Red Flags in Spinal Conditions: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="noeditbox">Welcome to [[Nottingham University Spinal Rehabilitation Project|Nottingham University's Spinal Rehabilitation Project]]. Students are currently creating this page. Please check back in January 2014 to see the finished result.</div> <div class="editorbox"> | <div class="noeditbox">Welcome to [[Nottingham University Spinal Rehabilitation Project|Nottingham University's Spinal Rehabilitation Project]]. Students are currently creating this page. Please check back in January 2014 to see the finished result.</div><div class="editorbox"> | ||
'''Original Editor '''- Anna Butler, Fiona Stohrer and Kat Moon .... as part of the [[Nottingham University Spinal Rehabilitation Project]] | '''Original Editor '''- Anna Butler, Fiona Stohrer and Kat Moon .... as part of the [[Nottingham University Spinal Rehabilitation Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= What are red flags?<br> | = What are red flags?<br> = | ||
Part of the UK guidelines for an assessment of lower back pain is to rule out serious pathology and identify red flags (Koes et al. 2010). Red flags are features from a patients subjective and objective assessment which is thought to put them at a higher risk of serious pathology and warrant referral for further diagnostic testing (Henschke et al. 2013). Red flags often highlight non-mechanical conditions or pathologies of visceral origin (E. Mulligan). Red flags can be contraindications to many Physiotherapy treatments. | Part of the UK guidelines for an assessment of lower back pain is to rule out serious pathology and identify red flags (Koes et al. 2010). Red flags are features from a patients subjective and objective assessment which is thought to put them at a higher risk of serious pathology and warrant referral for further diagnostic testing (Henschke et al. 2013). Red flags often highlight non-mechanical conditions or pathologies of visceral origin (E. Mulligan). Red flags can be contraindications to many Physiotherapy treatments. | ||
<br>Although red flags have a valid role to play in assessment and diagnosis they should also be used with caution. Some guidelines contain no information on diagnostic accuracy for individual red flags, so it is the responsibility of individual practitioners to make themselves aware of these. Other guidelines even recommend immediate referral to imaging if any red flag is present, which could lead to many unnecessary referrals if clinicians did not clinically reason their referral (Downie et al. 2013). <br> | <br>Although red flags have a valid role to play in assessment and diagnosis they should also be used with caution. Some guidelines contain no information on diagnostic accuracy for individual red flags, so it is the responsibility of individual practitioners to make themselves aware of these. Other guidelines even recommend immediate referral to imaging if any red flag is present, which could lead to many unnecessary referrals if clinicians did not clinically reason their referral (Downie et al. 2013). <br> | ||
== History of red flags == | == History of red flags == | ||
| Line 16: | Line 16: | ||
== Red Herrings == | == Red Herrings == | ||
Red Herrings are “any misleading biomedical or psychosocial factors that will deflect the course of accurate clinical reasoning” (Greenhalgh). When assessing lower back pain red herrings can mislead a clinician into misdiagnosis resulting in a delay in appropriate treatment for the pathology causing the lower back pain.<br> | Red Herrings are “any misleading biomedical or psychosocial factors that will deflect the course of accurate clinical reasoning” (Greenhalgh). When assessing lower back pain red herrings can mislead a clinician into misdiagnosis resulting in a delay in appropriate treatment for the pathology causing the lower back pain.<br> | ||
== Spinal Masqueraders<br> | == Spinal Masqueraders<br> == | ||
<span style="line-height: 1.5em | <span style="line-height: 1.5em">Spinal masqueraders are conditions which present as lower back pain but are actually caused by non-mechanical referred pain from a structure not part of the spine.</span><span style="line-height: 1.5em"> </span> | ||
<span style="line-height: 1.5em | <span style="line-height: 1.5em">Spinal masqueraders are examples of where red herrings can sometimes lead to misdiagnosis. Patients will present with lower back pain but the source is not a mechanical structure (Walcott et al 2011). Although the percentage of patients seen by Physiotherapists with these conditions is small it is important to be able to recognise the red flags that could point towards these conditions. </span><br> | ||
</span><br> | |||
Some of the sources of visceral pain include:<br>• Inflammation - eg appendicitis <br>• Distention - eg bowel obstruction<br>• Ischemia - eg a tumour blocking blood supply<br>The blood supply to internal organs is in close proximity to the sympathetic nerve system so changes to the blood supply from ischemia, distention of inflammation can directly affect the nerve innervation (Eveliegh 2013).<br> | Some of the sources of visceral pain include:<br>• Inflammation - eg appendicitis <br>• Distention - eg bowel obstruction<br>• Ischemia - eg a tumour blocking blood supply<br>The blood supply to internal organs is in close proximity to the sympathetic nerve system so changes to the blood supply from ischemia, distention of inflammation can directly affect the nerve innervation (Eveliegh 2013).<br> | ||
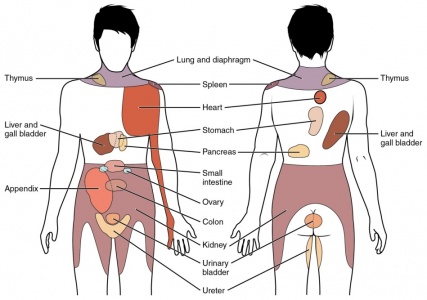
This diagram depicts the most commong referral patterns for visceral pathologies. | This diagram depicts the most commong referral patterns for visceral pathologies. | ||
[[Image:Visceral pain referral.jpg| | [[Image:Visceral pain referral.jpg|427x300px]] | ||
(Eveliegh 2013) | (Eveliegh 2013) | ||
| Line 37: | Line 36: | ||
