Vulvar Hygiene: Difference between revisions
No edit summary |
Nicole Hills (talk | contribs) mNo edit summary |
||
| Line 10: | Line 10: | ||
'''Physiology of the vulvovaginal area:'''<ref name=":1">Chen Y, Bruning E, Rubino J, Eder SE. Role of female intimate hygiene in vulvovaginal health: Global hygiene practices and product usage. Women's Health. 2017 Dec;13(3):58-67.</ref> | '''Physiology of the vulvovaginal area:'''<ref name=":1">Chen Y, Bruning E, Rubino J, Eder SE. Role of female intimate hygiene in vulvovaginal health: Global hygiene practices and product usage. Women's Health. 2017 Dec;13(3):58-67.</ref> | ||
The vulva is the first line of defense to protect the genital tract from infection | The vulva is the first line of defense to protect the genital tract from infection. The vulvar skin differs from other skin sites because of its increased hydration, occlusion, and frictional properties, it is also more susceptible to topical agents.The normal vaginal microflora, acidic vaginal pH, and vaginal discharge are all components to maintain the health of the vulvovaginal region. Estrogen promotes the growth of lactobacilli, which is a bacteria in the vagina that has several important functions. This bacteria maintains a slightly acidic environment in the vagina, reducing the likelihood of infections. As estrogen levels decrease during menopause, a women's pH increase and is associated with increased colonization with pathogenic microbes, resulting in an increase in vulvar skin disorders at this time. Additionally, there are several external factors that can affect the vaginal microflora and microbial growth, such as hygiene practices, sexual intercourse, the use of antibiotics, increased moisture, sweating, menses, and hormone replacement therapy, potentially resulting in odor and vulvovaginal infection.<ref name=":2" /><ref name=":1" /> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 17: | Line 17: | ||
== Importance of Educating Patients on Vulvar Proper Care == | == Importance of Educating Patients on Vulvar Proper Care == | ||
There are numerous products on the market targeting women and the vulvar region. Women's daily cleansing routine are impacted by many factors, including personal preference, cultural norms, religious practices, and guidance from health care professionals. It is important as health care professionals who interact with this population to educate on the topic of proper vulvar care. Some of the products and cleansing routines may actually cause harm | There are numerous products on the market targeting women and the vulvar region. Women's daily cleansing routine are impacted by many factors, including personal preference, cultural norms, religious practices, and guidance from health care professionals. It is important as health care professionals who interact with this population to educate on the topic of proper vulvar care. Some of the products and cleansing routines may actually cause harm. For example, intimate hygiene products for cleanliness and odor control may upset pH in the vulvovaginal area, which will affect the composition of the normal vulvovaginal microbiota needed for protection against infection. Vaginal douching has also been associated with an increased risk of pelvic inflammatory disease, endometriosis, and sexually transmitted infections.<ref name=":1" /> | ||
Irritation in the vulvar region can contribute to: | Irritation in the vulvar region can contribute to: | ||
| Line 28: | Line 28: | ||
== Vulvar Care == | == Vulvar Care == | ||
It is not absolutely necessary to follow each of these suggestions | It is not absolutely necessary to follow each of these suggestions; it is dependent on the patient's specific situation. | ||
'''Clothing and Laundry'''<ref name=":0">National Vulvodynia Association. Self help tips. Available from: https://www.nva.org/for-patients/self-help-tips/</ref><ref name=":3">The Ottawa Hospital. Vulvar Care. Available from: https://www.ottawahospital.on.ca/en/documents/2017/01/vulvar-care-e.pdf/</ref> | '''Clothing and Laundry'''<ref name=":0">National Vulvodynia Association. Self help tips. Available from: https://www.nva.org/for-patients/self-help-tips/</ref><ref name=":3">The Ottawa Hospital. Vulvar Care. Available from: https://www.ottawahospital.on.ca/en/documents/2017/01/vulvar-care-e.pdf/</ref> | ||
| Line 44: | Line 44: | ||
* Avoid getting shampoo on the vulvar area | * Avoid getting shampoo on the vulvar area | ||
* Do not use bubble bath, feminine hygiene products, or any perfumed creams or soaps | * Do not use bubble bath, feminine hygiene products, or any perfumed creams or soaps | ||
* Wash the vulva with cool to lukewarm water only - the vagina is self cleansing and does not require soap | * Wash the vulva with cool to lukewarm water only - the vagina is self-cleansing and does not require soap | ||
* Use 100% cotton menstrual pads and tampons and do not | * Use 100% cotton menstrual pads and tampons and do not leave your tampon in overnight | ||
'''Sexual Intercourse'''<ref name=":0" /> | '''Sexual Intercourse'''<ref name=":0" /> | ||
* Use a lubricant that is water soluble | * Use a lubricant that is water soluble | ||
| Line 51: | Line 51: | ||
* Do not use contraceptive creams or spermicides | * Do not use contraceptive creams or spermicides | ||
'''Physical Activity'''<ref name=":0" /> | '''Physical Activity'''<ref name=":0" /> | ||
* Avoid exercises that | * Avoid exercises that puts direct pressure on the vulva such as bicycle riding and horseback riding | ||
