Scleroderma
Original Editors - Amanda Schoenfelder & Katie Williams from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
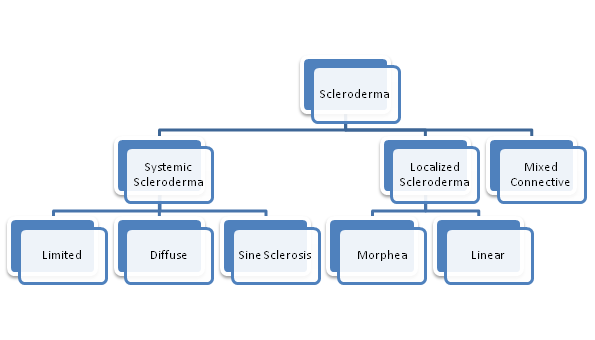
Scleroderma is a connective tissue disease that involves changes in the skin, blood vessels, muscles, and internal organs.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It is a chronic, progressive autoimmune disorder where inflammation and the overproduction of collagen accumulate in the body.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title There are two main types of Scleroderma- Systemic and Localized.
Systemic Scleroderma may affect multiple systems such as the integumentary, cardiopulmonary, vascular, gastrointestinal, genitourinary, or musculoskeletal. There are three forms of Systemic Scleroderma.
- With Diffuse Scleroderma skin thickening occurs more rapidly and involves more skin areas than in limited. In addition, people with diffuse scleroderma have a higher risk of developing “sclerosis” or fibrous hardening of the internal organs.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Sine Scleroderma involves organ fibrosis with no skin involvement.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - With Limited Scleroderma (CREST syndrome) skin thickening is less widespread, typically confined to the fingers, hands and face, and develops slowly over years. Internal problems occur, but they are less frequent and tend to be less severe than in diffuse scleroderma.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Localized Scleroderma usually affects only the skin on the hands and face. It develops slowly, and rarely, if ever, spreads throughout the body or causes serious complications.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title There are two types of Localized Scleroderma.
- Morphea is characterized by waxy patches on the skin of varying sizes, shapes and color. The skin under the patches may thicken. The patches may enlarge or shrink, and often may disappear spontaneously.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Linear Scleroderma starts as a streak or line of hardened, waxy skin on an arm or leg or on thehead and neck. Linear scleroderma tends to involve deeper layers of the skin as well as the surface layers, and sometimes affects the motion of the joints, which lie underneath.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Linear scleroderma often appears mostly on one side of the body. Cite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title
Mixed Connective Disease is when Scleroderma is diagnosed when another disease, such as systemic lupus erythematosus and polymyositis, has been previously diagnosed.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Prevalence[edit | edit source]
It’s estimated that about 300,000 Americans have scleroderma. About one third of those people have the systemic form of scleroderma. Localized scleroderma is more common in children, whereas systemic scleroderma is more common in adults. Overall, female patients outnumber male patients about 4-to-1. Although scleroderma is not directly inherited, some scientists feel there is a slight predisposition to it in families with a history of rheumatic diseases. However, scleroderma can develop in every age group from infants to the elderly, but its onset is most frequent between the ages of 25 to 55. Race and ethnic background, may influence the risk of getting scleroderma, the age of onset, and the pattern or severity of internal organ involvement.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleChoctaw Native Americans in Oklahoma are at least 20 times as likely as is the general population to develop systemic scleroderma. This increased risk doesn't apply to Choctaws living in Mississippi. African-Americans are more at risk to develop systemic scleroderma and are more likely to develop severe lung complications.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
Associated Co-morbidities[edit | edit source]
add text here
Medications
[edit | edit source]
Medicines used to treat scleroderma include: [1]
• Anti-inflammatory medicines such as corticosteroids
• Immune-suppressing medications such as methotrexate and Cytoxan
• Nonsteroidal anti-inflammatory drugs (NSAIDs)
Scleroderma can affect many different organs and organ systems. Additional medications are based on the symptoms that the individual experiences.
Examples of other treatments for specific symptoms include:[1][2]
• Medicines for heartburn or swallowing problems
• Blood pressure medications (particularly ACE inhibitors) for high blood pressure or kidney problems
• Light therapy to relieve skin thickening
• Medicines to improve breathing
• Medications to treat Raynaud's phenomenon
• Intestinal dysfunction
• Medicines to increase saliva secretion in the mouth to reduce effects of Sjogren’s Syndrome
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
add text here
Etiology/Causes Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
The cause of scleroderma is unknown, but it cannot be transmitted from person to person. Several factors that may increase a person's risk of getting scleroderma include:
Abnormal immune or inflammatory activity: In scleroderma, the immune system is thought to stimulate cells called fibroblasts so they produce too much collagen. People who already have rheumatic or autoimmune disorders are at increased risk due to previous abnormal autoimmune activity.
Genetic makeup: Although genes seem to put certain people at risk for scleroderma and play a role in its course, the disease is not passed from parent to child like some genetic diseases. Research indicates that there is a susceptibility gene, which raises the likelihood of getting scleroderma, but by itself does not cause the disease. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Environmental triggers: Research suggests that exposure to some environmental factors may trigger scleroderma-like disease in people who are genetically predisposed to it. Suspected triggers include viral infections, certain adhesive and coating materials, and organic solvents such as vinyl chloride or trichloroethylene. But no environmental agent has been shown to cause scleroderma. In the past, some people believed that silicone breast implants might have been a factor in developing connective tissue diseases such as scleroderma. But several studies have not shown evidence of a connection.
Hormones: Women develop scleroderma more often than men. Scientists suspect that hormonal differences between women and men play a part in the disease. However, the role of estrogen or other female hormones has not been proven.
