Valgus Knee: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 22: | Line 22: | ||
== Classification: == | == Classification: == | ||
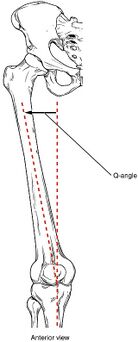
There are numerous grading systems used for the classification of the knee deformaty that depend on the severiry of deformation and the soft tissue involeved. But the most recent one descibes three grades of valgus deformity<ref>Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87(Suppl 1(Pt 2)):271–284</ref> | [[File:Q angle of knee.jpg|right|frameless|343x343px|Q angle]] | ||
There are numerous grading systems used for the classification of the knee deformaty that depend on the severiry of deformation and the soft tissue involeved. But the most recent one descibes three grades of valgus deformity<ref>Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87(Suppl 1(Pt 2)):271–284</ref> that depend on the degree of the angle . | |||
* Grade I: the deviation is less than 10°, passively correctable, with contracture of the lateral soft tissue but without elongation of the medial collateral ligament. | * Grade I: the deviation is less than 10°, passively correctable, with contracture of the lateral soft tissue but without elongation of the medial collateral ligament. | ||
| Line 29: | Line 30: | ||
== Diagnostic Procedures: == | == Diagnostic Procedures: == | ||
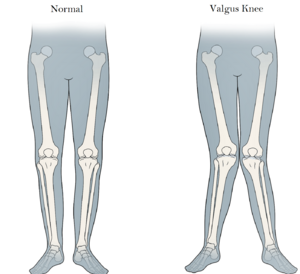
[[File:Valgus Knee.jpg|right|frameless]] | |||
[[X-Rays]] will help confirm the diagnosis, images of the hip and the ankle also should be taken. | [[X-Rays]] will help confirm the diagnosis, images of the hip and the ankle also should be taken. | ||
| Line 47: | Line 49: | ||
#* Growth stimulation by greenstick fracture of the proximal tibial metaphysic | #* Growth stimulation by greenstick fracture of the proximal tibial metaphysic | ||
#* Asymmetric growth arrest due to fracture-separation involving the lateral segment of the upper tibial physis or distal femoral physis. | #* Asymmetric growth arrest due to fracture-separation involving the lateral segment of the upper tibial physis or distal femoral physis. | ||
# Infection – causing asymmetric growth disturbance | # Infection – causing asymmetric growth disturbance. | ||
# Arthritis of knee – rheumatoid, hemophylia | # Arthritis of knee – rheumatoid, hemophylia | ||
# Metabolic bone disease.<ref>Ramin E, Seyed M, and Taghi B.Angular Deformities of the Lower Limb in Children.2010:46–53.</ref> | |||
# Metabolic bone disease | |||
== Management: == | == Management: == | ||
Treatment for genu valgum depends on the causes and severity of your symptoms. | |||
# Non-operative treatment | # Non-operative treatment | ||
- Conservative management | - <u>Conservative management:</u>With an orthosis like a brace or a splint has been suggested for children under 8 years old to help bone growth , but there is no evidence to substantiate the efficacy of this method<ref>Greene WB. Genu varum and genu valgum in children: differential diagnosis and guidelines for evaluation. Compr Ther. 1996;22:22–9</ref>. | ||
-Physical Therapy | <u>-Physical Therapy</u>: Exercise can help realign and stabilize the knees. depending on the deformaty and the cause , the therapist suggest exercises designed to strengthen the leg, hip, and thigh muscles. Specific stretches may also be useful in relieving symptoms. Posture of the leg can help reduce the angle . | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 18:29, 26 April 2022
Original Editor - Yesmine Gouddi
Top Contributors - Yesmine Gouddi and Sehriban Ozmen
Definition[edit | edit source]
Valgus knee or knock knee is a lower leg deformity that exists when the bone at the knee joint is angled out and away from the body's midline. This deformity is defined as a valgus angle equal to or greater than 10°[1]
The valgus deformity is resulted of anatomical variations : bone tissue remodelling and soft tissue contraction/elongation.
