Tibialis posterior rupture: Difference between revisions
Tim Hendrikx (talk | contribs) No edit summary |
No edit summary |
||
| (14 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Tim Hendrikx|Tim Hendrikx]] from [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
''' | </div> | ||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
Whenever the tibialis posterior muscle contracts or is stretched, tension is placed through the tibialis posterior tendon. If this tension is excessive due to too much force or repetition, damage to the tibialis posterior tendon may occur. This can range from minor tearing of the tendon with subsequent inflammation to a complete tibialis posterior tendon rupture. Early diagnosis and surgical repair will restore full normal function. <ref name="William M. Geideman" | Whenever the tibialis posterior muscle contracts or is stretched, tension is placed through the tibialis posterior tendon. If this tension is excessive due to too much force or repetition, damage to the tibialis posterior tendon may occur. This can range from minor tearing of the tendon with subsequent inflammation to a complete tibialis posterior tendon rupture. Early diagnosis and surgical repair will restore full normal function. <ref name="William M. Geideman" /> | ||
A rupture of the posterior tibial tendon can be easily missed because the symptoms of this injury resemble the symptoms of a normal ankle sprain. Some physicians may feel that posterior tibial tendon rupture is a rare condition, one that they have never seen. | |||
== [[Tibialis Posterior|Clinically Relevant Anatomy]] == | |||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Posterior tibialis tendon ruptures occur predominantly in the late middle-aged population (average age 57 years). For posterior tibialis dysfunction, the patient is typically a female over the age of 40 who exhibits ligamentous laxity in multiple joints and has an occupation that requires extended periods of standing. They usually do not recall any acute traumatic event. There is another subset of the populations in which posterior tibial tendon insufficiency occurs and that consists of the 20- to 40-year old athletes. They usually recall a traumatic event, usually a direct blow to the medial malleolus. Or, they present with years of involvement in athletics with a pronated foot.<ref name="William M. Geideman"> | Posterior tibialis tendon ruptures occur predominantly in the late middle-aged population (average age 57 years). For posterior tibialis dysfunction, the patient is typically a female over the age of 40 who exhibits ligamentous laxity in multiple joints and has an occupation that requires extended periods of standing. They usually do not recall any acute traumatic event. There is another subset of the populations in which posterior tibial tendon insufficiency occurs and that consists of the 20- to 40-year old athletes. They usually recall a traumatic event, usually a direct blow to the medial malleolus. Or, they present with years of involvement in athletics with a pronated foot.<ref name="William M. Geideman">Geideman WM, Johnson JE. Posterior Tibial Tendon Dysfunction. Journal of Orthopedic & Sports Physical Therapy. 2000; 30(2): 68-77</ref> <br> | ||
== Characteristics/Clinical Presentation<ref name="William M. Geideman" /> == | == Characteristics/Clinical Presentation<ref name="William M. Geideman" /> == | ||
• Swelling along the medial aspect of the foot and ankle<br>• Absence of the classical sudden severe pain of a tendon rupture<br>• Tenderness along the posterior tibialis tendon<br>• Progressive loss of longitudinal arch → pes planus and heel valgus<br>• Palpable pain between medial malleolus and navicular<br>• Pain in the plantar medial arch <br> | • Swelling along the medial aspect of the foot and ankle<br>• Absence of the classical sudden severe pain of a tendon rupture<br>• Tenderness along the posterior tibialis tendon<br>• Progressive loss of longitudinal arch → pes planus and heel valgus<br>• Palpable pain between medial malleolus and navicular<br>• Pain in the plantar medial arch <br><br> | ||
== Differential Diagnosis<ref name="Johnson KA">Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. ''Clin Orthop Relat Res''. 1989;(239):196-206.</ref> == | |||
| • Attenuation or rupture of the calcaneonavicular (spring) ligament complex<br>• Degenerative arthritis of the ankle joint with valgus talar<br>• Arthritis of the talonavicular joint<br>• Posttraumatic tarsometatarsal (Lisfranc) joint arthritis<br>• Inflammatory arthritis of the hindfoot, usually secondary to rheumatoid disease | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 46: | Line 33: | ||
