Wheelchair Users: Difference between revisions
No edit summary |
No edit summary |
||
| Line 140: | Line 140: | ||
Progressive diseases by nature CHANGE, some slowly over a number of years but some quickly in a period of months. By ignoring that during assessment for a wheelchair and only taking a “snapshot” of how the person currently is during the seating clinic we are doing a disservice to individuals with a progressive neurological condition and potentially providing them with an inappropriate wheelchair. There are diagnosis specific considerations that should be taken into account to ensure that the seating system can react to functional declines. | Progressive diseases by nature CHANGE, some slowly over a number of years but some quickly in a period of months. By ignoring that during assessment for a wheelchair and only taking a “snapshot” of how the person currently is during the seating clinic we are doing a disservice to individuals with a progressive neurological condition and potentially providing them with an inappropriate wheelchair. There are diagnosis specific considerations that should be taken into account to ensure that the seating system can react to functional declines. | ||
== [[MS Multiple Sclerosis|Multiple Sclerosis]] == | === [[MS Multiple Sclerosis|Multiple Sclerosis]] === | ||
<div align="justify"> | |||
<div align="justify"> | |||
<div align="justify"> | |||
<div align="justify"><div align="justify"> | |||
''Multiple Sclerosis (MS) is an immune-mediated disease characterized by inflammation, selective demyelination of central nervous system axons and gliosis, destroying the myelin and the axon in variable degrees causing both acute and chronic symptoms resulting into significant physical disability and impaired quality of life.''<ref name=":6">Medscape. Multiple Sclerosis. https://emedicine.medscape.com/article/1146199-overview (accessed 02 June 2018)</ref> The course that Multiple Sclerosis can be unpredictable with the hallmark being symptomatic episodes that occur months or years apart and affect different anatomic locations. In most cases, the disease follows a relapsing-remitting pattern, with short-term episodes of neurologic deficits that resolve completely or almost completely. A minority of patients experience steadily progressive neurologic deterioration. | ''Multiple Sclerosis (MS) is an immune-mediated disease characterized by inflammation, selective demyelination of central nervous system axons and gliosis, destroying the myelin and the axon in variable degrees causing both acute and chronic symptoms resulting into significant physical disability and impaired quality of life.''<ref name=":6">Medscape. Multiple Sclerosis. https://emedicine.medscape.com/article/1146199-overview (accessed 02 June 2018)</ref> The course that Multiple Sclerosis can be unpredictable with the hallmark being symptomatic episodes that occur months or years apart and affect different anatomic locations. In most cases, the disease follows a relapsing-remitting pattern, with short-term episodes of neurologic deficits that resolve completely or almost completely. A minority of patients experience steadily progressive neurologic deterioration. | ||
Revision as of 11:00, 15 July 2018
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Naomi O'Reilly, Kim Jackson, Jess Bell, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Rucha Gadgil, Amrita Patro, Lucinda hampton and Olajumoke Ogunleye
Introduction[edit | edit source]
About 10% of the global population, i.e. about 650 million people, have a disability with research indicating that some 10% or 65 million people require the use of a wheelchair. In 2003, it was estimated that 20 million of those requiring a wheelchair for mobility did not have one, and of those who did have a wheelchair, very few had access to an appropriate wheelchair. [1]
Wheelchair users are people who already have a wheelchair or who can benefit from using a wheelchair because their ability to walk is limited or inefficient. The needs of each wheelchair user will vary. However, they all need an appropriate wheelchair. Every well-fitting wheelchair provides the user some postural support. The backrest, cushion, footrests and armrests all provide postural support when adjusted to suit the wheelchair user’s size. However many children and adults need additional postural support in their wheelchair. Wheelchair users include Children, Adults and the Elderly; both men and women who have a wide range of mobility impairments, lifestyles, life roles and backgrounds; living and working in different environments including rural, semi-urban and urban.[1] Here we will take a look at just some of the range of wheelchair users and some of their requirements in relation to wheelchair mobility.
