Quadriceps Muscle Strain
Original Editors - Maxime Tuerlinckx
Top Contributors - Mandeepa Kumawat, Maxime Tuerlinckx, Carlos Areia, Lucinda hampton, Shanna Blyckaerts, Admin, Shaimaa Eldib, Kim Jackson, Wanda van Niekerk, Jelle Van Hemelryck, Rachael Lowe, Frederik Töpke, Joao Costa, WikiSysop, Claire Knott, Fasuba Ayobami, 127.0.0.1, Rucha Gadgil, Evan Thomas, Scott Buxton, Naomi O'Reilly and Daphne Jackson
Search strategy[edit | edit source]
We looked after information on different databases like Web of Science, PubMed, PEDro, Web of Knowledge, etc. The keywords that we used were quadriceps muscle strain, muscle strain, quadriceps strain, quadriceps strain therapy, quadriceps injury, muscle injury, etc.
Definition/Description[edit | edit source]
A quadriceps muscle strain is an acute tearing injury of the quadriceps,more specific a partial tear of the small fibers of the muscles that make up the quadriceps group.[1] This injury is usually due to an acute stretch of the muscle often at the same time of a forceful contraction or repetitive functional overloading. The quadriceps which consists of four parts, can be overloaded by repeated eccentric muscle contractions of the knee extensor mechanism.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title When the muscle is elongated by an eccentric contraction, high muscle forces are generated during the elongation and added to the forces produced by the passive connective tissue so it almost certainly induces a muscle strain injury. This force is several times higher than the force produced during a maximal isometric contraction.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinically Relevant Anatomy[edit | edit source]
There are generally three mechanisms for quadriceps strain. 1. Sudden deceleration of the leg (kicking), 2. violent contraction of the quadriceps (sprinting) and 3. rapid deceleration of an overstretched muscle (by quickly change of direction).
The quadriceps femoris acts as a hip flexor and knee extender. This muscle is composed of 4 subcomponents:
- Rectus femoris
- -Vastus medialis
- -Vastus lateralis
- Vastus intermedius
The rectus femoris originates at the ilium, thus crossing both the hip and knee joint along its course. The remaining muscles originate on the femur. These four muscles are innervated by the femoral nerve.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
These four muscles come together in the quadriceps tendon and insert to the base of the patella.
The true insertion of the quadriceps femoris is into the tibial tubercle, but convention considers it as inserting into the patella through the quadriceps tendon or the suprapatellar tendon. The part distal to the sesamoid bone is known as the patellar ligament (ligamentum patellae), patellar tendon, or infrapatellar tendon.[2]
The Rectus femoris is the only part of the muscle participating in both flexion of the hip and extension of the knee. The other 3 parts are only involved in the extension of the knee. The rectus femoris is the most superficial part of the quadriceps and it crosses both the hip and knee joints. So it is more susceptible to stretch-induced strain injuries. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The most common sites of strains are the muscle tendon junction just above the knee (both distal and proximal but most frequently at the distal muscle-tendon) and in the muscle itself.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Muscle functions:
-Rectus Femoris: Hip flexion, Knee extension
-Vastus Lateralis: Knee extension
-Vastus Intermedius: Knee extension
-Vastus Medialis: Knee extension
-Semitendinosus: Hip extension, Knee flexion
-Semimembranosus: Hip extension, Knee flexion
-Biceps Femoris: Hip extension, Knee flexion
Epidemiology/ Etiology[edit | edit source]
There are generally three mechanisms for quadriceps strain.
- Sudden deceleration of the leg (kicking),
- violent contraction of the quadriceps (sprinting) and
- rapid deceleration of an overstretched muscle (by quickly change of direction).