It is hard to get an exact picture of the epidemiology of red flags as it depends heavily on the level of documentation by clinicians. One study by Leerar et al, 2007 suggested that “the documentation of red flags was comprehensive in some areas (age over 50, bladder dysfunction, history of cancer, immune suppression, night pain, history of trauma, saddle anaesthesia and lower extremity neurological deficit) but lacking in others (weight loss, recent infection, and fever/chills)”. | It is hard to get an exact picture of the epidemiology of red flags as it depends heavily on the level of documentation by clinicians. One study by Leerar et al, 2007 suggested that “the documentation of red flags was comprehensive in some areas (age over 50, bladder dysfunction, history of cancer, immune suppression, night pain, history of trauma, saddle anaesthesia and lower extremity neurological deficit) but lacking in others (weight loss, recent infection, and fever/chills)”. | ||
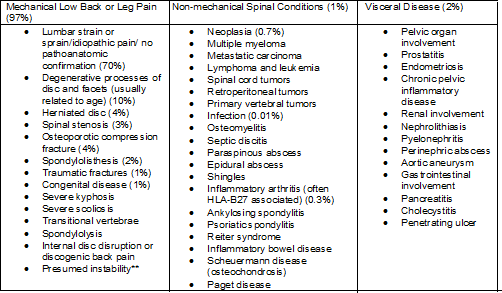
<br>This model was suggested by the 1994 Clinical Standards Advisory Group for the proportion of serious spinal pathologies.<br> | <br>This model was suggested by the 1994 Clinical Standards Advisory Group for the proportion of serious spinal pathologies.<br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
This table shows further breakdown of the conditions lower back pain patients present with. | This table shows further breakdown of the conditions lower back pain patients present with. | ||
[[Image:Spinal.png| | [[Image:Spinal.png|502x293px]] | ||
Figures in brackets indicate estimated percentages of patients with these conditions among all adult patients with signs and symptoms of low back pain. Percentages may vary substantially according to demographic. Data obtained from Deyo et al | Figures in brackets indicate estimated percentages of patients with these conditions among all adult patients with signs and symptoms of low back pain. Percentages may vary substantially according to demographic. Data obtained from Deyo et al | ||
(Jarvik et al. 2002)<br> | (Jarvik et al. 2002)<br> | ||
= Subjective History - Red Flags = | = Subjective History - Red Flags = | ||
| Line 77: | Line 76: | ||
In the UK age above 55 years is considered a red flag (CSAG 1994), this is because above this age, particularly above 65, the chances of being diagnosed with many serious pathologies, such as cancers, increase (Greenhalgh and Selfe). | In the UK age above 55 years is considered a red flag (CSAG 1994), this is because above this age, particularly above 65, the chances of being diagnosed with many serious pathologies, such as cancers, increase (Greenhalgh and Selfe). | ||
== History of cancer<br> | == History of cancer<br> == | ||
A patient history of cancer and also family history of cancer should be established, particularly in a first degree relative, such as a parent or sibling (Greenhalgh and Selfe). The most common forms of metastatic cancer are: breast, lung and prostate (Jarvik 2002). | A patient history of cancer and also family history of cancer should be established, particularly in a first degree relative, such as a parent or sibling (Greenhalgh and Selfe). The most common forms of metastatic cancer are: breast, lung and prostate (Jarvik 2002). | ||
| Line 113: | Line 112: | ||
This can also be considered a yellow flag and should be taken with caution as many patients suffer episodic lower back pain. However, patients who initially respond to treatment and then relapse may be a cause for concern (Greenhalgh and Selfe). | This can also be considered a yellow flag and should be taken with caution as many patients suffer episodic lower back pain. However, patients who initially respond to treatment and then relapse may be a cause for concern (Greenhalgh and Selfe). | ||
== Other <br> | == Other <br> == | ||
*Systemically unwell | *Systemically unwell | ||
| Line 122: | Line 121: | ||
*Cauda Equina symptoms: urinary retention, faecal incontinence, unilateral or bilateral sciatica, reduced straight leg raise and saddle anaesthesia | *Cauda Equina symptoms: urinary retention, faecal incontinence, unilateral or bilateral sciatica, reduced straight leg raise and saddle anaesthesia | ||
(Greenhalgh and Selfe)<br> | (Greenhalgh and Selfe)<br> | ||
= Objective History = | = Objective History = | ||
The subjective assessment will provide the therapist with the majority of the information needed to clarify cause of symptoms <ref>Eveleigh, C. Red Flags and Spinal Masquereders. [online]. Available at : www.nspine.co.uk/.../09-nspine2013-red-flags-masqueraders.ppt. Accessed 13/01/14. 2013.</ref><br> | The subjective assessment will provide the therapist with the majority of the information needed to clarify cause of symptoms <ref>Eveleigh, C. Red Flags and Spinal Masquereders. [online]. Available at : www.nspine.co.uk/.../09-nspine2013-red-flags-masqueraders.ppt. Accessed 13/01/14. 2013.</ref><br> | ||
== Physical Appearance == | == Physical Appearance == | ||
| Line 132: | Line 131: | ||
The therapist should determine if the patient is unwell objectively however this is a very subjective concept. The following signs may indicate that the patient has a systemic serious pathology<ref name="G+S2006">Greenhalgh, S. and Selfe, J. Red Flags: A guide to identifying serious pathology of the spine. Churchill Livingstone: Elsevier. 2006.</ref>. | The therapist should determine if the patient is unwell objectively however this is a very subjective concept. The following signs may indicate that the patient has a systemic serious pathology<ref name="G+S2006">Greenhalgh, S. and Selfe, J. Red Flags: A guide to identifying serious pathology of the spine. Churchill Livingstone: Elsevier. 2006.</ref>. | ||
• Pallor/flushing<br>• Sweating<br>• Altered complexion: sallow/jaundiced<br>• Tremor/shaking<br>• Tired<br>• Dishevelled/unkempt<br>• Halitosis<br>• Poorly fitting clothes | • Pallor/flushing<br>• Sweating<br>• Altered complexion: sallow/jaundiced<br>• Tremor/shaking<br>• Tired<br>• Dishevelled/unkempt<br>• Halitosis<br>• Poorly fitting clothes | ||
== Observation == | == Observation == | ||
=== Deformity of the spine === | === Deformity of the spine === | ||
Deformity of the spine with muscle spasm and severe limitation of movement are suggested to be key indicators of serious spinal pathology<ref name="G+S2006" />. A rapid onset of a scoliosis may be indicative of an osteoma or osteoblastoma however this may not be apparant in standing. Physiological movements are often required to detemine a rapid onset scoliosis | Deformity of the spine with muscle spasm and severe limitation of movement are suggested to be key indicators of serious spinal pathology<ref name="G+S2006" />. A rapid onset of a scoliosis may be indicative of an osteoma or osteoblastoma however this may not be apparant in standing. Physiological movements are often required to detemine a rapid onset scoliosis | ||