Non-Progressive Neurological Conditions[edit | edit source]
Cerebral Palsy[edit | edit source]
Cerebral Palsy has been defined as a group of permanent, but not unchanging, disorders of movement and/or posture, causing activity limitations which are due to a non-progressive interference, lesion, or abnormality of the developing or immature brain, resulting in a wide range of impairments which affect people very differently.[2][3]
Personal mobility can range from independent, unaided walking through to totally dependent wheelchair mobility with up to one third of children and adults with Cerebral Palsy being non-ambulant and reliant on some form of wheelchair mobility, either manual or powered, indoor or outdoor.[4]
A recent study by Rodby-Bousquet and Hägglund describe the use of manual and powered wheelchair indoors and outdoors in relation to the degree of independent wheelchair mobility or need for assistance in children with Cerebral Palsy, suggesting that environmental factors, influence of parents, personal factors (e.g. choice, motivation, acceptance of disability) and body functions (e.g. spasticity, fatigue) are important when it comes to use of a manual or powered wheelchair, both indoors and outdoors.[4]
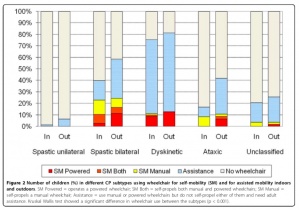
Children at GMFCS Level III predominantly used manual wheelchairs for self-mobility, while powered wheelchairs were more frequent at GMFCS Level IV. (Fig 1). More children used a wheelchair for outdoor mobility than indoor mobility, with the number using both manual and powered wheelchair outdoors increasing with GMFCS Levels. At GMFCS Level I 2% used a wheelchair, 39% at Level II and 85-90% at Levels III-V. Similarly the number of children requiring adult assistance increased with increasing GMFCS Levels, with only 14% overall being able to independently self-propel for outdoor mobility. (Fig.1).[4]
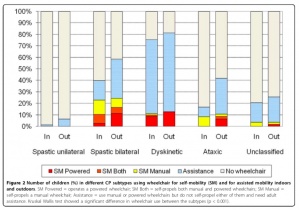
Rodby-Bousquet and Hägglund also found a difference in wheelchair use between different subtypes of cerebral palsy, with a higher incidence of wheelchair use for indoor mobility among the dyskinetic subtype. In this group of children only 11% could self propel (Fig.2), [4] while those who were utilising Powered Wheelchairs indoors had predominantly dyskinetic cerebral palsy or spastic diplegia.More children with spastic bilateral cerebral palsy had independent wheeled mobility compared to the other subtypes, in total 24% (Fig.2). [4]
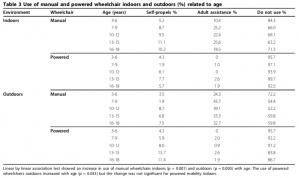
Finally Rodby-Bousquet and Hägglund [4] found that the use of manual wheelchairs for indoor mobility was similar for boys (30%) and girls (29%) with overall indoor wheelchair mobility increasing with age, although the same was not evident for powered wheelchair use.
Postural instability was seen as one of the key areas that can restrict functional performance and upper extremity function in children with cerebral palsy, in some cases leading to difficulties in self propulsion in wheelchair mobility both in manual and powered wheelchair use, with up to 89% showing instability during manual wheelchair self-propulsion and 61% during powered wheelchair self-propulsion.[8][4]
There is sometimes a resistance to prescribe a wheelchair to children, in particular younger children who may have some ability to walk. Current evidence suggests that there are many benefits for children with impaired walking ability to access a wheelchair to increase their independence in their environment, with early self-produced mobility crucial for the child's cognitive and psychosocial development. [9] Use of wheelchairs in children with impaired walking ability has been shown to have a less negative impact on visuomotor accuracy than walking with assistive devices due to a lower energy cost, while social interaction and participation in the improved. Self-initiated behaviours including interaction with objects, communication and changes in location were also more evident in children, as young as 23-38 months when provided with access to wheelchair mobility.[4][10]
To achieve as high a level of independent mobility as possible, both manual and powered wheelchairs should be considered at an early age for children with cerebral palsy who show impaired walking ability, ensuring provision of a stable sitting posture to improve function and wheeled mobility.[4]
Spina Bifida[edit | edit source]
Spina Bifida is defined as a neural tube defect (NTD) that results when the inferior neuropore does not close. Developing vertebrae do not close around an incomplete neural tube, resulting in a bony defect at the distal end of the tube. [11] Symptoms of spina bifida vary widely dependant on both on the severity of the neural tube defect and the location on the spinal cord, which are also the key factor in determining the type of wheelchair mobility.
