Urinary Tract Infection: Difference between revisions
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
== Introduction == | == Introduction == | ||
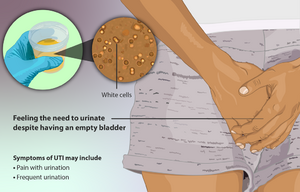
[[File:Urinary Tract Infection (UTI).png|thumb|Symptoms UTI]] | [[File:Urinary Tract Infection (UTI).png|thumb|Symptoms UTI]] | ||
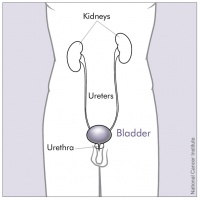
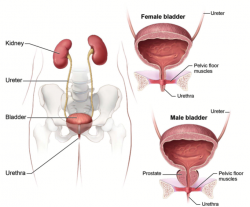
A urinary tract infection is an infection in any part of your urinary system, which includes the bladder, urethra, ureters (urine tubes) and kidneys. If untreated, UTIs can lead to kidney infection which can be very serious. UTIs are caused by microbes, mainly bacteria, but also fungi and viruses<ref name="Rose" />. | A urinary tract infection is an infection in any part of your urinary system, which includes the bladder, urethra, ureters (urine tubes) and kidneys. If untreated, UTIs can lead to kidney infection which can be very serious. UTIs are caused by microbes, mainly bacteria, but also fungi and viruses<ref name="Rose">Rosenblum, N. Recurrent Urinary Tract Infections. Urology. Available at: http://www.med.nyu.edu/urology/patient-care-information/conditions-we-treat/recurrent-urinary-tract-infections</ref>. | ||
Normally, bacteria that enters the urinary tract is rapidly removed by the body before symptoms are present, but sometimes this bacteria overcomes the natural defences of the body, resulting in an infection. This infection may involve the lower urinary tract only, or both the lower and upper urinary tracts<ref name="Rowe" />. The upper urinary tract is made up of the kidneys and the ureters, while the lower urinary tract is made up of the bladder and urethra <ref name="Rowe" />. | Normally, bacteria that enters the urinary tract is rapidly removed by the body before symptoms are present, but sometimes this bacteria overcomes the natural defences of the body, resulting in an infection. This infection may involve the lower urinary tract only, or both the lower and upper urinary tracts<ref name="Rowe" />. The upper urinary tract is made up of the kidneys and the ureters, while the lower urinary tract is made up of the bladder and urethra <ref name="Rowe" />. | ||
| Line 20: | Line 20: | ||
A major risk factor for UTI is catheter use. Sexual intercourse and the use of spermicides and diaphragms are also risk factors for UTI. Frequent pelvic exams and the presence of anatomical abnormalities of the urinary tract can also predispose one to a UTI. | A major risk factor for UTI is catheter use. Sexual intercourse and the use of spermicides and diaphragms are also risk factors for UTI. Frequent pelvic exams and the presence of anatomical abnormalities of the urinary tract can also predispose one to a UTI. | ||
UTIs are very common after a kidney transplant. The two triggers include the use of immunosuppressive drugs and vesicoureteral reflux. Other risk factors include the use of antibiotics and diabetes mellitus<ref>Bono MJ, Reygaert WC. Urinary tract infection. InStatPearls [Internet] 2021 Jun 23. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK470195/ (accessed 13.5.2022)</ref>. | UTIs are very common after a kidney transplant. The two triggers include the use of immunosuppressive drugs and vesicoureteral reflux. Other risk factors include the use of antibiotics and diabetes mellitus<ref name=":1">Bono MJ, Reygaert WC. Urinary tract infection. InStatPearls [Internet] 2021 Jun 23. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK470195/ (accessed 13.5.2022)</ref>. | ||
=== Epidemiology === | === Epidemiology === | ||
[[Image:Bladder.png|border|right|250x250px|Anatomy of Male and Female Bladder]]An estimated 150 million UTIs occur every year world-wide, adding to $6 billion in health care costs <ref name="Pontari" | [[Image:Bladder.png|border|right|250x250px|Anatomy of Male and Female Bladder]]An estimated 150 million UTIs occur every year world-wide, adding to $6 billion in health care costs <ref name="Pontari">M, Pontari. Adult UTI. Advancing Urology. Available at: www.auanet.org/education/adult-uti.cfm</ref>. | ||