Some spinal tumors can be large enough to be seen or felt. Swelling and tenderness may be the first sign of a tumour<ref name="G+S2006" />. It is also common for spinal tumours to limit physiological movements. | Some spinal tumors can be large enough to be seen or felt. Swelling and tenderness may be the first sign of a tumour<ref name="G+S2006" />. It is also common for spinal tumours to limit physiological movements. | ||
=== Muscle Spasm === | === Muscle Spasm === | ||
This is suggested to be synonymous with low back pain and is therefore difficult to determine if it is associated with a red flag pathology. If a serious spinal pathology is present, the muscle spasm may be severe enough to be a cause of scoliosis in the spine<ref name="G+S2006" />. The correlation between muscle spasm, pain and other objective clinical measurements however, are poorly supported by strong evidence<ref name="G+S2006" />. | This is suggested to be synonymous with low back pain and is therefore difficult to determine if it is associated with a red flag pathology. If a serious spinal pathology is present, the muscle spasm may be severe enough to be a cause of scoliosis in the spine<ref name="G+S2006" />. The correlation between muscle spasm, pain and other objective clinical measurements however, are poorly supported by strong evidence<ref name="G+S2006" />. | ||
=== Neurological Assessment === | === Neurological Assessment === | ||
Patients who report neurological signs in the subjective assessment require a neurological assessment<ref name="P+M">Petty, N. J. and Moore, A. P. Neuromuscular examination and assessment: a handbook for therapists. Edingburgh: Churchill Livingstone. 2001.</ref>. A neurological deficit is rarely the first presenting symptom in a patient with serious spinal pathology however 70% of patients will have a neurological deficit at the time of diagnosis <ref name="G+S2006" /> | Patients who report neurological signs in the subjective assessment require a neurological assessment<ref name="P+M">Petty, N. J. and Moore, A. P. Neuromuscular examination and assessment: a handbook for therapists. Edingburgh: Churchill Livingstone. 2001.</ref>. A neurological deficit is rarely the first presenting symptom in a patient with serious spinal pathology however 70% of patients will have a neurological deficit at the time of diagnosis <ref name="G+S2006" /> | ||
The dermatomes, myotomes and reflexes should be examined. The upper motor neurone should also be examined via extensor plantar reflex (Babinski), clonus and hoffmans. If brisk, it may indicate a upper motor neurone pathlogy<ref name="G+S2006" />. | The dermatomes, myotomes and reflexes should be examined. The upper motor neurone should also be examined via extensor plantar reflex (Babinski), clonus and hoffmans. If brisk, it may indicate a upper motor neurone pathlogy<ref name="G+S2006" />. | ||
= Diagnostic Tests = | = Diagnostic Tests = | ||
'''What is differential diagnosis?'''<br> | '''What is differential diagnosis?'''<br> | ||
<br>A systematic process in which tools such as clinical tests are used to identify the proper diagnosis from a competing set of possible diagnoses. (Whiting et al, 2008) <br> | <br>A systematic process in which tools such as clinical tests are used to identify the proper diagnosis from a competing set of possible diagnoses. (Whiting et al, 2008) <br> | ||
<br>'''For a clinical test to be the ''best ''test?'''<br>• Reliable<br>• Low Cost<br>• Validated findings<br>• High diagnostic Accuracy = SPECIFICITY AND SENSITIVITY <br> | <br>'''For a clinical test to be the ''best ''test?'''<br>• Reliable<br>• Low Cost<br>• Validated findings<br>• High diagnostic Accuracy = SPECIFICITY AND SENSITIVITY <br> | ||
<br>'''SPECIFICITY'''<br>Is the percentage of people who test negative for a specific disease among a group of people who do not have the disease (Sackett et al 2000)<br>'''SENSITIVITY'''<br>Percentage of people who test positive for a specific disease among a group of people who have the disease (Sackett et al, 2000).<br> | <br>'''SPECIFICITY'''<br>Is the percentage of people who test negative for a specific disease among a group of people who do not have the disease (Sackett et al 2000)<br>'''SENSITIVITY'''<br>Percentage of people who test positive for a specific disease among a group of people who have the disease (Sackett et al, 2000).<br> | ||
'''<br>Likelihood ratio''' = The Likelihood Ratio (LR) is the likelihood that a given test result would be expected in a patient with the target disorder compared to the likelihood that that same result would be expected in a patient without the target disorder. (http://www.cebm.net/?o=1158) <br>http://www.physio-pedia.com/Test_Diagnostics<br> | '''<br>Likelihood ratio''' = The Likelihood Ratio (LR) is the likelihood that a given test result would be expected in a patient with the target disorder compared to the likelihood that that same result would be expected in a patient without the target disorder. (http://www.cebm.net/?o=1158) <br>http://www.physio-pedia.com/Test_Diagnostics<br> | ||
<br>'''High sensitivity and LOW LR''' = RULE OUT people who don’t have the disease<br>'''High specificity and HIGH LR''' = RULE IN people who have the disease | <br>'''High sensitivity and LOW LR''' = RULE OUT people who don’t have the disease<br>'''High specificity and HIGH LR''' = RULE IN people who have the disease | ||
| Line 170: | Line 169: | ||
<br>'''Tests :''' Compression fractures<br>The examiner stands behind the patient. The patient stands facing a mirror so that the examiner can gauge their reaction. The entire length of the spine is examined using firm, closed-fist percussion. <br>'''Positive =''' when the patient complains of a sharp, sudden pain. | <br>'''Tests :''' Compression fractures<br>The examiner stands behind the patient. The patient stands facing a mirror so that the examiner can gauge their reaction. The entire length of the spine is examined using firm, closed-fist percussion. <br>'''Positive =''' when the patient complains of a sharp, sudden pain. | ||