Average worldwide incidence of spina bifida is 1 per 1000 births, but marked geographic variations occur. The highest rates are found in Ireland and Wales, where 3-4 cases of myelomeningocele per 1000 population have been reported with frequencies ranging from 0.9 in Canada, 0.7 in France, 7.7 in United Arab Emirates and 11.7 in South America. [12]
Spina bifida, in particular the more severe myelomeningocele form, can cause a number of clinical and developmental concerns, typically including difficulty with mobility, altered sensation and in some cases hydrocephalus, which is often treated with a ventriculoperitoneal shunt that drains excess fluid into the abdominal cavity, where it is absorbed by the body. If this fluid imbalance creates too much pressure on the brain, it can cause damage to the brain, resulting in additional neurologic insult potentially affecting mobility i.e., tonal changes, balance issues, etc.[12]
Personal mobility can range from independent, unaided walking through to totally reliant on some form of wheelchair mobility, either manual or powered. In some children with lower-level lesions they will have some degree of ambulation, but acquisition of this mobility is often delayed, while those with higher-level lesions often have no functional ambulation, requiring manual or powered wheelchairs.
Children with sensory levels below L3 are more likely to ambulate as adults and are less likely to have pressure sores or need daily care.[13] Evidence shows that approximately 50-60% of young adults with spina bifida ambulate household or community distances, with about 20% of these using some orthotic or assistive device, while the other 50% use a wheelchair as their primary form of mobility. Approximately 20% of these individuals ambulate with orthotics and assistive devices as a form of therapeutic exercise. [13][14]
Some challenges when prescribing mobility equipment for children with spina bifida are reducing the risk for spinal deformity, risk of shoulder-overuse injury associated with lifetime wheelchair use and addressing the need for multiple types of mobility equipment, including orthotic management, ambulation aids such as crutches or walkers, and a wheelchair.
| Level of Neural
Tube Defect |
Muscle Function | Anticiapted Mobility |
|---|---|---|
| Group 1
Thoracic High Lumbar |
|
Household ambulator till approx. 13 years, with use of Hip-Knee-Ankle-Foot-Orthosis (HKAFO) or Reciprocating Gait Orthosis
95%-99% are wheelchair users as adults, although exceptions are seen Manual Wheelchair main form of mobility Power Wheelchair may be used due to impairments such as poor cardiovascular fitness, shoulder pain, severe scoliosis / kyphosis |
| Group 2
Low Lumbar |
|
Ambulation requires ankle-foot orthoses (AFO) and crutches
79% retain community ambulation as adults Most use wheelchairs for long-distance mobility Significant difference in ability to walk between L4 and L3 level Lesions Medial hamstring function is needed for community ambulation |
| Group 3
High Sacral |
|
Walks with and without support but uses AFO Braces;
Has characteristic gluteus lurch with excessive pelvic obliquity and rotation during gait |
| Group 3
Low Sacral |
|
Walks without the need for AFO’s;
Gait is close to normal |
For more information on how Spina Bifida impacts on daily function you can read the following Handout from the Spina Bifida Association;
Spinal Cord Injury[edit | edit source]
Spinal cord injury is defined as traumatic damage to the spinal cord or nerves at the end of the spinal canal, which can affect conduction of sensory and motor signals across the site of the lesion. There are two types of spinal cord injury: Incomplete and Complete injury. [16]
- Incomplete Lesion: not all the nerves are severed or the nerves are only slightly damaged. Recovery is possible, but never to pre-injury level.
- Complete Lesion: the nerves are severed and there is no motor or sensory function preserved of this point. [16]
Symptoms of a spinal cord injury vary widely dependant on both on the severity of injury and the location on the spinal cord, which are also the key factor in determining the type of wheelchair mobility. Personal mobility can range from independent, unaided walking through to totally reliant on some form of wheelchair mobility, either manual or powered.