* Urinary tract infections are very frequent bacterial infections in women. | |||
* Usually occur between the ages of 16 and 35 years, with 10% of women getting an infection yearly and more than 40% to 60% having an infection at least once in their lives. | |||
* Recurrences are common, with nearly half getting a second infection within a year. | |||
* Urinary tract infections occur at least four times more frequently in females than males<ref name=":1" /><br> | |||
== Characteristics/Clinical Presentation | == Characteristics/Clinical Presentation == | ||
Some of the symptoms of UTIs include: | Some of the symptoms of UTIs include: | ||
| Line 42: | Line 45: | ||
* Loin (lower abdominal) pain | * Loin (lower abdominal) pain | ||
* Pain in the back | * Pain in the back | ||
* Vomiting.<ref name=":0" /><br> | * Vomiting.<ref name=":0" /> | ||
Urinary Tract infections that are left untreated may lead to many complications, including urosepsis, systemic inflammatory response syndrome (SIRS), and chronic kidney infections. Sepsis associated with UTIs often requires hospitalization<ref name="Mody" />. <br> | |||
== | == Diagnosis == | ||
[[Image:UrineSample.jpg|125x150px|Urine sample|alt=|thumb]]Tests and procedures used to diagnose urinary tract infections include: | |||
* | * Analyzing a urine sample. | ||
* | * Growing urinary tract bacteria in a lab. This test finds what bacteria is causing infection and which medications will be most effective. | ||
Typically, symptoms of a UTI will conclude within 24-48 hours after treatment. A UTI is considered recurrent if the condition presents more than twice in 6 months <ref name="Rose" />. Additional tests include the following: kidney and bladder ultrasound, voiding cystourethrogram, computerized tomography (CT) scan, MRI, radionuclide scan, urodynamics, and cystoscopy <ref name="Urinary" /> | |||
== Prognosis == | |||
Even with proper antibiotic treatment, most UTI symptoms can last several days. In women with recurrent UTIs, the quality of life is poor, 25% of women experience such recurrences. Factors indicating a poor outlook include: Catheterization; Poor overall health; Advanced age; Presence of renal calculi; Diabetes (especially if poorly controlled); Presence of malignancy; Incontinence; Chronic diarrhea.<ref name=":1" /> | |||
== | |||
== Systemic Involvement == | == Systemic Involvement == | ||
| Line 83: | Line 64: | ||
Urinary Tract infections that are left untreated may lead to many complications, including urosepsis, systemic inflammatory response syndrome (SIRS), and chronic kidney infections. Sepsis associated with UTIs often requires hospitalization<ref name="Mody">Mody, L, Juhani-Mehtta, M. Urinary Tract Infections in Older Women: A Clinical Review. JAMA. 2014;311:844–854.</ref>. Urosepsis spreads into the bloodstream from its origin in the urinary tract. Kidney infections also progress to the blood stream, referred to as septicemia<ref name="Urinary">Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.</ref>. This complication can be life threatening. Systemic inflammatory response syndrome can also become life threatening if treatment fails. SIRS is usually the first incidence of multi-organ failure<ref name="Grabe">Grabe, M. Guidelines on Urological Infections. Urological Infections. Available at: http://uroweb.org/wp-content/uploads/19-urological-infections_lr2.pdf.</ref>. | Urinary Tract infections that are left untreated may lead to many complications, including urosepsis, systemic inflammatory response syndrome (SIRS), and chronic kidney infections. Sepsis associated with UTIs often requires hospitalization<ref name="Mody">Mody, L, Juhani-Mehtta, M. Urinary Tract Infections in Older Women: A Clinical Review. JAMA. 2014;311:844–854.</ref>. Urosepsis spreads into the bloodstream from its origin in the urinary tract. Kidney infections also progress to the blood stream, referred to as septicemia<ref name="Urinary">Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.</ref>. This complication can be life threatening. Systemic inflammatory response syndrome can also become life threatening if treatment fails. SIRS is usually the first incidence of multi-organ failure<ref name="Grabe">Grabe, M. Guidelines on Urological Infections. Urological Infections. Available at: http://uroweb.org/wp-content/uploads/19-urological-infections_lr2.pdf.</ref>. | ||