== Examination == | == Examination == | ||
'''<u></u>Observation:'''<ref name="Randall E. Marcus"> | '''<u></u>Observation:'''<ref name="Randall E. Marcus">Marcus RE, Pfister ME. The enigmatic diagnosis of posterior tibialis tendon rupture. Iowa Orthop J. 1993;13:171-7. </ref> | ||
Posterior tibialis tendon rupture is strongly suspected in patients presenting a complex of findings. These include: | Posterior tibialis tendon rupture is strongly suspected in patients presenting a complex of findings. These include: | ||
| Line 52: | Line 39: | ||
• Eversion ankle injury<br>• Generalized medial ankle pain<br>• Medial ankle swelling<br>• Flexible, asymmetric pes planus and forefoot pronation<br>• Gait disturbance secondary to deformity<br>• Talonavicular sag in lateral standing radiograph | • Eversion ankle injury<br>• Generalized medial ankle pain<br>• Medial ankle swelling<br>• Flexible, asymmetric pes planus and forefoot pronation<br>• Gait disturbance secondary to deformity<br>• Talonavicular sag in lateral standing radiograph | ||
The first four findings are nondiagnostic, however, seen together they are helpful in identifying patients with posterior tibialis tendon pathology. Manual testing of the | The first four findings are nondiagnostic, however, seen together they are helpful in identifying patients with posterior tibialis tendon pathology. Manual testing of the posterior tibialis tendon should be performed in the presence of these findings to confirm the tendon's functional status. | ||
| Line 58: | Line 45: | ||
<br>'''Tests:'''<ref name="A. Foster">A. Foster, N. T. Rupture of the tibialis posterior tendon: an important differential in the assessment of ankle injuries. Ermergency Medical Journal , 2005 (4): 915-916</ref> | <br>'''Tests:'''<ref name="A. Foster">A. Foster, N. T. Rupture of the tibialis posterior tendon: an important differential in the assessment of ankle injuries. Ermergency Medical Journal , 2005 (4): 915-916</ref> | ||
• Palpation from area between malleolus | • Palpation from the area between the medial malleolus and os naviculare<br>• “Too many toes” sign secondary to an increase in forefoot abduction and heel eversion<br>• Nonfunctional posterior tibialis tendon on manual testing<br>• Motion of the ankle and subtalar joints<br>• Positive first metatarsal rise sign test<br>• Positive single-limb heel rise-test<br>• [http://www.physio-pedia.com/Ottawa_Ankle_Rules Ottawa ankle rules test] to exclude fractures within the first week after an ankle injury<br> | ||
[[Image:Too_many_toes.JPG]] | [[Image:Too_many_toes.JPG]] | ||
| Line 64: | Line 51: | ||
<br> | <br> | ||
== Medical Management <ref name="William M. Geideman" /> | == Medical Management <ref name="William M. Geideman" /> == | ||
'''Postoperative rehabilitation for tendon transfer procedure:'''<br> | '''Postoperative rehabilitation for tendon transfer procedure:'''<br> | ||
| Line 74: | Line 61: | ||
• With attenuation or rupture of the posterior tibial tendon, the medial longitudinal arch of the foot collapses and there is a relative internal rotation of the tibia and talus<br>• The subtalar joint everts, causing the heel to assume a valgus position and the foot to abduct at the talonavicular joint. A compensatory forefoot varus deformity ensues<br>• As the heel assumes an increased valgus alignment, the Achilles tendon becomes positioned lateral to the axis of rotation of the subtalar joint. Over time, the shortened position of the hindfoot results in an Achilles tendon contracture<br>• As the deformity progresses, the fibula abuts against the lateral wall of the calcaneus, causing pain in the lateral hindfoot<br> | • With attenuation or rupture of the posterior tibial tendon, the medial longitudinal arch of the foot collapses and there is a relative internal rotation of the tibia and talus<br>• The subtalar joint everts, causing the heel to assume a valgus position and the foot to abduct at the talonavicular joint. A compensatory forefoot varus deformity ensues<br>• As the heel assumes an increased valgus alignment, the Achilles tendon becomes positioned lateral to the axis of rotation of the subtalar joint. Over time, the shortened position of the hindfoot results in an Achilles tendon contracture<br>• As the deformity progresses, the fibula abuts against the lateral wall of the calcaneus, causing pain in the lateral hindfoot<br> | ||