<br>Table 1. A table to show sensitivity, specificity and likelihood ratios of the Percussion diagnostic test for compression fracture. (Langdon et al 2009)<br><br><br> | <br>Table 1. A table to show sensitivity, specificity and likelihood ratios of the Percussion diagnostic test for compression fracture. (Langdon et al 2009)<br><br><br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br> | <br> | ||
<br><br> | <br><br> | ||
= Clinical Reasoning = | = Clinical Reasoning = | ||
| Line 186: | Line 185: | ||
[http://www.physio-pedia.com/Clinical_Reasoning. Clinical Reasoning ]is integral to physiotherapy practice. As a concept, clinical reasoning is quite a simple one however in practice, it is difficult and fraught with errors. The aim of clinical reasoning is to prevent misdirection <ref name="Jones">Jones, M. Clinical reasoning and pain. Manual Therapy. 1, pp: 17 – 24. 1995.</ref>The way a therapsit clinically reasons their finidings can strongly influence how the case is interpreted. This has implications as to how the clinician views the red flags and gives weight to any red herrings presented therein <ref name="G+S2004">Greenhalgh, S. and Selfe, J. Margaret: a tragic case of spinal Red Flags and Red Herrings. Physiotherapy. 90, pp: 73 – 76. 2004</ref> | [http://www.physio-pedia.com/Clinical_Reasoning. Clinical Reasoning ]is integral to physiotherapy practice. As a concept, clinical reasoning is quite a simple one however in practice, it is difficult and fraught with errors. The aim of clinical reasoning is to prevent misdirection <ref name="Jones">Jones, M. Clinical reasoning and pain. Manual Therapy. 1, pp: 17 – 24. 1995.</ref>The way a therapsit clinically reasons their finidings can strongly influence how the case is interpreted. This has implications as to how the clinician views the red flags and gives weight to any red herrings presented therein <ref name="G+S2004">Greenhalgh, S. and Selfe, J. Margaret: a tragic case of spinal Red Flags and Red Herrings. Physiotherapy. 90, pp: 73 – 76. 2004</ref> | ||
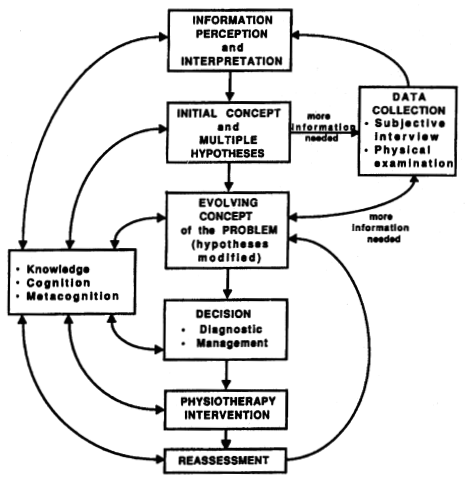
The most common form of clinical reasoning within the physiotherapy profession is hypothetico-deductive reasoning <ref name="Doody">Doody, C. and McAteer, M. Clinical reasoning of expert and novice physiotherapists in an outpatient orthopaedic | The most common form of clinical reasoning within the physiotherapy profession is hypothetico-deductive reasoning <ref name="Doody">Doody, C. and McAteer, M. Clinical reasoning of expert and novice physiotherapists in an outpatient orthopaedic setting. Physiotherapy. 88 (5), pp: 258 – 268. 2002.</ref>Within hypothetico-deductive reasoning, the clinician gains initial clues in regards to the patients problem (from the subjective assessment) which forms initial hypotheses in the therapists mind. Further data is collected in the objective assessment which may confirm or negate the hypotheses. Continual hypothesis generation may occur during management and reassessment <ref name="Ed2004">Edwards, I., Jones, M., Carr, J., Braunack-Mayer, A. and Jensen, G. M. Clinical Reasoning Strategies in Physical Therapy. Physical Therapy. 84 (4), pp: 312 - 335. 2004</ref> | ||
[http://www.physio-pedia.com/Opportunity_to_reflect! Reflection] after the initial assessment and also after the subsequent sessions will help the therapist to recognise mechanical and non-mecahnical patterns and their clinical reasoning process will improve <ref name="Jones" /> <ref name="G+S2008">Greenhalgh, S. Red Flags, and clinical Presentation Mapping. [online]. Available at: https://www.macpweb.org/home/index.php?m=file&f=873. Accessed 21/12/13. 2008</ref> | [http://www.physio-pedia.com/Opportunity_to_reflect! Reflection] after the initial assessment and also after the subsequent sessions will help the therapist to recognise mechanical and non-mecahnical patterns and their clinical reasoning process will improve <ref name="Jones" /><ref name="G+S2008">Greenhalgh, S. Red Flags, and clinical Presentation Mapping. [online]. Available at: https://www.macpweb.org/home/index.php?m=file&amp;f=873. Accessed 21/12/13. 2008</ref> | ||
== Process of Clinical Reasoning == | == Process of Clinical Reasoning == | ||
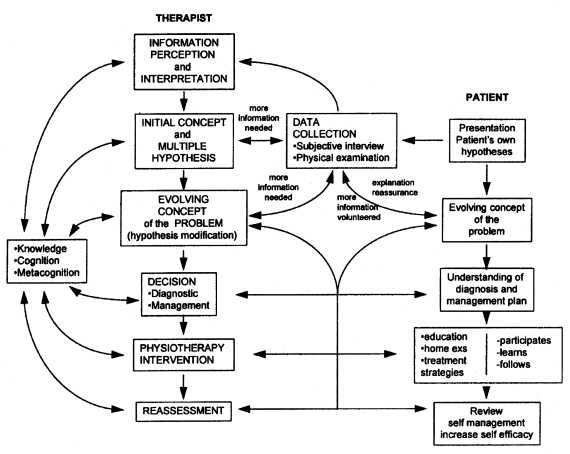
Clinical reasoning should begin as soon as the therapist meets the patient as their behaviour can inform the therapists clinical reasoning <ref name="G+S2006" />There should be ongoing data collection which should not stop at the end of the assessment to aid this process. A hyptothetico-deductive model of clinical reasoning can be seen in Figure 1. | Clinical reasoning should begin as soon as the therapist meets the patient as their behaviour can inform the therapists clinical reasoning <ref name="G+S2006" />There should be ongoing data collection which should not stop at the end of the assessment to aid this process. A hyptothetico-deductive model of clinical reasoning can be seen in Figure 1. | ||
[[Image:Clinical reasoning.png|Figure 1: Hypothetico-deductive model of Clinical Reasoning (Jones,1995).]] | [[Image:Clinical reasoning.png|Figure 1: Hypothetico-deductive model of Clinical Reasoning (Jones,1995).]] | ||
Figure 1: A Hypothetico-deductive model of Clinical Reasoning<ref name="Jones" /> <br> | Figure 1: A Hypothetico-deductive model of Clinical Reasoning<ref name="Jones" /> <br> | ||
The therapist may be able to ascertain quickly that something is wrong with the patient due to the subjective and objective assessment along wither their subsequent clinical reasoning. The data gathered over sessions should be collated to best inform the therapist. This will contribute to the therapists evolving concept of the patients’ problem<ref name="G+S2006" /><ref name="Jones" />. | The therapist may be able to ascertain quickly that something is wrong with the patient due to the subjective and objective assessment along wither their subsequent clinical reasoning. The data gathered over sessions should be collated to best inform the therapist. This will contribute to the therapists evolving concept of the patients’ problem<ref name="G+S2006" /><ref name="Jones" />. | ||
| Line 202: | Line 201: | ||
== Pattern Recognition == | == Pattern Recognition == | ||
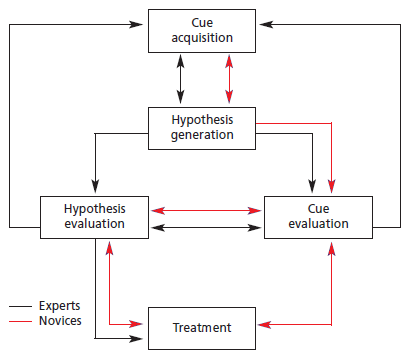