== | == Treatment == | ||
[[Image:Amoxicillin.jpg|200x200px|alt=|thumb|Amoxicillin]]Antibiotics usually are the first line treatment for urinary tract infections. Which drugs are prescribed and for how long depend on persons health condition and the type of bacteria found in your urine. | |||
The | The group of antibiotic medicines known as fluoroquinolones are not commonly recommended for simple UTIs, as the risks of these medicines generally outweigh the benefits for treating uncomplicated UTIs. In some cases, such as a complicated UTI or kidney infection, they may be prescribed, if there are no other treatment options. | ||
Pain medications may be prescribed (numbs your bladder and urethra to relieve burning while urinating), but pain usually is relieved soon after starting an antibiotic<ref>Moyo clinic UTI Available;https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/diagnosis-treatment/drc-20353453 (accessed 13.5.2022)</ref>. | |||
Antibiotics are usually taken anywhere from 3 days to 10 days, depending on severity of symptoms, comorbidities, complications of infection, and dosage <ref name="Rowe">Rowe, TA, Juthani-Mehta, M. Urinary tract infection in older adults. Aging Health. 2013;9(5).</ref> <ref name="Rose" />. Overutilization of antibiotics is a common issue, particularly in hospitals and long term facilities, which may cause patients to develop resistance to the medication over time <ref name="Rowe" />. | |||
Alternative treatment includes the use of probiotics, ensuring proper hydration, drinking cranberry juice, and urinating frequently <ref name="Beck">Becknell, B, Schober, M, Korbel, L, Spencer, JD. The Diagnosis, Evaluation and Treatment of Acute and Recurrent Pediatric Urinary Tract Infections. Expert Review of Anti-infective Therapy. 2015;13(1):81–90.</ref> <ref name="Mody" /><ref name="Urinary" />. Using a heating pad on the patient’s lower back or abdomen may also help the symptoms of the UTI<ref>Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.</ref>. Surgery may be required in the presence of an anatomical abnormality <ref name="Rose" />. | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
Physical therapists that are trained in pelvic floor dysfunction can greatly improve a UTI patient’s quality of life. A typical approach includes training pelvic floor musculature, manipulative techniques, local heat, breathing and relaxation techniques, postural education, muscle coordination reeducation, and behavioral therapy<ref name="Souza">Souza, EL, Figueiredo, EM, Velloso, FB, Geo, MS. Physiotherapy For Women with Recurrent Urinary Tract Infection: A Promising Approach. International Continence Society. 2013:223.</ref>. Therapists are also encouraged to educate the patient on drinking and voiding schedules to ensure consistency<ref name="De">De Paepe, H, Hoebeke, P, Renson, C, et al. Pelvic-floor therapy in girls with recurrent urinary tract infections and dysfunctional voiding. British Journal of Urology. 1998;3:10–9113.</ref>. Treatments and patient education have been found to improve efficiency of emptying the bladder, create better bowel habits, and promote full relaxation of the pelvic-floor when voiding<ref name="Souza" />. All of these factors may lead to a decreased incidence and reoccurrence of UTIs. | Physical therapists that are trained in pelvic floor dysfunction can greatly improve a UTI patient’s quality of life. A typical approach includes training pelvic floor musculature, manipulative techniques, local heat, breathing and relaxation techniques, postural education, muscle coordination reeducation, and behavioral therapy<ref name="Souza">Souza, EL, Figueiredo, EM, Velloso, FB, Geo, MS. Physiotherapy For Women with Recurrent Urinary Tract Infection: A Promising Approach. International Continence Society. 