Positive Expiratory Pressure (PEP) Devices: Difference between revisions
(reference and images) |
(Referencing) |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Positive Expiratory Pressure (PEP) is breathing against resistance, which can be performed either through a device or against pursed lips<ref name=":0">Monika Fagevik Olse ́n a, 2015</ref> . | Positive Expiratory Pressure (PEP) is breathing against resistance, which can be performed either through a device or against pursed lips<ref name=":0">Monika Fagevik Olse ́n a, b,c,*, Louise Lannefors d, Elisabeth Westerdahl e,f.Positive expiratory pressure e Common clinical applications and physiological effects.Respiratory Medicine.2015;105;297- 307.</ref> . | ||
'''Mechanism of PEP''' | '''Mechanism of PEP''' | ||
| Line 13: | Line 13: | ||
==== Types of PEP ==== | ==== Types of PEP ==== | ||
Some literature has described PEP as two types varying in pressure range low and high pressure PEP. Low pressure PEP ranges from 5-20cm H2O at mid-expiration, whereas high-pressure PEP ranges from 26-102cm H2O which is achieved by maximal inspiration followed by performing forced expiratory maneuver into PEP mask<ref> | Some literature has described PEP as two types varying in pressure range low and high pressure PEP. Low pressure PEP ranges from 5-20cm H2O at mid-expiration, whereas high-pressure PEP ranges from 26-102cm H2O which is achieved by maximal inspiration followed by performing forced expiratory maneuver into PEP mask<ref>RRT-NPS, Timothy R Myers.Positive Expiratory Pressure and Oscillatory Positive Expiratory Pressure Therapies.Respiratory Care.Oct 2007;52;10;1308-1327.</ref>. Other sources have described PEP as a three airways techniques that has been developed based on expiratory resistance:- PEP, High Positive Expiratory Pressure (HiPEP), and Oscillatory Positive Expiratory Pressure (OscPEP)<ref name=":0" />. | ||
* PEP | * PEP | ||
** Involves breathing against expiratory resistance to temporarily increase [https://en.wikipedia.org/wiki/Functional_residual_capacity Functional Residual Capacity (FRC)]and [https://en.wikipedia.org/wiki/Tidal_volume Tidal Volume (VT)]accompanied by clearance techniques such as [http://bronchiectasis.com.au/physiotherapy/techniques/forced-expiration-technique Forced Expiratory Technique (FET), huffing, and or coughing]<ref name=":0" />. | ** Involves breathing against expiratory resistance to temporarily increase [https://en.wikipedia.org/wiki/Functional_residual_capacity Functional Residual Capacity (FRC)]and [https://en.wikipedia.org/wiki/Tidal_volume Tidal Volume (VT)]accompanied by clearance techniques such as [http://bronchiectasis.com.au/physiotherapy/techniques/forced-expiration-technique Forced Expiratory Technique (FET), huffing, and or coughing]<ref name=":0" />. | ||
| Line 23: | Line 23: | ||
==== Indications for PEP ==== | ==== Indications for PEP ==== | ||
* Acute and chronic respiratory failure for reasons of surgery <ref name=": | * Acute and chronic respiratory failure for reasons of surgery <ref name=":0" /> | ||
* Neurological or musculoskeletal dysfunction<ref name=":02" /> | * Neurological or musculoskeletal dysfunction<ref name=":02">Monika Fagevik Olse ́n a, b,c,*, Louise Lannefors d, Elisabeth Westerdahl e,f.Positive expiratory pressure e Common clinical applications and physiological effects.Respiratory Medicine.2015;105;297- 307.</ref> | ||
* Old age and immobility<ref name=":02" /> | * Old age and immobility<ref name=":02" /> | ||
* To increase lung volume by increasing FRC and VT<ref name=":02" /> | * To increase lung volume by increasing FRC and VT<ref name=":02" /> | ||
| Line 56: | Line 56: | ||
Face mask with a one-way valve to which expiratory resistors are attached or face-mask connected to a plastic ring drilled by holes of different caliber that act as resistors. Both devices could be suited to mouthpiece application if necessary. These systems are considered to be ''flux-dependent''. | Face mask with a one-way valve to which expiratory resistors are attached or face-mask connected to a plastic ring drilled by holes of different caliber that act as resistors. Both devices could be suited to mouthpiece application if necessary. These systems are considered to be ''flux-dependent''. | ||
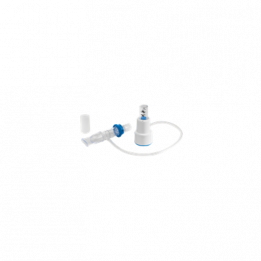