Pattern recognition is an important part of clinical reasoning however this will be limited in students and newly qualified physiotherapists <ref name="Jones" /> <ref name="Doody" /> | Pattern recognition is an important part of clinical reasoning however this will be limited in students and newly qualified physiotherapists <ref name="Jones" /><ref name="Doody" /> | ||
Knowledge is also an important consideration. The newly qualified therapist is expected to have many more potential hypotheses in comparison to a experienced therapist <ref name="Jones" />. There is suggested to be differences in novice and expert therapists in the process of clinical reasoning<ref name="Doody" />. Although largely similar, novice physiotherapists have to go through a longer process of clinical reasoning compared to expert therapists due to lack of knowledge in comparison; and less experience in pattern recognition. Figure 2 demonstrates the clinical reasoning process of expert therapists (with at least 3 years of experience) and novice therapists (with under three years’ experience or students)<ref name="Doody" />.<br> | Knowledge is also an important consideration. The newly qualified therapist is expected to have many more potential hypotheses in comparison to a experienced therapist <ref name="Jones" />. There is suggested to be differences in novice and expert therapists in the process of clinical reasoning<ref name="Doody" />. Although largely similar, novice physiotherapists have to go through a longer process of clinical reasoning compared to expert therapists due to lack of knowledge in comparison; and less experience in pattern recognition. Figure 2 demonstrates the clinical reasoning process of expert therapists (with at least 3 years of experience) and novice therapists (with under three years’ experience or students)<ref name="Doody" />.<br> | ||
[[Image:Diff in clinical reasoning.png]] | [[Image:Diff in clinical reasoning.png]] | ||
Figure 2: Difference in clinical reasoning between expert and novice therapists <ref name="Doody" />. | Figure 2: Difference in clinical reasoning between expert and novice therapists <ref name="Doody" />. | ||
== Patient involvement in the clinical reasoning process == | == Patient involvement in the clinical reasoning process == | ||
The patient should be an integral part of the clinical reasoning process as this can help the clinician to form hypotheses and lead towards the review of the outcome post physiotherapy intervention <ref name="Jones" /> (See Figure 3). | The patient should be an integral part of the clinical reasoning process as this can help the clinician to form hypotheses and lead towards the review of the outcome post physiotherapy intervention <ref name="Jones" />(See Figure 3). | ||
[[Image:Patient involve.png]] | [[Image:Patient involve.png]] | ||
| Line 220: | Line 219: | ||
== Errors in Clinical Reasoning == | == Errors in Clinical Reasoning == | ||
Patients’ inappropriate misattribution of insidious symptoms to a traumatic event is common and can be misleading<ref name="G+S2004" />. Clinical reasoning is only as good as the information on which it is based indicating the importance of thorough questioning in the subjective assessment <ref name="G+S2008" /> | Patients’ inappropriate misattribution of insidious symptoms to a traumatic event is common and can be misleading<ref name="G+S2004" />. Clinical reasoning is only as good as the information on which it is based indicating the importance of thorough questioning in the subjective assessment <ref name="G+S2008" /> | ||
The three types of errors that can occur in clinical reasoning include:<br>- Faulty perception or elicitation of cues<br>- Incomplete factual knowledge<br>- Misapplication of known facts to a specific problem | The three types of errors that can occur in clinical reasoning include:<br>- Faulty perception or elicitation of cues<br>- Incomplete factual knowledge<br>- Misapplication of known facts to a specific problem | ||
== Red Herrings == | == Red Herrings == | ||
Within the clinical reasoning process, the therapist should determine if there are logical inferences in regards to the information they are recieving from the patient <ref name="G+S2004" />. The therapist should not be reassured by previous investigations being reported on as normal <ref name="G+S2008" />. In the early stages, serious spinal pathology is difficult to detect and weight loss will not always be evident in these early stages <ref name="G+S2003">Greenhalgh, S. and Selfe, J. Malignant Myeloma of the spine: Case Report. Physiotherapy. 89 (8), pp: 486 – 488.</ref> | Within the clinical reasoning process, the therapist should determine if there are logical inferences in regards to the information they are recieving from the patient <ref name="G+S2004" />. The therapist should not be reassured by previous investigations being reported on as normal <ref name="G+S2008" />. In the early stages, serious spinal pathology is difficult to detect and weight loss will not always be evident in these early stages <ref name="G+S2003">Greenhalgh, S. and Selfe, J. Malignant Myeloma of the spine: Case Report. Physiotherapy. 89 (8), pp: 486 – 488.</ref> | ||
= Management of red flags = | = Management of red flags = | ||
== Students Responsibility == | == Students Responsibility == | ||
| Line 238: | Line 237: | ||
In some cases the red flags may be obvious. If serious enough, the therapist may refer onto Accident and Emergency. This may be the case in cauda equina syndrome for further surgical opinion <ref name="Chau">Chau, A. M. T., Xu, L. L., Pelzer, N. R. and Gragnaniello, C. (2013). Timing of surgical intervention in cauda equine syndrome – a systematic critical review. World Neurosurgery. 12</ref> | In some cases the red flags may be obvious. If serious enough, the therapist may refer onto Accident and Emergency. This may be the case in cauda equina syndrome for further surgical opinion <ref name="Chau">Chau, A. M. T., Xu, L. L., Pelzer, N. R. and Gragnaniello, C. (2013). Timing of surgical intervention in cauda equine syndrome – a systematic critical review. World Neurosurgery. 12</ref> | ||
The patient however may not present with clear red flags and physiotherapy intervention may continue. | The patient however may not present with clear red flags and physiotherapy intervention may continue. | ||
== Referral Back to the GP == | == Referral Back to the GP == | ||
