Bowel Management in Spinal Cord Injury
Original Editor - Naomi O'Reilly
Top Contributors - Redisha Jakibanjar, Naomi O'Reilly, Kim Jackson, Anas Mohamed, Arnold Fredrick D'Souza, Admin and Lucinda hampton
Introduction[edit | edit source]
Neurogenic bowel dysfunction is characterized by alteration in normal bowel function due to the lack of nervous control.[1][2] The clinical symptoms of neurogenic bowel may vary. Some clinical symptoms are bloating, constipation, abdominal pain, Urinary Incontinence.[2]
The symptoms of neurogenic bowel in Spinal Cord Injury can be broadly divided into two headings:
Upper Motor Neuron (UMN) Bowel Syndrome[edit | edit source]
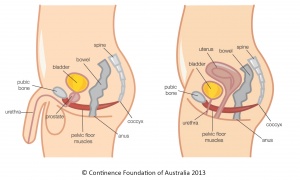
Upper Motor Neuron (UMN) Bowel Syndrome occurs in a spinal cord injury above the conus medullaris and results in a hyperreflexic bowel, characterized by an increased colonic wall and anal tones, with disrupted voluntary External Anal Sphincter (EAS) control. The nerve connections between the spinal cord and colon remain intact so, the sphincter remains tight thereby promoting retention of stool and there is preserved reflex coordination and stool propulsion. Hence, UMN Bowel Syndrome is associated with constipation and fecal retention at least in part due to EAS activity.[3]
Lower Motor Neuron (LMN) Bowel Syndrome[edit | edit source]
Lower Motor Neuron (LMN) Bowel Syndrome, occurs in a spinal cord injury at the conus medullaris or cauda equina and results in an areflexic bowel, characterized by loss of spinal cord-mediated peristalsis and slow stool propulsion with an atonic EAS. Typically, it is associated with constipation and a significant risk of incontinence due to flaccid paralysis of the EAS and reduced motor control of levator ani.[3]
The three main implications of disruption to the motor, sensory, and autonomic pathways post spinal cord injury on bowel function are an inability to:
- Feel when the bowel is full
- Voluntarily control muscles to defecate
- Voluntarily contract muscles to prevent defecating.
Neurogenic bowel dysfunction can have different neuropathological patterns in individuals with Spinal Cord Injury including:
Pattern A: This pattern is seen in individuals with a Spinal Cord Injury above T7 and is characterised by loss of voluntary abdominal muscle contraction but preserved sacral spinal reflexes. Individuals with this pattern have a moderate delay in Colonic Transit Time (CTT), absence of anal relaxation during the defecatory manoeuvre, and decreased intra-abdominal pressure, which causes very frequent constipation with significant defecatory difficulty and infrequent incontinence. [4]
Pattern B: This pattern is seen in individuals with a Spinal Cord Injury below T7 and who have preserved both voluntary control of abdominal muscles and preserved sacral reflexes. These individuals have a moderate delay in CTT, have increased intra-abdominal pressure and increased anal resistance during the defecatory manoeuvre, presence of external anal sphincter contraction when intra-abdominal pressure increases, and during rectal distension. They have frequent constipation, significant defecatory difficulty, and not very frequent incontinence. [4]
Pattern C: This pattern is seen in individuals with a Spinal Cord Injury below T7 and who have voluntary control of abdominal muscles and absent sacral reflexes. They have frequent constipation, less difficulty during defecation, and have a high chance of incontinence due to severe delay in CTT, increased intra-abdominal pressure, absence of anal resistance during the defecatory manoeuvre, and absence of EAS contraction when intra-abdominal pressure increases and during renal distension.[4]
Consequences of Neurogenic Bowel Dysfunction[edit | edit source]
People with Neurogenic Bowel Dysfunction commonly have the following consequences in life.[2][5]
- Loss of Independence
- Feeling of Embarrassment
- Social Isolation (Restrictions in social life)
- Decreased Quality of Life
Assessment[edit | edit source]
Bowel management will be successful only when the assessment is properly completed, diagnosis is accurate and the treatment is individualised. The history-taking should include;[1]
- Previous Bowel and Bladder habits and the findings should be related to current situations
- Premorbid bowel history, which includes;
- Daily Fluid Intake
- Diet (Fiber, Meal Frequency, Spice preferences, Amounts)
- Bowel Movements (Frequency, Duration, Difficulties)
- Stool (Consistency, Colour, Mucus, Blood)
- Medications
- Current Situation
- Spinal Cord Injury ASIA Level
- Daily Fluid Intake
- Medication
- Diet (Fiber, Meal Frequency, Spice preferences, Amounts)
- Bowel Movements (Frequency, Duration, Difficulties)
- Stool (Consistency, Colour, Mucus, Blood)
- Bowel Care Habits (Frequency, Duration, Digital Stimulation, Frequency / Technique)
- Bowel Incontinence History (Time of day, Frequency, Relationship to eating)
- Understanding of the effect of spinal cord injury on elimination, of the patients
- Before setting the intervention goals, the examiner should have knowledge about the lifestyle of the individual including
- Daily Schedule, For example, School, Work, Leisure Activities
- Assistance Level (Assistance Required, Assistance Availability)
- Amount of Time needed to complete a Bowel Care Regimen
Proper examination of the body and organs also gives a brief idea for diagnosis. The bowel sounds should be auscultated and the abdomen should be properly palpated and check for distention.[1]
Rectal examination should also be performed as it gives the idea about sphincter innervation and the amount and consistency of stool present in the rectal vault, the presence of hemorrhoids or masses, and in males the size of the prostate gland. Rectal examination should also determine the rectal angle and tone or spasticity of the puborectalis muscle. When the examining finger is inserted, it should be directed towards the umbilicus to check the rectal angle, and to check for puborectalis tone, gentle pressure is applied towards the sacrum. The strength and endurance of the voluntary muscles (EAS, Puborectalis, and Bulbocavernosus) should also be assessed. These findings will also help to differentiate whether the injury is UMN or LMN type.[1]
The neurological examination should also include sacral reflexes, including anal tone, anocutaneous reflex (a contraction of the EAS in response to pricking or stroking the anal skin and it should be assessed in all four quadrants that surround the anal verge), bulbocavernosus reflex (pricking or pinching the dorsal glans penis or pressing the clitoris and palpating for bulbocavernosus and EAS contraction), and the internal anal sphincter reflexes (a contraction of the IAS with the stimulation of digital introduction to the rectum beyond the EAS and the sphincter is closed immediately on withdrawal).[1]
Other examination methods include lab tests, radiographic findings, and liver function tests.[1]
Management[edit | edit source]
There are various management options available according to the condition of the patient. It can be pharmacological and Non-pharmacological (including surgery and conservative management).