[https://www.pari.com/uk-en/products/pari-pep-systems/pari-pep-s-system-1/ '''PARI S-System'''] | [https://www.pari.com/uk-en/products/pari-pep-systems/pari-pep-s-system-1/ '''PARI S-System'''] <ref name=":3">PARI S-System.https://www.pari.com/uk-en/products/pari-pep-systems/pari-pep-s-system-1/<nowiki/>(accessed 25 June 2018)</ref> [https://www.smiths-medical.com/products/respiratory/bronchial-hygiene/therapep-pep-therapy-system '''TheraPEP'''] | ||
''[https://www.pari.com/fileadmin/user_upload/PARI.com_UK/Doc/IFU/018D4000-E-de-en-IFU-PARI-PEP-S.pdf Instructions] - [https://www.pari.com/fileadmin/user_upload/PARI.com_UK/Doc/Docs/018D4008-EN-UK-PARI-PEP-S-short-ifu.pdf Brochure] - [http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-pari-pep Video]'' | ''[https://www.pari.com/fileadmin/user_upload/PARI.com_UK/Doc/IFU/018D4000-E-de-en-IFU-PARI-PEP-S.pdf Instructions]''<ref name=":3" /> ''- [https://www.pari.com/fileadmin/user_upload/PARI.com_UK/Doc/Docs/018D4008-EN-UK-PARI-PEP-S-short-ifu.pdf Brochure]''<ref name=":3" /> ''- [http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-pari-pep Video]''<ref>Positive Expiratory Pressure Therapy using PARI PEP.http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-pari-pep (accessed 25 June 2018).</ref> [http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-thera-pep ''Video'']<ref>Positive Expiratory Pressure Therapy using Thera PEP.http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-thera-pep (accessed 25 June 2018)</ref> | ||
[[File:PARI PEP S-System.jpg|alt=PARI S-System|left|thumb|[https://www.pari.com/uk-en/products/pari-pep-systems/pari-pep-s-system-1/ PARI S-System] ]] | [[File:PARI PEP S-System.jpg|alt=PARI S-System|left|thumb|[https://www.pari.com/uk-en/products/pari-pep-systems/pari-pep-s-system-1/ PARI S-System] ]]<ref name=":3" />[[File:TheraPEP.png|alt=Smiths Medical- TheraPEP|center|thumb|261x261px|[https://www.smiths-medical.com/products/respiratory/bronchial-hygiene/therapep-pep-therapy-system Smiths Medical] TheraPEP ]]<ref>TheraPEP® PEP Therapy System.https://www.smiths-medical.com/products/respiratory/bronchial-hygiene/therapep-pep-therapy-system (accessed 25 June 2018). | ||
[[File:TheraPEP.png|alt=Smiths Medical- TheraPEP|center|thumb|261x261px|[https://www.smiths-medical.com/products/respiratory/bronchial-hygiene/therapep-pep-therapy-system Smiths Medical] TheraPEP ]] | </ref> | ||
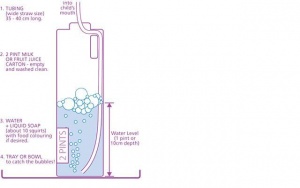
A very common ''threshold-dependent'' system is "PEP Bottle" that consists of a bottle filled with a predetermined quantity of water in which a tube that draws from the bottom. Patient blows into the tube and has to overcome the pressure opposed by the level of water until bubbles are produced. | A very common ''threshold-dependent'' system is "PEP Bottle" that consists of a bottle filled with a predetermined quantity of water in which a tube that draws from the bottom. Patient blows into the tube and has to overcome the pressure opposed by the level of water until bubbles are produced. | ||
[https://www.cincinnatichildrens.org/health/b/Bubble-PEP '''PEP Bottle'''] [https://www.cincinnatichildrens.org/health/b/Bubble-PEP ''(Instructions)''] | [https://www.cincinnatichildrens.org/health/b/Bubble-PEP '''PEP Bottle''']<ref name=":4">Bubble PEP (Positive Expiratory Pressure). Cincinnati Children's.https://www.cincinnatichildrens.org/health/b/Bubble-PEP<nowiki/>(accessed 25 June 2018). | ||
[[File:Bubble PEP.jpg|alt=Cincinnati Childrens- https://www.cincinnatichildrens.org/health/b/Bubble-PEP|center|thumb|[https://www.cincinnatichildrens.org/health/b/Bubble-PEP Bubble PEP] ]] | </ref> [https://www.cincinnatichildrens.org/health/b/Bubble-PEP ''(Instructions)'']<ref name=":4" /> | ||
[[File:Bubble PEP.jpg|alt=Cincinnati Childrens- https://www.cincinnatichildrens.org/health/b/Bubble-PEP|center|thumb|[https://www.cincinnatichildrens.org/health/b/Bubble-PEP Bubble PEP] ]]<ref name=":4" /> | |||
PEP may also be applied togheter with vibrations with oscillating PEP (OscPEP) devices . | PEP may also be applied togheter with vibrations with oscillating PEP (OscPEP) devices . | ||
Revision as of 14:29, 25 June 2018
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Lucinda hampton, Fatemah Ali Fairouz, Kim Jackson, Uchechukwu Chukwuemeka, Riccardo Guarise, Adam Vallely Farrell, Vidya Acharya, Merinda Rodseth and Amanda Ager
Introduction[edit | edit source]
Positive Expiratory Pressure (PEP) is breathing against resistance, which can be performed either through a device or against pursed lips[1] .