2013:223.</ref>. Therapists are also encouraged to educate the patient on drinking and voiding schedules to ensure consistency<ref name="De">De Paepe, H, Hoebeke, P, Renson, C, et al. Pelvic-floor therapy in girls with recurrent urinary tract infections and dysfunctional voiding. British Journal of Urology. 1998;3:10–9113.</ref>. Treatments and patient education have been found to improve efficiency of emptying the bladder, create better bowel habits, and promote full relaxation of the pelvic-floor when voiding<ref name="Souza" />. All of these factors may lead to a decreased incidence and reoccurrence of UTIs. | ||
< | For those patients in the hospital, recent studies have shown that mobilization of patients with a catheter is safe and is not associated with urinary-related adverse effects, including urinary tract infections<ref name="Lima">Lima, NP, Cardim da Silva, GM, Park, M, Pires-Neto, RC. Mobility therapy and central or peripheral catheter-related adverse events on an ICU in Brazil. J bras pneumol. 2015;41(3):225–230.</ref>. | ||
== | == '''Variation in Symptom Presentation''' == | ||
<div> | <div> | ||
Post-menopausal women present with constitutional symptoms, such as abdominal pain, back pain, chills, and constipation <ref name="Rowe" />. | Post-menopausal women present with constitutional symptoms, such as abdominal pain, back pain, chills, and constipation <ref name="Rowe" />. | ||
Nursing home patients present with nonspecific symptoms, such as confusion and a decline in functional status. | Nursing home patients present with nonspecific symptoms, such as confusion and a decline in functional status. | ||
A urinary infection in a child needs to be investigated as it may indicate a more serious condition. The most common urinary system condition is urinary reflux. With this condition, the bladder valve isn’t working properly and allows urine to flow back to the kidneys, increasing the risk of a kidney infection<ref name=":0" />. | |||
</div> | </div> | ||
== References == | == References == | ||
Revision as of 06:07, 13 May 2022
Introduction[edit | edit source]
A urinary tract infection is an infection in any part of your urinary system, which includes the bladder, urethra, ureters (urine tubes) and kidneys. If untreated, UTIs can lead to kidney infection which can be very serious. UTIs are caused by microbes, mainly bacteria, but also fungi and viruses[1].
Normally, bacteria that enters the urinary tract is rapidly removed by the body before symptoms are present, but sometimes this bacteria overcomes the natural defences of the body, resulting in an infection. This infection may involve the lower urinary tract only, or both the lower and upper urinary tracts[2]. The upper urinary tract is made up of the kidneys and the ureters, while the lower urinary tract is made up of the bladder and urethra [2].
Types of urinary tract infections (UTIs)[edit | edit source]
The different types of UTI can include:
- Urethritis – infection of the urethra
- Cystitis – infection of the bladder
- Pyelonephritis – infection of the kidneys
- Vaginitis – infection of the vagina.[3]
Etiology[edit | edit source]
Pathogenic bacteria ascend from the perineum, causing the UTI. Women have shorter urethras than men and therefore are far more susceptible to UTI.
A major risk factor for UTI is catheter use. Sexual intercourse and the use of spermicides and diaphragms are also risk factors for UTI. Frequent pelvic exams and the presence of anatomical abnormalities of the urinary tract can also predispose one to a UTI.
UTIs are very common after a kidney transplant. The two triggers include the use of immunosuppressive drugs and vesicoureteral reflux. Other risk factors include the use of antibiotics and diabetes mellitus[4].
