Surgery and General Anaesthetic: Difference between revisions
Erin Froude (talk | contribs) No edit summary |
Erin Froude (talk | contribs) No edit summary |
||
| Line 49: | Line 49: | ||
<u>'''Post-operative Physiotherapy'''</u> | <u>'''Post-operative Physiotherapy'''</u> | ||
The main problems found on assessment of a patient who has had major surgical procedure is reduced lung volume<ref name="Pryor" />. This could result in impaired gas exchange and airway clearance<ref name="Pryor" />, | The main problems found on assessment of a patient who has had major surgical procedure is reduced lung volume<ref name="Pryor" />. This could result in impaired gas exchange and airway clearance<ref name="Pryor" />. Other cardiovascular and respiratory effects are reduction in functional residual capacity, PaO2, VO2Max, cardiac output and stroke volume, and an increase in HR<ref name="Pryor" />. Thus the aim of the physiotherapist is to try and improve these problems. From the post-operative assessment a treatment plan will be developed.<br> | ||
*'''Mobilisation -''' will improve lung volume, decrease their stay in the hospital and will make it easier for the patient to remove secretions. Examples: walking around their bed or along the corridor. | *'''Mobilisation -''' important component that will improve lung volume, decrease their stay in the hospital and will make it easier for the patient to remove secretions. Examples: walking around their bed or along the corridor. | ||
*'''Positioning - ''' | *'''Positioning - ''' | ||
*'''deep breathing exercises''' - | *'''deep breathing exercises''' - include thoracic expansion exercises, diaphragmatic breathing & maximal inspiration<ref name="Pryor" />. Can help reinflate the collapsed lung<ref name="Pryor" />. | ||
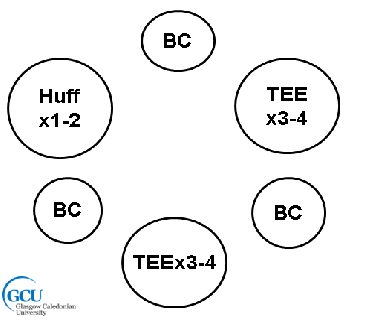
*Appropriate airway clearance techniques can be implemented, such as, active cycle of breathing techniques (ACBT) and autogenic drainage (AD)<ref name="Hough" />. | *Appropriate airway clearance techniques can be implemented, such as, active cycle of breathing techniques (ACBT) and autogenic drainage (AD)<ref name="Hough" />. With surgery, more emphasis is on the deep breathing component rather than the forced expiratory manoeuvres to avoid pain and discomfort for the patient<ref name="Pryor" />. | ||
[[Image:ACBT 2.png|center]] | [[Image:ACBT 2.png|center]] | ||
*'''Continuous Positive Airway Pressure (CPAP)''' - assist with hypoxaemia | *'''Continuous Positive Airway Pressure (CPAP)''' - assist with hypoxaemia, reduce RR & minute ventilation and also through to increase vital capactiy<ref name="Pryor" />. | ||
*'''Intermittent Positive Pressure''' - help improve lung volume and sputum retention | *'''Intermittent Positive Pressure''' - help improve lung volume and sputum retention | ||
*'''Incentive spirometry -''' used to stimulate the patient to perform deep breathing exercises<ref name="Pryor" />.<br> | |||
<br> | <br> | ||
Revision as of 10:20, 3 June 2015
Original Editors - Students from Glasgow Caledonian University's Cardiorespiratory Therapeutics Project.
Top Contributors - Bo Lian Ho Sing, Lucinda hampton, Erin Froude, Michelle Lee, Chris Seenan, Kim Jackson, 127.0.0.1, Admin, George Prudden, Adam Vallely Farrell and Karen Wilson
Definition/Description[edit | edit source]
Definition of the disease or condition
Epidemiology[edit | edit source]
Background epidemiology to the disease or condition (to include prevalence and incidence as appropriate from a UK or Scottish perspective. (You may want to also look at the disease prevalence across different social economic groups).
Pathophysiology[edit | edit source]
The causes of the disease or condition, current thinking and research activity as appropriate
Investigations[edit | edit source]
Prior to surgery, the patient must undergo a pre-operative assessment. This involves seeing a nurse or doctor who will ask the patient questions about their health, medical history, advise the patient on what to do before the surgery and where to report on the day [1]. They may also carry out some tests, such as, blood pressure (BP) and respiratory rate (RR) so that when assessing the patient after surgery, they have baseline measurements to compare against. The pre-assessment willl highlight any contra-indications that could postpone the surgery procedure [1].