The most commonly strained quadriceps muscle is the M. Rectus Femoris, because he crosses two joints and has a high proportion of type 2 fibers. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The strongest risk factor for developing a quadriceps muscle strain injury is a recent history of muscle strains. The next strongest risk factor in line is a past history of a quadriceps muscle strain. Other risk factors for this injury may include low muscle strength, an imbalance between the quadriceps and the hamstrings, limited flexibility, muscle fatigue, a poor technique, a high percentage of Type II fibers in the muscle, and so on. Another possible cause of strain injury can be a bad warming-up before an exercise or no warming-up at all. The majority of quadriceps strains (incurred by kicking sports) are located in the dominant leg, because it is the preferred kicking leg which is used more often.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation[edit | edit source]
Typically a muscle strain is characterized by a violent muscle contraction occurring simultaneously with an excessively forced stretch. The vast majority of muscle strains involve muscles that pass over two joints or more or occur in muscles with complex architecture (Brewer 1962). In the anterior thigh the rectus femoris is most vulnerable to strains.
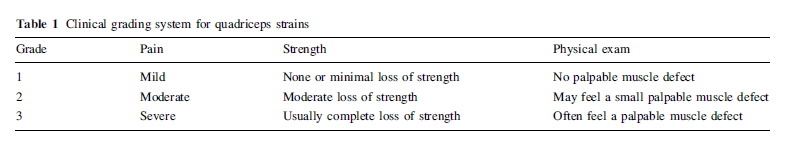
Various ways of grading muscle strains have been proposed. Factoring in pain, loss of strength, and physical exam findings in a grading system helps provide guidance for treatment, rehabilitation, and eventual return to play. The table below provides an outline of a clinical grading system for muscle strains.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Grade 1 strains represent minor tearing of muscle fibers with only minimal or no loss in strength. Pain is usually mild to moderate with no palpable defect in the muscle tissue on exam.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Grade 2 strains involve more severe disruption to the muscle fibers with significant pain and loss of strength. A defect in the muscle tissue may sometimes be felt. Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Grade 3 strains are a result of complete tearing of the muscle with associated severe pain and complete loss of strength. A palpable defect in the muscle tissue can frequently be felt, especially if examined at onset of injury prior to hematoma formation.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Although most of the times trauma history is associated, evaluation methods can be used to identify the strained muscle.
Examples of evaluation methods:
- Hamstrings/Quadriceps ratio (H : Q)
- Range of motion (ROM) and End-feel
- Muscle strengh
- Skin temperature
- Pain(while flexing, stretching or using the muscles)[1]
- Muscle spasms[1]
- Swelling[1]
- Bruises, if the blood vessels are broken/damaged[1]
Differential Diagnosis[edit | edit source]
- Contusion
- Jumper's Knee
- Femoral Neck Stress Fracture
- Slipped Capital Femoral Epiphysis[3]
Diagnostic procedures[edit | edit source]
Most acute injuries in the quadriceps muscles can be found easily by the therapist by just letting the patient tell how the injury occurred and doing a quick examination of the quadriceps muscles afterwards. But when the therapist isn’t too sure, he can always consider medical imaging to give a definite answer. Medical imaging tells us for example the exact type and location of the muscle strain.[4]Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
After obtaining a thorough history, a careful examination should ensue including observation, palpation, strength testing, and evaluation of motion. Strain injuries of the quadriceps may present with an obvious deformity such as a bulge or defect in the muscle belly. Ecchymosis may not develop until 24 h after the injury. Palpation of the anterior thigh should include the length of the injured muscle, locating the area of maximal tenderness and feeling for any defect in the muscle. Strength testing of the quadriceps should include resistance of knee extension and hip flexion. Adequate strength testing of the rectus femoris must include resisted knee extension with the hip flexed and extended. Practically, this is best accomplished by evaluating the patient in both a sitting and prone-lying position. The prone-lying position also allows for optimum assessment of quadriceps motion and flexibility. Pain is typically felt by the patient with resisted muscle activation, passive stretching, and direct palpation over the muscle strain. Assessing tenderness, any palpable defect, and strength at the onset of muscle injury will determine grading of the injury and provide direction for further diagnostic testing and treatment.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
There are several types of medical imaging which can be used for muscle strains:
- Radiographs: a positive point about radiographs is that they are good to differentiate the etiology of the pain in the quadriceps muscles. Etiologies can be muscular (muscle strain etc.) or bony (stress fracture etc.).
- Ultrasound (US): Ultrasound is very often used because it is relatively inexpensive. But it also has a quite big disadvantage, namely the fact that it’s highly operator dependent and requires a skilled and experienced clinician. Another advantage of US is the fact that it has the ability to image the muscles dynamically and to asses for bleedings and hematoma formation via Doppler.