| Line 246: | Line 245: | ||
== Further Specialist Medical Opinion == | == Further Specialist Medical Opinion == | ||
As well as a referral back to the GP, further specialist medical opinions can be gained<ref name="carv">Carvalho, A. Red Alert: How useful are flags for identifying the origins of pain and barriers to rehabilitation? Frontline. 13 (17). 2007</ref>. This may be referall onto a specialist spinal clinic. | As well as a referral back to the GP, further specialist medical opinions can be gained<ref name="carv">Carvalho, A. Red Alert: How useful are flags for identifying the origins of pain and barriers to rehabilitation? Frontline. 13 (17). 2007</ref>. This may be referall onto a specialist spinal clinic. | ||
<ref name="carv" /> | <ref name="carv" /> | ||
== Documentation == | == Documentation == | ||
| Line 257: | Line 257: | ||
= Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) = | = Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) = | ||
<div class="researchbox"> | <div class="researchbox"> | ||
<rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | <rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | ||
</div> | </div> | ||
= References = | = References = | ||
Revision as of 12:39, 15 January 2014
Original Editor - Anna Butler, Fiona Stohrer and Kat Moon .... as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - Katherine Moon, Fiona Stohrer, Anna Butler, Admin, Kim Jackson, Rachael Lowe, Naomi O'Reilly, WikiSysop, Claire Knott, Jess Bell, Gunilla Buitendag, Tarina van der Stockt, Simisola Ajeyalemi, Shaimaa Eldib and 127.0.0.1
What are red flags?
[edit | edit source]
Part of the UK guidelines for an assessment of lower back pain is to rule out serious pathology and identify red flags (Koes et al. 2010). Red flags are features from a patients subjective and objective assessment which is thought to put them at a higher risk of serious pathology and warrant referral for further diagnostic testing (Henschke et al. 2013). Red flags often highlight non-mechanical conditions or pathologies of visceral origin (E. Mulligan). Red flags can be contraindications to many Physiotherapy treatments.
Although red flags have a valid role to play in assessment and diagnosis they should also be used with caution. Some guidelines contain no information on diagnostic accuracy for individual red flags, so it is the responsibility of individual practitioners to make themselves aware of these. Other guidelines even recommend immediate referral to imaging if any red flag is present, which could lead to many unnecessary referrals if clinicians did not clinically reason their referral (Downie et al. 2013).
History of red flags[edit | edit source]
The role of Physiotherapists in identifying red flags has changed as Physiotherapists increasingly become a patients first point of contact with a healthcare professional. In McKenzies 1990 book he states that “the patient once screened by the medical practitioner, should have any unsuitable pathologies excluded.” Within today’s healthcare system patients may not have even been seen by a doctor before they present to a Physiotherapist as there is more scope for self referral and private clinics. The term ‘red flag’ was first used by the Clinical Standards Advisory Group in 1994. However, similar high risk markers date back to Mennell in 1952 and Cyriax in 1982 (Greenhalgh and Selfe 2006).
Red Herrings[edit | edit source]
Red Herrings are “any misleading biomedical or psychosocial factors that will deflect the course of accurate clinical reasoning” (Greenhalgh). When assessing lower back pain red herrings can mislead a clinician into misdiagnosis resulting in a delay in appropriate treatment for the pathology causing the lower back pain.
Spinal Masqueraders
[edit | edit source]
Spinal masqueraders are conditions which present as lower back pain but are actually caused by non-mechanical referred pain from a structure not part of the spine.
Spinal masqueraders are examples of where red herrings can sometimes lead to misdiagnosis. Patients will present with lower back pain but the source is not a mechanical structure (Walcott et al 2011). Although the percentage of patients seen by Physiotherapists with these conditions is small it is important to be able to recognise the red flags that could point towards these conditions.
Some of the sources of visceral pain include:
• Inflammation - eg appendicitis
• Distention - eg bowel obstruction
• Ischemia - eg a tumour blocking blood supply
The blood supply to internal organs is in close proximity to the sympathetic nerve system so changes to the blood supply from ischemia, distention of inflammation can directly affect the nerve innervation (Eveliegh 2013).
This diagram depicts the most commong referral patterns for visceral pathologies.
(Eveliegh 2013)
Epidemiology of red flags[edit | edit source]
It is hard to get an exact picture of the epidemiology of red flags as it depends heavily on the level of documentation by clinicians. One study by Leerar et al, 2007 suggested that “the documentation of red flags was comprehensive in some areas (age over 50, bladder dysfunction, history of cancer, immune suppression, night pain, history of trauma, saddle anaesthesia and lower extremity neurological deficit) but lacking in others (weight loss, recent infection, and fever/chills)”.
This model was suggested by the 1994 Clinical Standards Advisory Group for the proportion of serious spinal pathologies.
This table shows further breakdown of the conditions lower back pain patients present with.
Figures in brackets indicate estimated percentages of patients with these conditions among all adult patients with signs and symptoms of low back pain. Percentages may vary substantially according to demographic. Data obtained from Deyo et al
(Jarvik et al. 2002)
Subjective History - Red Flags[edit | edit source]
The most important indicators for increasing the probability of underlying systemic disease are:
- age
- history of cancer
- unexplained weight loss
- duration of pain
- responsiveness to previous therapy
(Deyo 1992)
Age[edit | edit source]
In the UK age above 55 years is considered a red flag (CSAG 1994), this is because above this age, particularly above 65, the chances of being diagnosed with many serious pathologies, such as cancers, increase (Greenhalgh and Selfe).