People with a spinal cord injury are very likely to be at risk of developing a pressure sore. This is because most people with a spinal cord injury cannot feel below the level of their injury. Always prescribe a pressure relief cushion.
| Level of Injury | Type of Wheelchair Mobility |
|---|---|
| C1 - C4 Tetraplegia |
|
| C5 Tetraplegia |
|
| C6 - C8 Tetraplegia |
|
| T1 - T12 Paraplegia |
|
Progressive Neurological Conditions[edit | edit source]
Progressive diseases by nature CHANGE, some slowly over a number of years but some quickly in a period of months. By ignoring that during assessment for a wheelchair and only taking a “snapshot” of how the person currently is during the seating clinic we are doing a disservice to individuals with a progressive neurological condition and potentially providing them with an inappropriate wheelchair. There are diagnosis specific considerations that should be taken into account to ensure that the seating system can react to functional declines.
Multiple Sclerosis[edit | edit source]
Multiple Sclerosis (MS) is an immune-mediated disease characterized by inflammation, selective demyelination of central nervous system axons and gliosis, destroying the myelin and the axon in variable degrees causing both acute and chronic symptoms resulting into significant physical disability and impaired quality of life.[17] The course that Multiple Sclerosis can be unpredictable with the hallmark being symptomatic episodes that occur months or years apart and affect different anatomic locations. In most cases, the disease follows a relapsing-remitting pattern, with short-term episodes of neurologic deficits that resolve completely or almost completely. A minority of patients experience steadily progressive neurologic deterioration.
There are approximately 2.1 million people worldwide affected by multiple sclerosis, affecting all races and all parts of the world with rates varying widely but generally the prevalence tends to increase with latitude (eg, lower rates in the tropics, higher rates in northern Europe), but with many exceptions to this gradient (eg, low rates among Chinese, Japanese, and African blacks; high rates among Sardinians, Parsis, and Palestinians). More than 30% of people with multiple sclerosis will develop significant physical disability, with a large portion relying on wheelchair for personal mobility in particular those with primary progressive which has a high incidence of spinal cord involvement. [17]
Symptoms of a multiple sclerosis vary widely dependant on both on the subtype and the location of the lesions including sensory loss, spinal cord symptoms (motor and autonomic), cerebellar symptoms nystagmus, and intention tremor, fatigue, dizziness, pain etc, which are also the key factor in determining the type of mobility. Personal mobility can range from independent, unaided walking through to totally reliant on some form of wheelchair mobility, either manual or powered. [17]
In contrast to cases involving sudden disability, mobility aids take on a new meaning in the context of diseases like multiple sclerosis that tend toward chronic progression making it particularly challenging to decide when to recommend the use of a wheelchair and which model to use. Many individuals with multiple sclerosis can be reluctant to make use of mobility aids feeling that they will become more dependant on them and often signifying an advanced element of disease progression. The selection of an appropriate wheelchair can be more complex due to the unpredictable and potentially progressive nature of multiple sclerosis e.g. the wheelchair needs of person with multiple sclerosis can change, as does ambulatory status, because the appropriate chair for occasional community access is different from one required for full-time mobility use. Most people with multiple sclerosis start using a wheelchair, either manual or powered, just for specific activities such as outdoor mobility to help conserve strength and reduce fatigue, or as an aid to help reduce the risk of falling. The goal with individuals with multiple sclerosis is to maintain mobility, maximize stability and safety, while reducing the effort required. [18]
Motor Neuron Disease[edit | edit source]
Motor Neuron Disease are a clinically and pathologically heterogeneous group of neurologic diseases characterized by progressive degeneration of motor neurons; which include both sporadic and hereditary diseases, that progressively damages parts of the nervous system. Attacking both the upper and lower motor neurones affecting either or both of the following 2 sets of motor neurons; [19][20]
- Upper Motor Neurons (UMNs), which originate from the primary motor cortex of the cerebrum (precentral gyrus) and possess long axons forming corticospinal and corticobulbar tracts
- Lower Motor Neurons (LMNs), which originate in the brainstem (cranial nerve, motor nuclei) and spinal cord (anterior horn cells) and directly innervate skeletal muscles
Characterised by muscles stiffness, muscle twitching and spasticity, and gradually worsening weakness due to muscles atrophy which results in difficulty with activities of daily living, mobility, speech, swallow, and eventually breathing. Individuals affected by the disorder may ultimately lose the ability to initiate and control all voluntary movement, although bladder and bowel function and the muscles responsible for eye movement are usually spared until the final stages of the disorder. As motor neuron disease is rapidly progressive, services face challenges to respond to the changing needs of clients with evidence highlighting lengthy delays in supplying wheelchairs which, when provided, are no longer appropriate due to functional deterioration. [19] It is important that a person with motor neurone disease has access to a holistic wheelchair and seating assessment as early as possible. This should take into account the progressive nature of motor neurone disease and determine the type of wheelchair that will best suit the changing needs of someone with the condition.