* Limit intense exercises that create a lot of friction in the vulvar area (try lower intensity exercises such as walking) | * Limit intense exercises that create a lot of friction in the vulvar area (try lower intensity exercises such as walking) | ||
* Use a frozen gel pack wrapped in a towel to relieve symptoms after exercise | * Use a frozen gel pack wrapped in a towel to relieve symptoms after exercise | ||
Revision as of 15:17, 7 May 2019
Definition[edit | edit source]
Definitions:[1]
- Vulva: the external female genital area
- Labia majora: the outer folds of skin
- Labia minora: the inner folds of skin
- The vestibule surrounds the opening of the vagina, which is the tube-like structure surrounded by muscles leading from the uterus to the outside of the body
Physiology of the vulvovaginal area:[2]
The vulva is the first line of defense to protect the genital tract from infection. The vulvar skin differs from other skin sites because of its increased hydration, occlusion, and frictional properties, it is also more susceptible to topical agents.The normal vaginal microflora, acidic vaginal pH, and vaginal discharge are all components to maintain the health of the vulvovaginal region. Estrogen promotes the growth of lactobacilli, which is a bacteria in the vagina that has several important functions. This bacteria maintains a slightly acidic environment in the vagina, reducing the likelihood of infections. As estrogen levels decrease during menopause, a women's pH increase and is associated with increased colonization with pathogenic microbes, resulting in an increase in vulvar skin disorders at this time. Additionally, there are several external factors that can affect the vaginal microflora and microbial growth, such as hygiene practices, sexual intercourse, the use of antibiotics, increased moisture, sweating, menses, and hormone replacement therapy, potentially resulting in odor and vulvovaginal infection.[1][2]
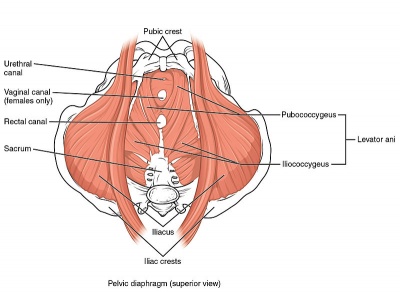
Clinically Relevant Anatomy[edit | edit source]
Please see the page "Pelvic Floor Anatomy," for further details regarding anatomy.
Importance of Educating Patients on Vulvar Proper Care[edit | edit source]
There are numerous products on the market targeting women and the vulvar region. Women's daily cleansing routine are impacted by many factors, including personal preference, cultural norms, religious practices, and guidance from health care professionals. It is important as health care professionals who interact with this population to educate on the topic of proper vulvar care. Some of the products and cleansing routines may actually cause harm. For example, intimate hygiene products for cleanliness and odor control may upset pH in the vulvovaginal area, which will affect the composition of the normal vulvovaginal microbiota needed for protection against infection. Vaginal douching has also been associated with an increased risk of pelvic inflammatory disease, endometriosis, and sexually transmitted infections.[2]
Irritation in the vulvar region can contribute to:
- dyspareunia
- interstitial cystitis
- yeast infections
- bacterial vaginosis
- urinary tract infection
- increased itching
Vulvar Care[edit | edit source]
It is not absolutely necessary to follow each of these suggestions; it is dependent on the patient's specific situation.
- Wear cotton underwear
- Do not wear pantyhose (wear thigh high or knee high hose instead)
- Wear loose-fitting pants or skirts
- Remove wet bathing suits and exercise clothing promptly
- Use dermatologically approved detergent such as Purex or Clear
- Double-rinse underwear and any other clothing that comes into contact with the vulva
- Do not use fabric softener on undergarments
- Do not wear tight underwear at night
- Use soft, white, unscented toilet paper
- Use lukewarm or cool sitz baths to relieve burning and irritation
- Avoid getting shampoo on the vulvar area
- Do not use bubble bath, feminine hygiene products, or any perfumed creams or soaps
- Wash the vulva with cool to lukewarm water only - the vagina is self-cleansing and does not require soap
- Use 100% cotton menstrual pads and tampons and do not leave your tampon in overnight
Sexual Intercourse[3]
- Use a lubricant that is water soluble
- Urinate (to prevent infection) and/or rinse vulva with cool water after sexual intercourse
- Do not use contraceptive creams or spermicides
Physical Activity[3]
- Avoid exercises that puts direct pressure on the vulva such as bicycle riding and horseback riding
- Limit intense exercises that create a lot of friction in the vulvar area (try lower intensity exercises such as walking)
- Use a frozen gel pack wrapped in a towel to relieve symptoms after exercise
- Enroll in an exercise class such as yoga to learn stretching and relaxation exercises
- Don’t swim in highly chlorinated pools
- Avoid the use of hot tubs
Resources[edit | edit source]
The American College of Obstetricians and Gynecologists: FAQ on Vulvovaginal Health
The Pelvic Guru: Your vagina is not cussing you - Good simple vulvovaginal hygiene tips
References[edit | edit source]
- ↑ 1.0 1.1 The American College of Obstetricians and Gynecologists. Vulvovaginal Health. Available from: https://www.acog.org/Patients/FAQs/Vulvovaginal-Health
- ↑ 2.0 2.1 2.2 Chen Y, Bruning E, Rubino J, Eder SE. Role of female intimate hygiene in vulvovaginal health: Global hygiene practices and product usage. Women's Health. 2017 Dec;13(3):58-67.
- ↑ 3.0 3.1 3.2 3.3 National Vulvodynia Association. Self help tips. Available from: https://www.nva.org/for-patients/self-help-tips/
- ↑ 4.0 4.1 The Ottawa Hospital. Vulvar Care. Available from: https://www.ottawahospital.on.ca/en/documents/2017/01/vulvar-care-e.pdf/