History of cancer
[edit | edit source]
A patient history of cancer and also family history of cancer should be established, particularly in a first degree relative, such as a parent or sibling (Greenhalgh and Selfe). The most common forms of metastatic cancer are: breast, lung and prostate (Jarvik 2002).
The most common warning signs of cancer are:
- Change in bowel or bladder habits
- Sores that do not heal
- Unusual bleeding or discharge
- Thickening or lump in breast elsewhere
- Indigestion or difficulty swallowing
- Obvious change in wart or mole
- Nagging cough or hoarseness
(Greenhalgh and Selfe)
Unexplained weight loss[edit | edit source]
This should depend on a patients previous weight and it is sometimes more useful to consider percentage weight loss. A weight loss of of 5% of more within a 4 week period is a rough indicator of when unexplained weight loss should cause alarm (Greenhalgh and Selfe).
Pain[edit | edit source]
Constaint pain - this needs to be true constant pain that does not vary within a 24 hour period
Thoracic pain - the thoracic region is the most common region for metatases
Severe night pain - this can be linked to be objective history if the patients symptoms are brought on when they are lying down or non weight bearing
Abdominal pain and changed bowel habits but with no change of medication - a change is bowel habits can be a red flag for cauda equina
(Greenhalgh and Selfe)
Responsiveness to previous therapy[edit | edit source]
This can also be considered a yellow flag and should be taken with caution as many patients suffer episodic lower back pain. However, patients who initially respond to treatment and then relapse may be a cause for concern (Greenhalgh and Selfe).
Other
[edit | edit source]
- Systemically unwell
- Bilateral pins and needles
- Trauma - fall from height, road traffic accident or combat
- Past medical history of tuberculosis or osteoporosis
- Smoking -has adverse affects on circulation, therefore decreasing the nutritional supply getting to the intervertebral disk and vertebrae. Over time this leads to degeneration of these structures and therefore instability which can cause lower back pain. It has also been suggested that regular coughing, which if often associated with smoking, can also lead to increased mechanical stress on the spine
- Cauda Equina symptoms: urinary retention, faecal incontinence, unilateral or bilateral sciatica, reduced straight leg raise and saddle anaesthesia
(Greenhalgh and Selfe)
Objective History [edit | edit source]
The subjective assessment will provide the therapist with the majority of the information needed to clarify cause of symptoms [1]
Physical Appearance[edit | edit source]
The therapist should determine if the patient is unwell objectively however this is a very subjective concept. The following signs may indicate that the patient has a systemic serious pathology[2].
• Pallor/flushing
• Sweating
• Altered complexion: sallow/jaundiced
• Tremor/shaking
• Tired
• Dishevelled/unkempt
• Halitosis
• Poorly fitting clothes
Observation[edit | edit source]
Deformity of the spine[edit | edit source]
Deformity of the spine with muscle spasm and severe limitation of movement are suggested to be key indicators of serious spinal pathology[2]. A rapid onset of a scoliosis may be indicative of an osteoma or osteoblastoma however this may not be apparant in standing. Physiological movements are often required to detemine a rapid onset scoliosis
Some spinal tumors can be large enough to be seen or felt. Swelling and tenderness may be the first sign of a tumour[2]. It is also common for spinal tumours to limit physiological movements.
Muscle Spasm[edit | edit source]
This is suggested to be synonymous with low back pain and is therefore difficult to determine if it is associated with a red flag pathology. If a serious spinal pathology is present, the muscle spasm may be severe enough to be a cause of scoliosis in the spine[2]. The correlation between muscle spasm, pain and other objective clinical measurements however, are poorly supported by strong evidence[2].
Neurological Assessment[edit | edit source]
Patients who report neurological signs in the subjective assessment require a neurological assessment[3]. A neurological deficit is rarely the first presenting symptom in a patient with serious spinal pathology however 70% of patients will have a neurological deficit at the time of diagnosis [2]
The dermatomes, myotomes and reflexes should be examined. The upper motor neurone should also be examined via extensor plantar reflex (Babinski), clonus and hoffmans. If brisk, it may indicate a upper motor neurone pathlogy[2].
Diagnostic Tests[edit | edit source]
What is differential diagnosis?
A systematic process in which tools such as clinical tests are used to identify the proper diagnosis from a competing set of possible diagnoses. (Whiting et al, 2008)
For a clinical test to be the best test?
• Reliable
• Low Cost
• Validated findings
• High diagnostic Accuracy = SPECIFICITY AND SENSITIVITY
SPECIFICITY
Is the percentage of people who test negative for a specific disease among a group of people who do not have the disease (Sackett et al 2000)
SENSITIVITY
Percentage of people who test positive for a specific disease among a group of people who have the disease (Sackett et al, 2000).
Likelihood ratio = The Likelihood Ratio (LR) is the likelihood that a given test result would be expected in a patient with the target disorder compared to the likelihood that that same result would be expected in a patient without the target disorder. (http://www.cebm.net/?o=1158)
http://www.physio-pedia.com/Test_Diagnostics
High sensitivity and LOW LR = RULE OUT people who don’t have the disease
High specificity and HIGH LR = RULE IN people who have the disease
Percussion test
Tests : Compression fractures
The examiner stands behind the patient. The patient stands facing a mirror so that the examiner can gauge their reaction. The entire length of the spine is examined using firm, closed-fist percussion.
Positive = when the patient complains of a sharp, sudden pain.
Table 1. A table to show sensitivity, specificity and likelihood ratios of the Percussion diagnostic test for compression fracture. (Langdon et al 2009)
Clinical Reasoning[edit | edit source]
Clinical Reasoning is integral to physiotherapy practice. As a concept, clinical reasoning is quite a simple one however in practice, it is difficult and fraught with errors. The aim of clinical reasoning is to prevent misdirection [4]The way a therapsit clinically reasons their finidings can strongly influence how the case is interpreted. This has implications as to how the clinician views the red flags and gives weight to any red herrings presented therein [5]
The most common form of clinical reasoning within the physiotherapy profession is hypothetico-deductive reasoning [6]Within hypothetico-deductive reasoning, the clinician gains initial clues in regards to the patients problem (from the subjective assessment) which forms initial hypotheses in the therapists mind. Further data is collected in the objective assessment which may confirm or negate the hypotheses. Continual hypothesis generation may occur during management and reassessment [7]
Reflection after the initial assessment and also after the subsequent sessions will help the therapist to recognise mechanical and non-mecahnical patterns and their clinical reasoning process will improve [4][8]
Process of Clinical Reasoning[edit | edit source]
Clinical reasoning should begin as soon as the therapist meets the patient as their behaviour can inform the therapists clinical reasoning [2]There should be ongoing data collection which should not stop at the end of the assessment to aid this process. A hyptothetico-deductive model of clinical reasoning can be seen in Figure 1.