Mechanism of PEP
The increase in pressure is transmitted to airways creating back pressure stenting them during exhalation [2], therefore preventing premature airway closure thus reducing gas trapping [3]. It promotes collateral ventilation, allowing pressure to build up distal to the obstruction[2] . Not only does PEP retains airways from collapsing and prolongs expiratory flow, it is effective airway clearance promoting movement of mucus proximally [3].
- Collateral Ventilation:Is a phenomenon found in the human lungs where alveolar structures are ventilated through passages or channels that bypass normal airways[4].
Types of PEP[edit | edit source]
Some literature has described PEP as two types varying in pressure range low and high pressure PEP. Low pressure PEP ranges from 5-20cm H2O at mid-expiration, whereas high-pressure PEP ranges from 26-102cm H2O which is achieved by maximal inspiration followed by performing forced expiratory maneuver into PEP mask[5]. Other sources have described PEP as a three airways techniques that has been developed based on expiratory resistance:- PEP, High Positive Expiratory Pressure (HiPEP), and Oscillatory Positive Expiratory Pressure (OscPEP)[1].
- PEP
- Involves breathing against expiratory resistance to temporarily increase Functional Residual Capacity (FRC)and Tidal Volume (VT)accompanied by clearance techniques such as Forced Expiratory Technique (FET), huffing, and or coughing[1].
- HiPEP
- Involves breathing against resistance by augmenting expiratory flow using FVC[1].
- OscPEP
- Is a technique that utilizes both PEP when exhaling against resistance and flow oscillation in exhalation[1].
Indications for PEP[edit | edit source]
- Acute and chronic respiratory failure for reasons of surgery [1]
- Neurological or musculoskeletal dysfunction[6]
- Old age and immobility[6]
- To increase lung volume by increasing FRC and VT[6]
- Reduce hyperinflation[6]
- Improve airway clearance[6]
Physiology of PEP[edit | edit source]
Literature has stated theoretical explanations that discuss the physiology behind PEP therapy and its effects on cardiopulmonary status. The theories are:-
Increasing lung volume FRC and VT[edit | edit source]
- A progressively temporary increase in FRC has been found to be proportionally correlated when increasing PEP[6]
- An increase in FRC is attained by alteration of breathing pattern that is a product of a decrease in expiratory flow and an increase in expiratory time leading to exhalation of smaller volumes[6].
- lung volume increase is achieved by altering breathing pattern, thereby increasing VT and decreasing respiratory frequency, which is due to an increase in muscle activity of inspiratory and expiratory muscles[6].
- Improved gas exchange is a result of breathing during a prolonged period with normalized lung volumes[6].
Reduction of hyperinflation[edit | edit source]
- Hyperinflation is a result of air entrapment causing the lungs to over inflate. It is caused by muscle spasm, mucosal inflammation, hyper-secretions, reduced lung elasticity due to destruction of lung parenchyma. If Untreated may lead to inspiratory muscle exhaustion, decreased ventilation, and deficient gas exchange[6].
- PEP reduces expiratory flow, which in return decreases the declining pressure across the airway wall thereby reducing collapse[6].
- Increasing pressure within airways transports EPP centrally and in stable airways therefore stenting them. Reduction of airway collapse increases expired volume leading to additional emptying of lung volume thus lowering FRC and improving ventilation distribution and gas exchange[6].