- Magnetic resonance imaging (MRi): Mri Is a good way to give detailed images of the muscle injury. If it’s not clear on the Mri images whether it’s a contusion or a strain, the therapist must rely on the story the patient told him about how the injury occurred. And then he can deduce whether it’s the one or the other.[5]Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Outcome measures[edit | edit source]
A significant evidence of a reduction in swelling with ice and simultaneous exercises in comparison with thermotherapy has been found by Bleakley c et al. Another trial found that continuous ice application led to statistically significant reductions in pain.[6]
A group of quadriceps injuries received treatment with application of a maximum compression bandage was compared to a control group where subjects were treated with rest and elevation only. No significant differences in time to complete subjective recovery were noted by Thorsson O. et al.[7]
Examination[edit | edit source]
Its often present:
- Tenderness provoked by direct palpation at the injury site.
- Pain during resisted extension
- Ely's test
An examination should include observation, palpation, strength testing and evaluation of the range of motion (ROM). When we are testing the strength of the muscle, this must happen with resisted knee extension with the hip both flexed and extended. And as mentioned above, this will result in pain when the muscle is damaged. When the muscle is damaged, the patient will also feel pain while the muscle is passively stretched. When the examination is done, the therapist will be able to determine the grading of the injury. When the examination isn’t clear enough, we can use medical imaging to give the decisive answer. Palpation of the anterior thigh should include the length of the injured muscle, locating the area of maximal tenderness and feeling for any defect in the muscle.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Medical Management
[edit | edit source]
The use of NSAID's ( nonsteroidal anti-inflammatory drugs) is still contorversial, their benefit, cost and potential adverse effects may be taken into consideration. If used, it should be during the inflamatory period (48h-72h) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Surgical Intervention may be necessary if there is a complete quadriceps muscle rupture.
There has been an experimental study (1998) about the use of hyperbaric oxygen therapy. The therapy should be applied during the early phase of the repair of the injured muscle.
This therapy could accelerate the repair of the injured muscle.
But we should be careful to extend these findings to clinical practice, because there haven’t been any clinical studies to show the beneficial effects of this therapy in the treatment of muscle or other types of soft tissue injuries in athletes yet.[8][5]
Surgery
One should exercise extreme caution in considering surgical intervention in the treatment of muscle injuries, as a properly executed nonoperative treatment results in a good outcome in virtually all cases. In fact, the phrase muscle injuries do heal conservatively could be used as a guiding principle in the treatment of muscle traumas. Having said that, there are certain highly specific indications in which surgical intervention might actually be beneficial. These indications include an athlete with a large intramuscular hematoma(s), a complete (III degree) strain or tear of a muscle with few or no agonist muscles, or a partial (II degree) strain if more than half of the muscle belly is torn. Also, surgical intervention should be considered if a patient complains of persisting extension pain (duration, >4-6 months) in a previously injured muscle, particularly if the pain is accompanied by a clear extension deficit. In this particular case, one has to suspect the formation of scar adhesions restricting the movement of the muscle at the site of the injury, a phenomenon that often requires surgical deliberation of the adhesions. If surgery is indeed warranted in the treatment of an acute skeletal muscle injury, the following general principles are recommended: the entire hematoma and all necrotic tissue should be carefully removed from the injured area. One should not attempt to reattach the ruptured stumps of the muscle to each other via sutures unless the sutures can be placed through a fascia overlying the muscle. Sutures placed solely through myofibers possess virtually no strength and will only pierce through the muscle tissue. Loop-type sutures should be placed very loosely through the fascia, as attempts to overtighten them will only cause them to pierce through the myofibers beneath the fascia, resulting in additional damage to the injured muscle. It needs to be emphasized here that sutures might not always provide the required strength to reappose all ruptured muscle fibers, and accordingly, the formation of empty gaps between the ruptured muscle stumps cannot always be completely prevented. As a general rule of thumb, the surgical repair of the injured skeletal muscle is usually easier if the injury has taken place close to the MTJ, rather than in the middle of the muscle belly, because the fascia overlying the muscle is stronger at the proximity of the MTJ, enabling more exact anatomical reconstruction. In treating muscle injuries with 2 or more overlying compartments, such as the m. quadriceps femoris, one should attempt to repair the fascias of the different compartments separately, beginning with the deep fascia and then finishing with the repair of the superficial fascia. After surgical repair, the operated skeletal muscle should be supported with an elastic bandage wrapped around the extremity to provide some compression (relative immobility, no complete immobilization, eg, in cast, is needed). Despite the fact that experimental studies suggest that immobilization in the lengthened position substantially reduces the atrophy