== Physical Therapy Management <ref name="Gregory S. Kolt">Gregory S. Kolt, L. S.-M. Common sport-related injuries. In L. S.-M. Gregory S. Kolt, Physical Therapies in Sport and Exercise, Philadelphia, Elsevier 2007: 428-429</ref> | == Physical Therapy Management <ref name="Gregory S. Kolt">Gregory S. Kolt, L. S.-M. Common sport-related injuries. In L. S.-M. Gregory S. Kolt, Physical Therapies in Sport and Exercise, Philadelphia, Elsevier 2007: 428-429</ref> == | ||
Furthermore, Woods and Leach (1991) pointed out that "the key" to successful treatment is early diagnosis23.<br>(Randall E. Marcus, 1993)<br>Phase I:<br>• Ice<br>• Non steroidal anti inflammatory drugs<br>• massage | Furthermore, Woods and Leach (1991) pointed out that "the key" to successful treatment is early diagnosis23.<br>(Randall E. Marcus, 1993)<br>Phase I:<br>• Ice<br>• Non steroidal anti inflammatory drugs<br>• massage | ||
| Line 114: | Line 101: | ||
add links and reviews of high quality evidence here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | add links and reviews of high quality evidence here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | ||
== Resources | == Resources == | ||
add appropriate resources here <br> | add appropriate resources here <br> | ||
| Line 122: | Line 109: | ||
add text here <br> | add text here <br> | ||
== References == | == References == | ||
| Line 134: | Line 116: | ||
<references /> | <references /> | ||
[[Category:Vrije_Universiteit_Brussel_Project | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
Latest revision as of 17:52, 21 September 2020
Original Editors - Tim Hendrikx from Vrije Universiteit Brussel's Evidence-based Practice project Top Contributors - Tim Hendrikx, Uchechukwu Chukwuemeka, Kim Jackson, 127.0.0.1, Admin, WikiSysop and Wanda van Niekerk
Definition/Description[edit | edit source]
Whenever the tibialis posterior muscle contracts or is stretched, tension is placed through the tibialis posterior tendon. If this tension is excessive due to too much force or repetition, damage to the tibialis posterior tendon may occur. This can range from minor tearing of the tendon with subsequent inflammation to a complete tibialis posterior tendon rupture. Early diagnosis and surgical repair will restore full normal function. [1]
A rupture of the posterior tibial tendon can be easily missed because the symptoms of this injury resemble the symptoms of a normal ankle sprain. Some physicians may feel that posterior tibial tendon rupture is a rare condition, one that they have never seen.
Clinically Relevant Anatomy[edit | edit source]
Epidemiology /Etiology[edit | edit source]
Posterior tibialis tendon ruptures occur predominantly in the late middle-aged population (average age 57 years). For posterior tibialis dysfunction, the patient is typically a female over the age of 40 who exhibits ligamentous laxity in multiple joints and has an occupation that requires extended periods of standing. They usually do not recall any acute traumatic event. There is another subset of the populations in which posterior tibial tendon insufficiency occurs and that consists of the 20- to 40-year old athletes. They usually recall a traumatic event, usually a direct blow to the medial malleolus. Or, they present with years of involvement in athletics with a pronated foot.[1]
Characteristics/Clinical Presentation[1][edit | edit source]
• Swelling along the medial aspect of the foot and ankle
• Absence of the classical sudden severe pain of a tendon rupture
• Tenderness along the posterior tibialis tendon
• Progressive loss of longitudinal arch → pes planus and heel valgus
• Palpable pain between medial malleolus and navicular
• Pain in the plantar medial arch
Differential Diagnosis[2][edit | edit source]
• Attenuation or rupture of the calcaneonavicular (spring) ligament complex
• Degenerative arthritis of the ankle joint with valgus talar
• Arthritis of the talonavicular joint
• Posttraumatic tarsometatarsal (Lisfranc) joint arthritis
• Inflammatory arthritis of the hindfoot, usually secondary to rheumatoid disease
Diagnostic Procedures[edit | edit source]
add text here related to medical diagnostic procedures
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
Observation:[3]
Posterior tibialis tendon rupture is strongly suspected in patients presenting a complex of findings. These include:
• Eversion ankle injury
• Generalized medial ankle pain
• Medial ankle swelling
• Flexible, asymmetric pes planus and forefoot pronation
• Gait disturbance secondary to deformity
• Talonavicular sag in lateral standing radiograph
The first four findings are nondiagnostic, however, seen together they are helpful in identifying patients with posterior tibialis tendon pathology. Manual testing of the posterior tibialis tendon should be performed in the presence of these findings to confirm the tendon's functional status.