Recent research by Rolfe aimed to identify a timeline for mapping the different types of wheelchair used by people with motor neurone disease from diagnosis to death with review of the Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS) and the site of disease onset as predictors of wheelchair need.[20][21]
Rolfe's Timeline (Fig.4) identifies the average time, in months, that a person with motor neuron disease is likely to need a wheelchair and the type of wheelchair, which in this study included three main types of wheelchair, with some individuals issued with more than one chair at any one time. The three types of wheelchair included;
- Lightweight Manual Chair which can be folded easily e.g. Invacare Action 2000
- Electrically Powered Indoor /Outdoor Chair e.g. Invacare Spectra Plus
- Manual Tilt-In-Space Wheelchair [21]
Average time to provision of a Lightweight Chair was 14 months (range 0-114 months), to an Electrically Powered Indoor /Outdoor Chair was 22 months (range 0-117 months) and to a Manual Tilt-In-Space Chair was 26 months (range 0 - 64). The average time between the provision of a lightweight chair and an EPIOC was 8 months (range 2-17 months); from an EPIOC to a Manual Tilt-In-Space Chair was 7 months (range 3-16); and from a Lightweight to a Manual Tilt-In-Space Chair was 18 months (range 4-30). [21]
The type of onset of disease was also mapped against the timeline of wheelchair provision and the results showed that people with bulbar-onset disease required all types of wheelchair more quickly than those with limb-onset disease, which is consistent with the faster rate of progression of bulbar-onset disease therefore wheelchair services should know the type of onset of motor neuron disease when the client is referred, in order to prioritise their resources further to ensure appropriate and timely provision. [21]
Similarly the ALSFRS Scores, when mapped to the timeline and type of chair provided, assist in predicting when a specific type of chair would be most appropriate. [22]
- The lower the ALSFRS score, the more complex the wheelchair and seating that were required (EPIOC and manual tilt in space).
- The higher ALSFRS score indicated the need for a less supportive chair, such as a lightweight self-propelling standard seat manual chair.