Epidemiology[edit | edit source]
An estimated 150 million UTIs occur every year world-wide, adding to $6 billion in health care costs [5].
- Urinary tract infections are very frequent bacterial infections in women.
- Usually occur between the ages of 16 and 35 years, with 10% of women getting an infection yearly and more than 40% to 60% having an infection at least once in their lives.
- Recurrences are common, with nearly half getting a second infection within a year.
- Urinary tract infections occur at least four times more frequently in females than males[4]
Characteristics/Clinical Presentation[edit | edit source]
Some of the symptoms of UTIs include:
- Wanting to urinate more often and urgently, if only a few drops
- Burning pain or a ‘scalding’ sensation when urinating
- Feeling that the bladder is still full after urinating
- Pain above the pubic bone
- Cloudy, bloody or very smelly urine.
If infection reaches the kidneys, prompt medical attention is needed. In addition to the general symptoms of UTIs, a person with a kidney infection can also experience:
- Chills
- Fever
- Loin (lower abdominal) pain
- Pain in the back
- Vomiting.[3]
Urinary Tract infections that are left untreated may lead to many complications, including urosepsis, systemic inflammatory response syndrome (SIRS), and chronic kidney infections. Sepsis associated with UTIs often requires hospitalization[6].
Diagnosis[edit | edit source]
Tests and procedures used to diagnose urinary tract infections include:
- Analyzing a urine sample.
- Growing urinary tract bacteria in a lab. This test finds what bacteria is causing infection and which medications will be most effective.
Typically, symptoms of a UTI will conclude within 24-48 hours after treatment. A UTI is considered recurrent if the condition presents more than twice in 6 months [1]. Additional tests include the following: kidney and bladder ultrasound, voiding cystourethrogram, computerized tomography (CT) scan, MRI, radionuclide scan, urodynamics, and cystoscopy [7]
Prognosis[edit | edit source]
Even with proper antibiotic treatment, most UTI symptoms can last several days. In women with recurrent UTIs, the quality of life is poor, 25% of women experience such recurrences. Factors indicating a poor outlook include: Catheterization; Poor overall health; Advanced age; Presence of renal calculi; Diabetes (especially if poorly controlled); Presence of malignancy; Incontinence; Chronic diarrhea.[4]
Systemic Involvement[edit | edit source]
Urinary Tract infections that are left untreated may lead to many complications, including urosepsis, systemic inflammatory response syndrome (SIRS), and chronic kidney infections. Sepsis associated with UTIs often requires hospitalization[6]. Urosepsis spreads into the bloodstream from its origin in the urinary tract. Kidney infections also progress to the blood stream, referred to as septicemia[7]. This complication can be life threatening. Systemic inflammatory response syndrome can also become life threatening if treatment fails. SIRS is usually the first incidence of multi-organ failure[8].
Treatment[edit | edit source]
Antibiotics usually are the first line treatment for urinary tract infections. Which drugs are prescribed and for how long depend on persons health condition and the type of bacteria found in your urine.
The group of antibiotic medicines known as fluoroquinolones are not commonly recommended for simple UTIs, as the risks of these medicines generally outweigh the benefits for treating uncomplicated UTIs. In some cases, such as a complicated UTI or kidney infection, they may be prescribed, if there are no other treatment options.
Pain medications may be prescribed (numbs your bladder and urethra to relieve burning while urinating), but pain usually is relieved soon after starting an antibiotic[9].
Antibiotics are usually taken anywhere from 3 days to 10 days, depending on severity of symptoms, comorbidities, complications of infection, and dosage [2] [1]. Overutilization of antibiotics is a common issue, particularly in hospitals and long term facilities, which may cause patients to develop resistance to the medication over time [2].