of the myofibers and the deposition of connective tissue within the skeletal muscle in comparison to immobilization in the shortened position, the lengthened position has an obvious draw-back of placing the antagonist muscles in the shortened position and, thus, subjecting them to the deleterious effects of immobility. After a careful consideration of all the above-noted information, we have adopted the following postoperative treatment regimen for operated muscle injuries: the operated muscle is immobilized in a neutral position with an orthosis that prevents one from loading the injured extremity. The duration of immobilization naturally depends on the severity of the trauma, but patients with a complete rupture of the m. quadriceps femoris or gastrocnemius are instructed not to bear any weight for 4 weeks, although one is allowed to cautiously stretch the operated muscle within the limits of pain at 2 weeks postoperatively. Four weeks after operation, bearing weight and mobilization of the extremity are gradually initiated until approximately 6 weeks after the surgery, after which there is no need to restrict the weightbearing at all. Experimental studies have suggested that in the most severe muscle injury cases, operative treatment may provide benefits. If the gap between the ruptured stumps is exceptionally long, the denervated part of the muscle may become permanently denervated and atrophied. Under such circumstances, the chance for the reinnervation of the denervated stump is improved, and the development of large scar tissue within the muscle tissue can possibly be at least partly prevented by bringing the retracted muscle stumps closer together through (micro) surgical means. However, in the context of experimental studies, it should be noted that the suturation of the fascia does not prevent contraction of the ruptured muscle fibers or subsequent formation of large hematoma in the deep parts of the muscle belly.[5]
Physical Therapy Management
[edit | edit source]
When a quadriceps muscle strain occurs during a competition or training, it is important to react immediately. In the 10 minutes following the trauma one needs to put the knee of the affected leg immediately in 120° of flexion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title This avoids potential muscle spasms, reduces the hemorrhage and minimizes the risk of developing myositis ossificansCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
If the knee is left in extension the healing process will be slower and more painful because the quadriceps will start to heal in a shortened position.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The rest of the therapy during the healing process is based on the RICE therapy. This includes:
- Rest,
- Ice treatment for 20 minutes every 2-3 hours,
- Compression with an ACE bandage
- Elevation.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Rest prevents worsening of the initial injury. Ice or cold application is thought to lower intra-muscular temperature and decrease blood flow to the injured area. Compression may help decrease blood flow and accompanied by elevation will serve to decrease both blood flow and excess interstitial fluid accumulation. The goal is to prevent hematoma formation and interstitial edema, thus decreasing tissue ischemia. However, if the immobilization phase is prolonged, it will be detrimental for muscle regeneration.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
By placing the injured extremity to rest the first 3-7 days after the trauma, we can prevent further retraction of the ruptured muscle stumps (the formation of a large gap within the muscle), reduce the size of the hematoma, and subsequently, the size of the connective tissue scar.[5] The elevation of an injured extremity above the level of heart results in a decrease in hydrostatic pressure, and subsequently, reduces the accumulation of interstitial fluid, so there is less swelling at the place of injury.[9] But it needs to be stressed that there is not a single randomized, clinical trial to validate the effectiveness of the RICE-principle in the treatment of soft tissue injury.[6]
Regarding the use of cold on injured skeletal muscle, it has been shown that early use of cryotherapy is associated with a significantly smaller hematoma between the ruptured myofiber stumps, less inflammation and tissue necrosis, and somewhat accelerated early regeneration.[10][11] But according to the most recent data on topic (2007), icing of the injured skeletal muscle should continue for an extended period of time (6 hours) to obtain substantial effect on limiting the hemorrhaging and tissue necrosis at the site of the injury.[12]
During the first few days after the injury, a short period of immobilization accelerates the formation of granulation tissue at the site of injury, but it should be noted that the duration of reduced activity (immobilization) ought to be limited only until the scar reaches sufficient strength to bear the muscle-contraction induced pulling forces without re-rupture. At this point, gradual mobilization should be started followed by a progressively intensified exercise program to optimize the healing by restoring the strength of the injured muscle, preventing the muscle atrophy, the loss of strength and the extensibility, all of which can follow prolonged immobilization.[13]
This hasn’t been proved in scientific literature, but it is commonly used by physiotherapists and doctors. Before a patient turn back to normal activities, he or she should do some exercises and stretching to reinforce the quadriceps and hamstrings- muscle. The exercises can be isometric, isotonic, isokinetic and in a later stage of the revalidation sport- or ADL-specific.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title An overview of the types of exercises:
- isometric: muscle contraction without change in muscle length (mostly against a fixed object).