Bone tissue remodelling:
- Lateral femoral condyle deficiency with external rotation deformity of the tibia and lateral tibial plateau deficiency as well.
- The patellofemoral joint can be affected with lateral subluxation of the patella and trochlear blunting secondary to lateral femoral condylar wear.
Soft tissue contraction/elongation:
- The lateral side is contracted including the lateral collateral ligament (LCL), popliteus tendon, posterolateral capsule, iliotibial band (IT band), and posterior capsule.
- The medial side, the soft tissue are attenuated, the medial collateral ligament (MCL) .
Classification:[edit | edit source]
There are numerous grading systems used for the classification of the knee deformaty that depend on the severiry of deformation and the soft tissue involeved. But the most recent one descibes three grades of valgus deformity[2] that depend on the degree of the angle .
- Grade I: the deviation is less than 10°, passively correctable, with contracture of the lateral soft tissue but without elongation of the medial collateral ligament.
- Grade II: the axial deviation ranges between 10 and 20°, the lateral structures are contracted and the MCL is elongated but functional.
- Grade III: the axial deformity is greater than 20°, the lateral structures are tight and the medial stabilisers are not functional.
Diagnostic Procedures:[edit | edit source]
X-Rays will help confirm the diagnosis, images of the hip and the ankle also should be taken.
Physical examination should be performed with the patient both seated and standing. Take note of:
- The Degree of Q angle of genu valgum with a goniometer on the lateral side of the thigh-leg, the distance between the medial maleolli with the knee just touching. [3]
- the gait should be observed, in order to identify other dynamic instabilities.
- Any sagittal deformity like flexion contracture or recurvatum, as well as any rotational deformity.
- The knee should be evaluated for anteroposterior laxity, range of motion (ROM), coronal and sagittal deformity, and mediolateral instability.[4]
Causes and Contributing Factors:[edit | edit source]
- Developmental – physiologic, no intrinsic bone disease or congenital anomaly.
- Congenital – due to longitudinal deficiency of the fibula.
- Iliotibial band contracture.
- Trauma
- Malunion of fracture
- Growth stimulation by greenstick fracture of the proximal tibial metaphysic
- Asymmetric growth arrest due to fracture-separation involving the lateral segment of the upper tibial physis or distal femoral physis.
- Infection – causing asymmetric growth disturbance.
- Arthritis of knee – rheumatoid, hemophylia
- Metabolic bone disease.[5]
Management:[edit | edit source]
Treatment for genu valgum depends on the causes and severity of your symptoms.
- Non-operative treatment
- Conservative management:With an orthosis like a brace or a splint has been suggested for children under 8 years old to help bone growth , but there is no evidence to substantiate the efficacy of this method[6].
-Physical Therapy: Exercise can help realign and stabilize the knees. depending on the deformaty and the cause , the therapist suggest exercises designed to strengthen the leg, hip, and thigh muscles. Specific stretches may also be useful in relieving symptoms. Posture of the leg can help reduce the angle .
References[edit | edit source]
- ↑ Long WJ, Scuderi GRVarus and Valgus Deformities. In: Lotke PA, Lonner JH, eds. Knee Arthroplasty, Masters Techniques in Orthopaedic Surgery. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2009:111–125
- ↑ Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87(Suppl 1(Pt 2)):271–284
- ↑ Guichet JM, Javed A, Russell J, Saleh M. Effect of the foot on the mechanical alignment of the lower limbs. Clin Orthop Relat Res. 2003;415:193–201.
- ↑ W-Dahl, Annette; Toksvig-Larsen, Sören; Roos, Ewa M . "Association between knee alignment and knee pain in patients surgically treated for medial knee osteoarthritis by high tibial osteotomy. A one year follow-up study"(2009)
- ↑ Ramin E, Seyed M, and Taghi B.Angular Deformities of the Lower Limb in Children.2010:46–53.
- ↑ Greene WB. Genu varum and genu valgum in children: differential diagnosis and guidelines for evaluation. Compr Ther. 1996;22:22–9