Therefore, knowing the ALSFRS score allows better identification of the type of equipment required.[21]
For wheelchair services to be client-centred, provide appropriate and timely access to services and equipment, be preventative and forward planning they should use the timeline and the ALSFRS score to identify the anticipated wheelchair needs of people with motor neurone disease, which would minimise equipment abandonment and prevent lengthy delays that impact upon individuals’ quality of life.[21]
Orthopaedic Conditions[edit | edit source]
Amputations[edit | edit source]
Amputation is the removal of a limb or part therof, as a result of trauma, prolonged constriction or surgery (see Pathology leading to amputation). As a surgical measure, it is used to control pain or a disease process in the affected limb such as a malignancy, infection or gangrene, while in some cases it is carried out on individuals as a preventative surgery for such problems (see Principles of Amputation). Amputations can be both congenital or acquired. When we look at describing congenital amputation the term limb difference or limb deficiency is used and simply means the partial or total absence of a limb at birth (see Paediatric Limb Deficiency). [23]
Lower extremity amputation continues to be a major source of morbidity and mortality worldwide, although the extent of this burden cannot be accurately quantified because of international variation and a lack of standardized reporting measures. All forms of lower extremity amputation incidence ranges from 46.1 to 9600 per 105 in the population with diabetes, compared to 5.8-31 per 105 in the total population, while major amputation ranges from 5.6 to 600 per 105 in the population with diabetes and from 3.6 to 68.4 per 105 in the total population. This highlight the profound impact of diabetes on amputation rates, mainly resulting from peripheral arterial disease, neuropathy and soft tissue sepsis, which are responsible for the majority of lower extremity amputations, but have show the potential for significant reductions in incidence of lower extremity amputation following introduction of specialist diabetic foot clinics. [24]
The improvement of an individual post amputation is impacted by age, physical and mental health, nutritional status, tissue perfusion, complications post amputation (e.g. poor wound healing or infection), the individual’s motivation, level of amputation, co-morbitities, smoking habits, suitability for prosthesis and the availability of rehabilitation programs, [24][25] with the overall goals of rehabilitation being to optimise the patient’s health status, quality of life and functional independence including personal mobility either through use of a prosthetic and/or wheelchair. [25]
Personal mobility can range from independent, unaided walking through to totally reliant on some form of wheelchair mobility, either manual or powered. Many individuals with amputations will require the use of a wheelchair post-operatively and during the early stages of rehabilitation so functional training to maximise independence in everyday activities needs to be addressed in both a wheelchair and with a prosthesis. It should also be noted that use of a wheelchair as “back up” mobility when a prosthesis is common and in some instances may be preferable to using a prosthesis in some situations due to comfort, function and energy factors e.g. poor fitting prosthesis, or injury/pressure area to residual limb. A wheelchair may increase and enhance function e.g. when a participant may have been using the prosthesis during the day but returns home in the evening and “can’t wait” to get the prosthesis off, they may find accessing the home in the wheelchair is convenient and requires less physical demands compared to using crutches, therefore competent wheelchair skills are essential even for those patients who are prescribed and use a prosthesis daily. [25][26]
Wheelchair use post amputation has a higher incidence in those with bilateral lower limb amputations, with more proximal amputations including hip disarticulation, transfemoral amputation and in those with non-traumatic amputations resulting from peripheral arterial disease, neuropathy and soft tissue sepsis, which tend to occur in aging populations with numerous other comorbidities such as cardiovascular disease, hypertension, renal disease, and arthritis. [24][25] The impact of lower limb amputation on older people with amputations can be complex. Taking into account all possible complications and post-operative goals is paramount for effective management of these patients and depending on their past medical and functional history, the goals and expectations of rehabilitation can be variable. [27] According to Fleury et al, there is a low prosthetic success rate in older people with amputations, with only 36% being successfully fitted with a prosthesis. This may be due to the fact that this population tend to demonstrate more inefficient ambulation, which could be associated with their age, presence of greater comorbidities, and/or higher level of amputation), which contribute to wheelchairs being their mobility device of choice as it requires less energy than walking. While in some cases a prosthesis can aid the ability of the patient to transfer more effectively, the tendency for more fragile skin leading to increased risk for wound break down combined with often decreased range of movement around the hip and knee joint often make the applicability of a prosthesis less suitable. [28]
The Amputee Mobility Predictor (AmpPro / AmpNoPro): is an instrument to assess determinants of the Lower-Limb Amputee's Ability to Ambulate and measure function post-rehabilitation. The test can be performed with or without the prosthesis.The AmpPro form & instructions can be viewed here AmpNoPro (In Appendix 2 for instructions).
Additional Considerations for Children with a Disability[edit | edit source]
When providing a child with a wheelchair, it is important to think about how children’s lives are different from adults’. These differences affect the way the wheelchair service personnel work with children and the choices about wheelchairs and additional postural support. Some important differences are; [29]
- the activities children carry out are different to activities of adults (play, school);
- children are often very active and do not stay in one position for very long;
- children are in the care of adults;
- children cannot always speak for themselves;
- children are still developing;
- young children have a different sitting posture to adults;
- children are still growing.