Alternative treatment includes the use of probiotics, ensuring proper hydration, drinking cranberry juice, and urinating frequently [10] [6][7]. Using a heating pad on the patient’s lower back or abdomen may also help the symptoms of the UTI[11]. Surgery may be required in the presence of an anatomical abnormality [1].
Physical Therapy Management[edit | edit source]
Physical therapists that are trained in pelvic floor dysfunction can greatly improve a UTI patient’s quality of life. A typical approach includes training pelvic floor musculature, manipulative techniques, local heat, breathing and relaxation techniques, postural education, muscle coordination reeducation, and behavioral therapy[12]. Therapists are also encouraged to educate the patient on drinking and voiding schedules to ensure consistency[13]. Treatments and patient education have been found to improve efficiency of emptying the bladder, create better bowel habits, and promote full relaxation of the pelvic-floor when voiding[12]. All of these factors may lead to a decreased incidence and reoccurrence of UTIs.
For those patients in the hospital, recent studies have shown that mobilization of patients with a catheter is safe and is not associated with urinary-related adverse effects, including urinary tract infections[14].
Variation in Symptom Presentation[edit | edit source]
Post-menopausal women present with constitutional symptoms, such as abdominal pain, back pain, chills, and constipation [2].
Nursing home patients present with nonspecific symptoms, such as confusion and a decline in functional status.
A urinary infection in a child needs to be investigated as it may indicate a more serious condition. The most common urinary system condition is urinary reflux. With this condition, the bladder valve isn’t working properly and allows urine to flow back to the kidneys, increasing the risk of a kidney infection[3].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Rosenblum, N. Recurrent Urinary Tract Infections. Urology. Available at: http://www.med.nyu.edu/urology/patient-care-information/conditions-we-treat/recurrent-urinary-tract-infections
- ↑ 2.0 2.1 2.2 2.3 2.4 Rowe, TA, Juthani-Mehta, M. Urinary tract infection in older adults. Aging Health. 2013;9(5).
- ↑ 3.0 3.1 3.2 Better Health UTIs Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/urinary-tract-infections-uti (accessed 13.5.2022)
- ↑ 4.0 4.1 4.2 Bono MJ, Reygaert WC. Urinary tract infection. InStatPearls [Internet] 2021 Jun 23. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK470195/ (accessed 13.5.2022)
- ↑ M, Pontari. Adult UTI. Advancing Urology. Available at: www.auanet.org/education/adult-uti.cfm
- ↑ 6.0 6.1 6.2 Mody, L, Juhani-Mehtta, M. Urinary Tract Infections in Older Women: A Clinical Review. JAMA. 2014;311:844–854.
- ↑ 7.0 7.1 7.2 Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.
- ↑ Grabe, M. Guidelines on Urological Infections. Urological Infections. Available at: http://uroweb.org/wp-content/uploads/19-urological-infections_lr2.pdf.
- ↑ Moyo clinic UTI Available;https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/diagnosis-treatment/drc-20353453 (accessed 13.5.2022)
- ↑ Becknell, B, Schober, M, Korbel, L, Spencer, JD. The Diagnosis, Evaluation and Treatment of Acute and Recurrent Pediatric Urinary Tract Infections. Expert Review of Anti-infective Therapy. 2015;13(1):81–90.
- ↑ Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.
- ↑ 12.0 12.1 Souza, EL, Figueiredo, EM, Velloso, FB, Geo, MS. Physiotherapy For Women with Recurrent Urinary Tract Infection: A Promising Approach. International Continence Society. 2013:223.
- ↑ De Paepe, H, Hoebeke, P, Renson, C, et al. Pelvic-floor therapy in girls with recurrent urinary tract infections and dysfunctional voiding. British Journal of Urology. 1998;3:10–9113.
- ↑ Lima, NP, Cardim da Silva, GM, Park, M, Pires-Neto, RC. Mobility therapy and central or peripheral catheter-related adverse events on an ICU in Brazil. J bras pneumol. 2015;41(3):225–230.