Tests:[4]
• Palpation from the area between the medial malleolus and os naviculare
• “Too many toes” sign secondary to an increase in forefoot abduction and heel eversion
• Nonfunctional posterior tibialis tendon on manual testing
• Motion of the ankle and subtalar joints
• Positive first metatarsal rise sign test
• Positive single-limb heel rise-test
• Ottawa ankle rules test to exclude fractures within the first week after an ankle injury
Medical Management [1][edit | edit source]
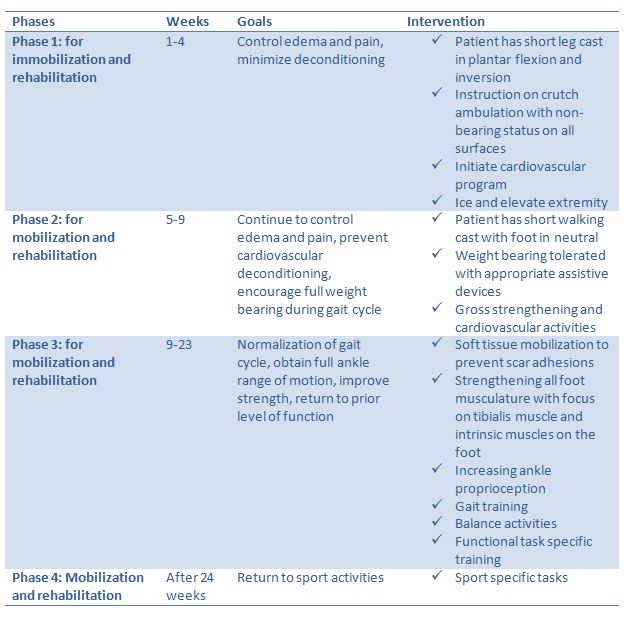
Postoperative rehabilitation for tendon transfer procedure:
Complications:
• With attenuation or rupture of the posterior tibial tendon, the medial longitudinal arch of the foot collapses and there is a relative internal rotation of the tibia and talus
• The subtalar joint everts, causing the heel to assume a valgus position and the foot to abduct at the talonavicular joint. A compensatory forefoot varus deformity ensues
• As the heel assumes an increased valgus alignment, the Achilles tendon becomes positioned lateral to the axis of rotation of the subtalar joint. Over time, the shortened position of the hindfoot results in an Achilles tendon contracture
• As the deformity progresses, the fibula abuts against the lateral wall of the calcaneus, causing pain in the lateral hindfoot
Physical Therapy Management [5][edit | edit source]
Furthermore, Woods and Leach (1991) pointed out that "the key" to successful treatment is early diagnosis23.
(Randall E. Marcus, 1993)
Phase I:
• Ice
• Non steroidal anti inflammatory drugs
• massage
Phase II:
• Passive ROM exercice for eversion and dorsiflexion such as manual mobilisation ankle
Phase III:
• Closed kinetic chain activities and eccentric strengthening exercises such as single leg standing toe raises with controlled lowering eccentric loads
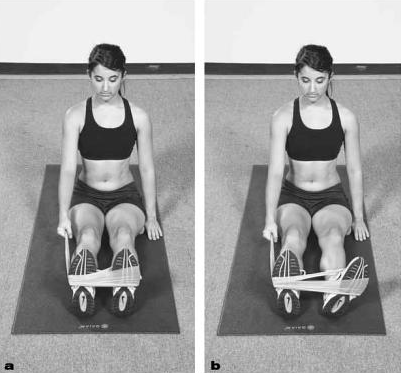
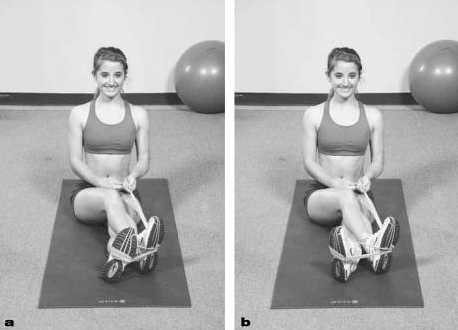
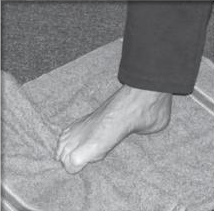
Phase III excercices:
without moving your leg, pull theraband away lateral with your foot
without moving your straight leg, invert your feet of your bended leg
without moving your leg, pull theraband away from you to the ground
place towel on the floor, keep the heel on the floor, use toes to pull towel towards you
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 Geideman WM, Johnson JE. Posterior Tibial Tendon Dysfunction. Journal of Orthopedic & Sports Physical Therapy. 2000; 30(2): 68-77
- ↑ Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 1989;(239):196-206.
- ↑ Marcus RE, Pfister ME. The enigmatic diagnosis of posterior tibialis tendon rupture. Iowa Orthop J. 1993;13:171-7.
- ↑ A. Foster, N. T. Rupture of the tibialis posterior tendon: an important differential in the assessment of ankle injuries. Ermergency Medical Journal , 2005 (4): 915-916
- ↑ Gregory S. Kolt, L. S.-M. Common sport-related injuries. In L. S.-M. Gregory S. Kolt, Physical Therapies in Sport and Exercise, Philadelphia, Elsevier 2007: 428-429