Wheelchairs that meet children’s needs should support them be a part of the activities that they carry out every day. Features in a wheelchair that are important for children include:[29]
If children push themselves, the wheelchair should:
- fit well to allow them to reach the push rims with comfort;
- be light enough for children to control, particularly going up or down hill.
- Try always to make sure the child is more visible than their wheelchair.
- Extended push handles can help family members or caregivers push the wheelchair without having to bend over.
- A wheelchair that can ride over uneven and soft surfaces such as grass and sand will make it easier for children to play with their friends.
A child’s wheelchair should make it easier for them to access education and enable them to both get to school and be mobile within school environment:[29]
- If most children in the child’s community walk to school, consider whether a wheelchair can travel on these paths?
- Does the child need a wheelchair that is good for rough terrain?
- If the child will go to school in transport (for example car, bus, rickshaw, taxi), think about how the wheelchair will be transported.
- The wheelchair should make it easy for them to be at school. The child should be able to pull up to a desk, or the wheelchair needs a tray as a work surface.
Ideally, children’s wheelchairs should: [29]
- enable children to push themselves, if they are able;
- have push handles to allow peers or adults to assist;
- be able to ride over uneven and soft surfaces such as grass and sand;
- make it easier for children to get to school;
- make it easier for children to be at school.
- attractive enough in terms of design, size and colour;
Importance of an early referral for children
Early referral for children is important, however often parents or referral sources do not refer a child for a wheelchair until the child becomes too heavy to carry. Some of the reasons for this include:
- it is sometimes thought that if a child is given a wheelchair, the child will no longer try to walk;
- while children are young and light, it is easier to carry them than manage a wheelchair over what may be difficult terrain and inaccessible environments;
- parents may not have funds to pay for a wheelchair and will delay until it becomes too difficult to carry the child. It is important to reassure parents and referral sources that a wheelchair will not usually prevent a child from walking. It is more likely that early provision of a wheelchair with good postural support will help the child.
Here are some reasons why early referral is better than delaying:
- Children who have difficulty sitting upright can develop postural problems if not well supported. If a child is referred late some postural problems may have become fixed. This can make it difficult for the child to sit comfortably even with support.
- Without the experience of sitting and being mobile, a child’s development can be delayed.
- For children who have some ability to walk, using a wheelchair may make their daily life easier and allow them to do more things in a day. For these reasons it is better if children come to a wheelchair service earlier.
References[edit | edit source]
- ↑ 1.0 1.1 William Armstrong, Johan Borg, Marc Krizack, Alida Lindsley, Kylie Mines, Jon Pearlman, Kim Reisinger, Sarah Sheldon. Guidelines on the Provision of Manual Wheelchairs in Less Resourced Settings. World Health Organization; Geneva: 2008.
- ↑ Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;49(Feb s109):8–14.
- ↑ SCPE. Dev Med Child Neurol 42 (2000) 816-824
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Rodby-Bousquet E, Hägglund G. Use of Manual and Powered Wheelchair in Children with Cerebral Palsy: A Cross-sectional Study. BMC Pediatrics. 2010 Dec;10(1):59.
- ↑ Rodby-Bousquet E, Hägglund G. Use of Manual and Powered Wheelchair in Children with Cerebral Palsy: A Cross-sectional Study. BMC Pediatrics. 2010 Dec;10(1):59.
- ↑ Rodby-Bousquet E, Hägglund G. Use of Manual and Powered Wheelchair in Children with Cerebral Palsy: A Cross-sectional Study. BMC Pediatrics. 2010 Dec;10(1):59.
- ↑ Rodby-Bousquet E, Hägglund G. Use of Manual and Powered Wheelchair in Children with Cerebral Palsy: A Cross-sectional Study. BMC Pediatrics. 2010 Dec;10(1):59.
- ↑ Lacoste M, Therrien M, Prince F: Stability of Children with Cerebral Palsy in their Wheelchair Seating: Perceptions of Parents and Therapists. Disabil Rehabil Assist Technol. 2009, 4 (3): 143-150. 10.1080/17483100802362036.
- ↑ Tefft D, Guerette P, Furumasu J: Cognitive Predictors of Young Children's Readiness for Powered Mobility. Dev Med Child Neurol. 1999, 41 (10): 665-670. 10.1017/S0012162299001371.