Airway Clearance[edit | edit source]
When using HiPEP
- It homogenously mobilize secretions in collapsed airways. It aims towards increasing FRC by recruiting collapsed lung volumes and uses resistance to obtain progressive homogenization emptying of the lungs[6].
- Homogenization is achieved by the facilitation of EPP to move peripherally during expiration avoiding collapsed airways, trapped gas, and atelectasis. This results in reduction of respiratory flow and an increase in expiratory flow combined with an increase in FRC. In doing so secretion is mobilized in closed or collapsed and unreachable parts of the lungs. HiPEP is proven to be an airway clearance technique equally or more effective than PEP[6].
When using OscPEP
- The oscillating property is achieved by bursts and turbulent expiratory airflow due to the opening and closing of the valve. Oscillations during expiration decreases the viscoelasticity properties of mucus, effecting its movement which depends on the oscillating frequency. OscPEP is equally as effective as other Airway Clearance Technique (ACT) as PEP and Active Cycle Breathing Technique (ACBT)[6].
Different PEP devices[edit | edit source]
PEP therapy may be applied through:
Face mask with a one-way valve to which expiratory resistors are attached or face-mask connected to a plastic ring drilled by holes of different caliber that act as resistors. Both devices could be suited to mouthpiece application if necessary. These systems are considered to be flux-dependent.
Instructions[7] - Brochure[7] - Video[8] Video[9]
A very common threshold-dependent system is "PEP Bottle" that consists of a bottle filled with a predetermined quantity of water in which a tube that draws from the bottom. Patient blows into the tube and has to overcome the pressure opposed by the level of water until bubbles are produced.
PEP Bottle[11] (Instructions)[11]
PEP may also be applied togheter with vibrations with oscillating PEP (OscPEP) devices .
Aerobika® , Acapella®, VibraPEP®, vPEP® are flux-dependent plastic-made devices with a general mechanism of opening and vibrating.
OscPEP can also be applied with a threshold-dependent mechanism with a high density steel "movable ball" that is interposed on a funnel or circular cone between the exhalation tract of the device causing a vibration that is transmitted to the lungs (examples are PARI O PEP®, Flutter® , TurboForte®, PEPE).
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Monika Fagevik Olse ́n a, b,c,*, Louise Lannefors d, Elisabeth Westerdahl e,f.Positive expiratory pressure e Common clinical applications and physiological effects.Respiratory Medicine.2015;105;297- 307.
- ↑ 2.0 2.1 Downs, Anne Mejia.Cadiovascular and Pulmonary Physical Therapy Evidence and Practice 4th ed.:Donna Frownfelter, Elizabeth Dean.
- ↑ 3.0 3.1 Cerny, Joan C Darbee Patricia J Ohtake Brydon JB Grant Frank J. Physiologic Evidence for the Efficacy of Positive Expiratory Pressure as an Airway Clearance Technique in Patients With Cystic Fibrosis. Physical Therapy.(1 June 2004).
- ↑ E J Cetti, A J Moore, D M Geddes.Collateral ventilation.Thorax. May 2006;61;5;371-373
- ↑ RRT-NPS, Timothy R Myers.Positive Expiratory Pressure and Oscillatory Positive Expiratory Pressure Therapies.Respiratory Care.Oct 2007;52;10;1308-1327.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 Monika Fagevik Olse ́n a, b,c,*, Louise Lannefors d, Elisabeth Westerdahl e,f.Positive expiratory pressure e Common clinical applications and physiological effects.Respiratory Medicine.2015;105;297- 307.
- ↑ 7.0 7.1 7.2 7.3 PARI S-System.https://www.pari.com/uk-en/products/pari-pep-systems/pari-pep-s-system-1/(accessed 25 June 2018)
- ↑ Positive Expiratory Pressure Therapy using PARI PEP.http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-pari-pep (accessed 25 June 2018).
- ↑ Positive Expiratory Pressure Therapy using Thera PEP.http://bronchiectasis.com.au/resources/videos/positive-expiratory-pressure-therapy-using-thera-pep (accessed 25 June 2018)
- ↑ TheraPEP® PEP Therapy System.https://www.smiths-medical.com/products/respiratory/bronchial-hygiene/therapep-pep-therapy-system (accessed 25 June 2018).
- ↑ 11.0 11.1 11.2 Bubble PEP (Positive Expiratory Pressure). Cincinnati Children's.https://www.cincinnatichildrens.org/health/b/Bubble-PEP(accessed 25 June 2018).