Figure 1: A Hypothetico-deductive model of Clinical Reasoning[4]
The therapist may be able to ascertain quickly that something is wrong with the patient due to the subjective and objective assessment along wither their subsequent clinical reasoning. The data gathered over sessions should be collated to best inform the therapist. This will contribute to the therapists evolving concept of the patients’ problem[2][4].
Pattern Recognition[edit | edit source]
Pattern recognition is an important part of clinical reasoning however this will be limited in students and newly qualified physiotherapists [4][6]
Knowledge is also an important consideration. The newly qualified therapist is expected to have many more potential hypotheses in comparison to a experienced therapist [4]. There is suggested to be differences in novice and expert therapists in the process of clinical reasoning[6]. Although largely similar, novice physiotherapists have to go through a longer process of clinical reasoning compared to expert therapists due to lack of knowledge in comparison; and less experience in pattern recognition. Figure 2 demonstrates the clinical reasoning process of expert therapists (with at least 3 years of experience) and novice therapists (with under three years’ experience or students)[6].
Figure 2: Difference in clinical reasoning between expert and novice therapists [6].
Patient involvement in the clinical reasoning process[edit | edit source]
The patient should be an integral part of the clinical reasoning process as this can help the clinician to form hypotheses and lead towards the review of the outcome post physiotherapy intervention [4](See Figure 3).
Figure 3: Patient involvement in the clinical reasoning process [4]
Errors in Clinical Reasoning[edit | edit source]
Patients’ inappropriate misattribution of insidious symptoms to a traumatic event is common and can be misleading[5]. Clinical reasoning is only as good as the information on which it is based indicating the importance of thorough questioning in the subjective assessment [8]
The three types of errors that can occur in clinical reasoning include:
- Faulty perception or elicitation of cues
- Incomplete factual knowledge
- Misapplication of known facts to a specific problem
Red Herrings[edit | edit source]
Within the clinical reasoning process, the therapist should determine if there are logical inferences in regards to the information they are recieving from the patient [5]. The therapist should not be reassured by previous investigations being reported on as normal [8]. In the early stages, serious spinal pathology is difficult to detect and weight loss will not always be evident in these early stages [9]
Management of red flags[edit | edit source]
Students Responsibility[edit | edit source]
Whilst on a clinical placement, it is the students’ responsibility to inform the clinical educator if they find a red flag and document appropriately in the clinical notes. This will allow the educator to perform the assessment again if required.
Onward referral to Accident and Emergency[edit | edit source]
In some cases the red flags may be obvious. If serious enough, the therapist may refer onto Accident and Emergency. This may be the case in cauda equina syndrome for further surgical opinion [10]
The patient however may not present with clear red flags and physiotherapy intervention may continue.
Referral Back to the GP[edit | edit source]
Failure to improve after one month is a red flag and the patient can be referred back to the GP for continued management and further diagnostic tests as required [2]
Further Specialist Medical Opinion[edit | edit source]
As well as a referral back to the GP, further specialist medical opinions can be gained[11]. This may be referall onto a specialist spinal clinic.
Documentation[edit | edit source]
After onward referral red flags must be acknowledged in the notes as this will indicate contraindication to physiotherapy. Physiotherapist documentation of red flags has been suggested to be documented 98% of the time for the main red flags:
• Age over 50
• Bladder dysfunction
• History of cancer
• Immunosuppression
• Night pain
• History of trauma
• Saddle anaesthesia
• Lower extremity neurological deficit
Red flags that were not documented routinely included[11]:
• Weight loss
• Recent infection
• Fever/chills
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Eveleigh, C. Red Flags and Spinal Masquereders. [online]. Available at : www.nspine.co.uk/.../09-nspine2013-red-flags-masqueraders.ppt. Accessed 13/01/14. 2013.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Greenhalgh, S. and Selfe, J. Red Flags: A guide to identifying serious pathology of the spine. Churchill Livingstone: Elsevier. 2006.
- ↑ Petty, N. J. and Moore, A. P. Neuromuscular examination and assessment: a handbook for therapists. Edingburgh: Churchill Livingstone. 2001.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Jones, M. Clinical reasoning and pain. Manual Therapy. 1, pp: 17 – 24. 1995.
- ↑ 5.0 5.1 5.2 Greenhalgh, S. and Selfe, J. Margaret: a tragic case of spinal Red Flags and Red Herrings. Physiotherapy. 90, pp: 73 – 76. 2004
- ↑ 6.0 6.1 6.2 6.3 6.4 Doody, C. and McAteer, M. Clinical reasoning of expert and novice physiotherapists in an outpatient orthopaedic setting. Physiotherapy. 88 (5), pp: 258 – 268. 2002.
- ↑ Edwards, I., Jones, M., Carr, J., Braunack-Mayer, A. and Jensen, G. M. Clinical Reasoning Strategies in Physical Therapy. Physical Therapy. 84 (4), pp: 312 - 335. 2004
- ↑ 8.0 8.1 8.2 Greenhalgh, S. Red Flags, and clinical Presentation Mapping. [online]. Available at: https://www.macpweb.org/home/index.php?m=file&f=873. Accessed 21/12/13. 2008
- ↑ Greenhalgh, S. and Selfe, J. Malignant Myeloma of the spine: Case Report. Physiotherapy. 89 (8), pp: 486 – 488.
- ↑ Chau, A. M. T., Xu, L. L., Pelzer, N. R. and Gragnaniello, C. (2013). Timing of surgical intervention in cauda equine syndrome – a systematic critical review. World Neurosurgery. 12
- ↑ 11.0 11.1 11.2 Carvalho, A. Red Alert: How useful are flags for identifying the origins of pain and barriers to rehabilitation? Frontline. 13 (17). 2007