- ↑ Butler C: Effects of Powered Mobility on Self-Initiated Behaviors of Very Young Children with Locomotor Disability. Dev Med Child Neurol. 1986, 28 (3): 325-332. 10.1111/j.1469-8749.1986.tb03881.x.
- ↑ Lundy-Ekman L. Neuroscience: Fundamentals for Rehabilitation. 3rd Edition. St. Louis: Saunders, 2007.
- ↑ 12.0 12.1 Medscape. Spina Bifida. https://emedicine.medscape.com/article/311113-overview#a6 (accessed 9 June 2018).
- ↑ 13.0 13.1 Oakeshott P, Hunt GM, Poulton A, Reid F. Open Spina Bifida: Birth Findings Predict Long-term Outcome. Archives of Disease in Childhood. 2011 Nov 1:archdischild-2011.
- ↑ Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C. Functional Ambulation in Patients with Myelomeningocele. JBJS. 1973 Jan 1;55(1):137-48.
- ↑ Wyszynski DF, editor. Neural Tube Defects: From Origin to Treatment. Oxford University Press; 2005 Oct 13.
- ↑ 16.0 16.1 Frederick M Maynard et al., International Standards for Neurological and Functional Classification of Spinal Cord Injury, American Spinal Injury Association, 1996
- ↑ 17.0 17.1 17.2 Medscape. Multiple Sclerosis. https://emedicine.medscape.com/article/1146199-overview (accessed 02 June 2018)
- ↑ Brown TR, Sliwa J. Wheelchair Prescription for People With MS: Ask the Right Questions, Get the Right Answers. International Journal of MS Care. 2005;7(3):115-6.
- ↑ 19.0 19.1 Talbot K, Marsden R (2008) Motor neuron disease: the facts. Oxford: Oxford University Press.
- ↑ 20.0 20.1 Talbot K, Turner M, Marsden R, Botell R (2009) Motor neuron disease: a practical manual. Oxford Care Manuals. Oxford: Oxford University Press.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 Rolfe J. Planning wheelchair service provision in motor neurone disease: implications for service delivery and commissioning. British Journal of Occupational Therapy. 2012 May;75(5):217-22.
- ↑ Cedarbaum J, Stambler N (1997) Performance of the Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS) in multicentre clinical trials.Journal of the Neurological Sciences, 152(Supplement 1), s1-s9.
- ↑ Limb Loss Definitions. Fact Sheet. Amputee Coalition 2008. http://www.amputee-coalition.org/resources/limb-loss-definitions/ [accessed 24 Sep 2017]
- ↑ 24.0 24.1 24.2 Moxey PW, Gogalniceanu P, Hinchliffe RJ, Loftus IM, Jones KJ, Thompson MM, Holt PJ. Lower extremity amputations—a review of global variability in incidence. Diabetic Medicine. 2011 Oct;28(10):1144-53.
- ↑ 25.0 25.1 25.2 25.3 VA/DoD, 2008, VA/DoD Clinical Guidelines for Rehabilitation of Lower Limb Amputation, Online accessed 1st June 2018 https://www.healthquality.va.gov/guidelines/Rehab/amp/VADoDLLACPG092817.pdf
- ↑ College of Occupational Therapists, 2011, ‘Occupational therapy with people who have had lower limb amputations evidence based guidelines’, College of Occupational Therapists, Brunel, London
- ↑ Fried L, Ferrucci L, Darer J, Williamson J, & Anderson G (2004), 'Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care', Journal of Gerontology, Vol.59, No. 3, pp.255-263.
- ↑ Fleury A, Salih A, & Peel N (2013), 'Rehabilitation of the older vascular amputee: A review of the literature', Geriatric and Gerontology International, vol.13, pp. 264-273.
- ↑ 29.0 29.1 29.2 29.3 Sarah Frost, Kylie Mines, Jamie Noon, Elsje Scheffler, and Rebecca Jackson Stoeckle. Wheelchair Service Training Package - Reference Manual for Participants - Intermediate Level. Section A.2 Children with Disabilities. World Health Organization, Geneva. 2013






