before we start with stretching of the piriformis muscle, we treat the same location with hot packs or cold spray for 10 minutes. The use of hot and cold before stretching is very useful to decrease pain. [[4],[5],[8],[9],[3]] After that we begin with stretching of the piriformis which can be executed in different ways. We can stretch the piriformis muscle by applying manual pressure to the muscle’s inferior border. It is important not to press downward, rather directing pressure tangentially, toward the ipsilateral shoulder. Because when we press downward, we will compress the sciatic nerve against the tendinous edge of the gemellus superior. When we apply tangential pressure, we will weaken the muscle’s grip on the nerve and relieve the pain of the syndrome. [[4],[8],[9],[3]]
Another way to stretch this muscle is the FAIR position. The patient lies in supine. The hip is flexed, adducted and internally rotated. Then the patient brings his foot of the involved side across and over the knee of the other not involved leg. We can enhance the stretch, by letting the physical therapist perform a muscle–energy technique. This contains that the patient abduct his limb against light resistance, which is provided by the therapist for 5-7 seconds, with 5-7 repetitions. [ [5],[6],[8],[9]]
After the stretching part we continue with myofascial release at lumbosacral paraspinal muscles and Mc Kenzie exercises. When the patient lies in FAIR position, we can use the lumbosacral corset. [[8],[9],[3]]
The therapist can also give several tips to avoid an aggrevation of the symptoms. This includes : avoid sitting for a long period, stand and walk every 20 minutes, make frequent stops when driving to stand and stretch, prevent trauma to the gluteal region and avoid further offending activities. Daily stretching is recommended to avoid the recurrence of the piriformis syndrome.[ [5],[6],[3]]
The patient can also perform several exercises at home like : rolling side to side with flexion and extension of the knees while lying on each side, rotate side to side while standing with the arms relaxed for 1 minute every few hours, take a warm bath, lie flat on the back and raise the hips with your hands and pedal with the legs like you are riding a bicycle and finally you can execute knee bends, with as many as 6 repetitions every few hours. [[5]]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XMgV6jliA8MRN6Ua6n63XW3D9Ftry5eh7-4zQdX9jwP5alwkA|charset=UTF-8|short|max=10: Error parsing XML for RSS
References and quality level of evidence
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve Jul 2009 ; 40(1) : 10-18
- ↑ 2.0 2.1 2.2 2.3 2.4 Cramp F, Bottrell O et al. Non – surgical management of piriformis syndrome : A systematic review. Physical Therapy Reviews 2007 ; 12 : 66-72. ( A1)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 Lori A, Boyajian- O’ Neill et al. Diagnosis and Management of Piriformis syndrome : an osteopathic approach. The journal of the American and osteopathic association Nov 2008; 108(11): 657-664.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Tonley JC, Yun SM et al. Treatment of an Individual With Piriformis syndrome Focusing on Hip Muscle Strengthening and Movement Reeducation : A case report. Journal of Orthopaedic Sports Physical Therapy 2010; 40(2): 103-111.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 Shah S,Wang TW. Piriformis syndrome. eMedicine specialities :Sports medicine : hip 2009fckLRhttp://emedicine.medscape.com/article/87545-overview
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Klein MJ. Piriformis syndrome. eMedicine Specialities :Physical Medicine and Rehabilitation :Lower limb Musculoskeletal conditions 2010 fckLRhttp://emedicine.medscape.com/article/308798-overview
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Hopayian K, Song F, Riera R, Sambandan S, The clinical features of the piriformis syndrome: a systematic review. European spine Journal Jan 2010.fckLR(A1)
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 5.Fishman LM, Dombi GW et al. Piriformis syndrome : Diagnosis, treatment , and outcome a 10-Year study. Archives of Physical Medicine and Rehabilitation March 2002; 83 : 295-301
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Fishman LM, Anderson C, Rosner B. Botox and physical therapy in the treatment of the piriformis syndrome. American journal of physical medicine and rehabilitation 2002; 81 (12): 936-942. (A2)
see adding references tutorial.