Systemic Involvement[edit | edit source]
IntegumentaryCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Swelling in fingers and hands
- Sclerodactyly: thickened patches of skin, particularly on the fingers or tight skin around the hands, face or mouth.
- Skin can appear shiny because it's so tight, and movement of the affected area may be restricted.
- Ulcers: restricted blood flow permanently damages the tissue at the fingertips, causing pits or skin sores. In some cases, gangrene and amputation may follow.
GICite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- GERD: valve dysfunction and narrowing of esophagus
- Swallowing difficulty from narrowing esophagus and decreased saliva production
- Diarrhea: decrease in peristalsis causing increase in bacterial growth or malabsorbtion
- Constipation: weak or scarred colon muscles causing decreased peristalsis
PulmonaryCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Fibrosis: Build-up of collagen thickens lung tissue making the transport of oxygen into the bloodstream more difficult.
- Pulmonary arterial hypertension (PAH): state of increased resistance to blood flow through the lungs, can result from damage to blood vessels
- Respiratory muscle weakness: from fibrosis may decrease lung function
Cardiac
- Heart Failure: from increased pressure secondary to Pulmonary HypertensionCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Pericarditis
- ArrythmiasCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
VascularCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Raynaud’s: blood vessels constrict or narrow in response to cold or emotional upset and stress. The resulting disturbance in blood circulation causes a series of color changes in the skin: white, blanched or pale, when circulation is reduced; blue as the affected part loses oxygen from decreased blood flow; and then red or flushed as blood flow returns and the part re-warms. Sensations such as tingling, numbness and coldness may be felt. In the “red” stage, a feeling of warmth, burning or throbbing may be noted.
EndocrineCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Sjögren Syndrome: is characterized by a decrease in secretions of the tear glands and the salivary glands. The unusual dryness of the eyes resulting from this condition can lead to serious irritation and inflammation. Excessive dryness of the mouth may lead to difficulties in swallowing and speaking, a pronounced increase in tooth decay and cavities, and a reduced sense of taste. May also involve the vagina and other areas of the body.
GUCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Hypertension: when the kidneys are affected, you can develop an elevated blood pressure and an increased level of protein in your urine.
- Renal Crisis: which involves a sudden increase in blood pressure and rapid kidney failure.
- Sexual Function: Erectile dysfunction and decrease of sexual lubrication
DentalCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Tooth Decay: decreased saliva and increased acid from GERD
Medical Management (current best evidence) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
Currently, there is no treatment that controls or stops the underlying problem—the overproduction of collagen—in all forms of scleroderma. Treatment and management focus on relieving symptoms and limiting damage, which is dependent upon the problems each individual experiences.
Several different specialists may be involved in the care of one person since scleroderma can affect many different organs and organ systems. Typically, care will be managed by a rheumatologist, who may refer the patient to other specialists, depending on the specific problems they are having.
These specialists can include:
• Dermatologist for the treatment of skin symptoms
• Nephrologist for kidney complications
• Cardiologist for heart complications
• Gastroenterologist for problems of the digestive tract
• Pulmonary specialist for lung involvement
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy can be very beneficial in the treatment of scleroderma. Physical therapists can design a program of regular stretching and gentle exercise to help:
• Manage pain
• Improve strength
• Improve/maintain mobility
• Minimize joint contractures
• Improve circulation
• Enhance/maintain performance of activities of daily living in order to encourage independence
In addition, an appropriate level of exercise can promote relaxation and a sense of well-being. [3]
Alternative/Holistic Management (current best evidence)[edit | edit source]
Yoga, meditation, and biofeedback can help manage stress and anxiety caused by the frustrations and complications of scleroderma.
Some nutritional supplements can improve or worsen the symptoms caused by scleroderma. [3]
File:Table nutrition complex pt.png
Differential Diagnosis Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
A number of other diseases have symptoms similar to those seen in scleroderma.
Some of the most common include:
Eosinophilic fasciitis (EF): This disease involves the fascia, the thin connective tissue around the muscles, particularly those of the forearms, arms, legs, and trunk. EF causes the muscles to become encased in collagen, the fibrous protein that makes up tissue such as the skin and tendons. Contractures may develop, sometimes causing disfigurement and problems with joint motion and function. EF may begin after hard physical exertion. The disease usually fades away after several years, but people sometimes have relapses. Although the upper layers of the skin are not thickened in EF, the thickened fascia may cause the skin to look somewhat like the tight, hard skin of scleroderma. A skin biopsy easily distinguishes between the two diseases.
Skin thickening on the fingers and hands: This also appears with diabetes, mycosis fungoides, amyloidosis, and adult celiac disease. It can also result from hand trauma.
Generalized scleroderma-like skin thickening: This may occur with scleromyxedema, graft-versus-host disease, porphyria cutanea tarda, and human adjuvant disease.
Internal organ damage: Similar to that seen in systemic sclerosis, this may instead be related to primary pulmonary hypertension, idiopathic pulmonary fibrosis, or collagenous colitis.
Raynaud’s phenomenon: This condition also appears with atherosclerosis or systemic lupus erythematosus or in the absence of underlying disease.
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 Teitel A D. Medline Plus [internet]. Bethesda (MD): U.S. National Library of Medicine; c1997-2013 [updated 2013 Feb 27; cited 2013 Mar 6]. Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000429.htm
- ↑ Scleroderma Research Foundation- Current Treatments [internet]. San Francisco: Scleroderma Research Foundation; c2013 [cited 2013 Mar 6]. Available from: http://www.srfcure.org/for-patients/current-treatments
- ↑ 3.0 3.1 Scleroderma Research Foundation- Tips for Living with Scleroderma [internet]. San Francisco: Scleroderma Research Foundation; c2013 [cited 2013 Mar 6]. Available from: http://www.srfcure.org/for-patients/tips-for-living