Investigations used for monitoring the patient after surgery could be chest x-rays, BP, HR, RR, ABG's and other observations noted. Surgery and general anaesthetic can lead to postoperative pulmonary complications so it is crucial that patients are monitored. Anaesthesia can have an effect on lung mechanics, lung defences and gas exchange, therefore a chest x-ray will help identify if there is a lung collapse or any consolidation[2]. A CT scan can also identify consolidation and atelectasis[3]. Postoperative hypoxaemia may be present, thus an analysis of an arterial blood sample allows a physiotherapist to monitor deterioration and identify respiratory failure[4]. Another possible effect of anaesthesia is an alteration in mucociliary clearance. This can be monitored using auscultation to determine where the secretions are (broad). Blood pressure can help determine cardiovascular status of the patient[4]. Other observations could be heart rate, respiratory rate and temperature as these can all be altered if the patient has an infection[3].
Clinical Manifestations[edit | edit source]
Clinical manifestations (the signs and symptoms your patient may well present to you on an examination) ensure you relate this back to the underlying pathophysiology.
Physiotherapy and Other Management[edit | edit source]
Pre-operative Physiotherapy[2]
Trying to see a patient before surgery can be beneficial, however, it can also be difficult if its an emergency or could be due to time constrictions with the patients, particularly within the NHS.
A pre-operative assessment may include:
- an explanation of the role of the physiotherapist within the team
- the possible risks of surgery and the effects of general aneasthesia
- what will happen after the surgery
Some of these benefits to seeing a physiotherapist pre-operatively are:
- may reduce the patient's anxiety levels
- confidence could be gained
- the patient will have more knowledge on what is entailed before,during and after the surgery and how they may feel afterwards
- can prevent the risk of developing post-operative pulmonary complications
Post-operative Physiotherapy
The main problems found on assessment of a patient who has had major surgical procedure is reduced lung volume[2]. This could result in impaired gas exchange and airway clearance[2]. Other cardiovascular and respiratory effects are reduction in functional residual capacity, PaO2, VO2Max, cardiac output and stroke volume, and an increase in HR[2]. Thus the aim of the physiotherapist is to try and improve these problems. From the post-operative assessment a treatment plan will be developed.
- Mobilisation - important component that will improve lung volume, decrease their stay in the hospital and will make it easier for the patient to remove secretions. Examples: walking around their bed or along the corridor.
- Positioning -
- deep breathing exercises - include thoracic expansion exercises, diaphragmatic breathing & maximal inspiration[2]. Can help reinflate the collapsed lung[2].
- Appropriate airway clearance techniques can be implemented, such as, active cycle of breathing techniques (ACBT) and autogenic drainage (AD)[3]. With surgery, more emphasis is on the deep breathing component rather than the forced expiratory manoeuvres to avoid pain and discomfort for the patient[2].
- Continuous Positive Airway Pressure (CPAP) - assist with hypoxaemia, reduce RR & minute ventilation and also through to increase vital capactiy[2].
- Intermittent Positive Pressure - help improve lung volume and sputum retention
- Incentive spirometry - used to stimulate the patient to perform deep breathing exercises[2].
Other health professionals will be treating your patient. What is their input?
Prevention[edit | edit source]
Brief consideration of how this pathology could be prevented and the physiotherapy role in health promotion in relation to prevention of disease or disease progression.
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 NHS. Going into hospital. http://www.nhs.uk/NHSEngland/AboutNHSservices/NHShospitals/Pages/going-into-hospital.aspx#assessment (accessed 29th May 2015).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Denehy, L. Surgery for adults. In: Pryor, J.A, Prasad, S.A (eds.) Physiotherapy for Respiratory and Cardiac Problems. United Kingdom: Churchill livingstone; 2008. p. 397-439.
- ↑ 3.0 3.1 3.2 Hough, A. Physiotherapy in Respiratory and Cardiac Care - an evidence-based approach. (4th ed.). Singapore: Andrew Ashwin; 2014.
- ↑ 4.0 4.1 Broad, M. Cardiorespiratory Assessment of the Adult Patient: a Clinician's Guide. Edinburgh: Churchill Livingstone; 2012