- isotonic: muscle contraction against a constant resistance with a shortening/lengthening of the muscle.
- isokinetic: muscle contraction by a specific movement (e.g. flexion-extension of the knee).
All of these exercises should be done in a range of motion that is pain-free. These strengthening exercises will also help in preventing from a new strain injury.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Key research[edit | edit source]
Resources[edit | edit source]
Clinical bottom line[edit | edit source]
Recent Related Research (from Pubmed)
[edit | edit source]
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Department of pediatrics. Quadriceps strain. http://pediatrics.med.nyu.edu/conditions-we-treat/conditions/quadriceps-strain (accessed 17 November 2014)
- ↑ Waligora AC, Johanson NA, Hirsch BE. Clinical Anatomy of the Quadriceps Femoris and Extensor Apparatus of the Knee. Clin Orthop Relat Res. 2009; 467(12): 3297–3306 (2A)
- ↑ Medscape. Drugs And Diseases: Slipped Capital Femoral Epiphysis. http://emedicine.medscape.com/article/91596-overview (accessed November 23, 2014)
- ↑ Tero AH Järvinen, Markku Järvinen, Hannu Kalimo; Regeneration of injured skeletal muscle after the injury; Muscles, Ligaments and Tendons Journal 2013; 3 (4): 337-345 (2A)
- ↑ 5.0 5.1 5.2 5.3 Järvinen TAH, Järvinen TLN, Kääriäinen M, Kalimo H, Järvinen M. Muscle InjuriesfckLRBiology and Treatment. The American Journal of Sports Medicine Vol. 33, No. 5, 2005 745-764 (2A)
- ↑ 6.0 6.1 Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. American Journal of Sports Medicine 2004; 32(1): 251-261. (2A)
- ↑ Thorsson 0, Lilja B, Nilsson P, Westlin N. Immediate external com- pression in the management of an acute muscle injury. Scand J Med Sci Sports 1997: 7: 182-190. 0 Munksgaard, 1997 (2A)
- ↑ Best TM, Loitz-Ramage B, Corr DT, Vanderby R. Hyperbaric oxygen in the treatment of acute muscle stretch injuries: results in an animal model. Am J Sports Med. 1998;26:367-372.) (2A)
- ↑ tero
- ↑ Hurme T, Rantanen J, Kalimo H. Effects of early cryotherapy in experimental skeletal muscle injury. Scand J Med & Sci Sports 1993;3:46-51. (2B)
- ↑ Deal DN, Tipton J, Rosencrance E, Curl WW, Smith TL. Ice reduces edema. A study of microvascular permeability in rats. J Bone & Joint Surg 2002;84-A:1573-1578. (2A)
- ↑ Schaser K-D et al., Prolonged superficial local cryotherapy attenuates microcirculatory impairment, regional inflammation, and muscle necrosis following closed soft tissue injury in rats. Am J Sports Med 2007;35:93-102. (2B)
- ↑ Delos D., et al. Muscle Injuries in Athletes: Enhancing Recovery Through Scientific Understanding and Novel Therapies. Sports Health 2013; 5(4): 346-352. (1A)