Non-Pharmacological[edit | edit source]
This method of management includes multifaceted programs, use of suppositories, dietary fiber, reflex stimulation of the GI tract, abdominal massage, assistive devices, irrigation techniques, functional electrical and magnetic stimulation of skeletal muscles.
Multifaceted Programs[edit | edit source]
This technique includes targeting more than one factor for the goal of reducing the CTT and decreasing the incidence of difficult evacuations. There are various factors responsible for effective bowel management like diet modification, routine bowel evacuation, and anal stimulation.[5] [3]
Use of Suppositories and Oral Laxatives[edit | edit source]
The use of suppositories and oral laxatives is also another method commonly used. Bisacodyl and glycerin are used commonly as active ingredients in the suppositories. The oral laxatives include peristaltic stimulants, osmotic laxatives, bulk-forming agents, and stool softeners.[5][3]
Dietary Fibre[edit | edit source]
Consuming a fiber-rich diet has also shown benefit to some patients. But the result may vary from person to person so, care should be taken and only a fiber-rich diet might not be helpful all the time.[3]
Reflex Stimulation of the GI Tract[edit | edit source]
Digital rectal stimulation is presumed to increase the motility in the left colon by activating preserved anorectal colonic reflexes. Enemas can also be a vital technique for the facilitation of bowel evacuation. [3][5]
Abdominal Massage[edit | edit source]
15 minutes of abdominal massage done for 15 days from cecum-colon-rectum has shown effective results for shortening the colonic transit time, decrease abdominal distension, and increased the frequency of bowel movements per week.[3]
Assistive Devices[edit | edit source]
Various assistive devices can be used for effective bowel evacuation for instance modified toilet seat, standing table, washing toilet seat with a visual feedback system.[3]
Irrigation Techniques[edit | edit source]
Transanal irrigation means inserting a balloon catheter into the rectum and slowly administering warm tap water in the specified volume. This technique has shown to improve constipation, fecal incontinence, and improve QoL. Enema continence catheter can also be used as an effective method for bowel evacuation.[5][3]
Electric Stimulation Techniques[edit | edit source]
Electric stimulators are based on a mechanism to promote the normal function of the intestine through improving blood flow, promoting protein synthesis, reinforcing muscular strength, and regulating nerve stimulation. There are various kinds of electric stimulators used. Some are:
- Transcutaneous electrical stimulation- safe, noninvasive, painless and could stimulate sympathetic and parasympathetic nerve fibers in the bowel system and reduces the pressure of the internal and external sphincter in the anus. [3][2]
- Transrectal bowel stimulation- improves the ability to control the intestinal tract, enhances the sense of the need to defecate, and reduces intestinal peristalsis hence it reduces the rate of fecal incontinence [2]
- Intravesical electrical stimulation- it decreases intravesical pressure and increases urinary bladder capacity and can also facilitate bladder emptying [2]
- Sacral nerve stimulation- a relatively safe and effective method despite the minimally invasive procedure (Level-4 Evidence)[2][3]
- Dorsal genital nerve electrical stimulation [2]
- Percutaneous tibial nerve stimulation [2][3]
- Threshold night-time electrical stimulation [2]
Colostomy[edit | edit source]
A colostomy is a surgical process of connecting the colon to an opening in the abdominal wall making an artificial anus. This process is done to patients who have faced failure in all the medical treatments available for bowel management. It has shown to reduces the number of hospitalizations caused by gastrointestinal problems and improves physical health, psychosocial adjustment, and self-efficacy areas within the quality of life.[3]
The Malone Antegrade Continence Enema and the Enema Continence Catheter[edit | edit source]
This approach is creating an entry into the large intestine surgically to irrigate the intestine. The procedure connects the appendix to the abdominal wall and acts as a valve mechanism that allows catheterization of the appendix, but avoids leakage of stool through it, thus forming an appendicostomy. Hence, a catheter can be introduced to the patient through the stoma and an enema can be administered. This process creates a washout effect and stimulates colonic peristaltic, the colon and rectum will empty, thus preventing fecal incontinence and constipation.[3]
Pharmacological Agents[edit | edit source]
Pharmacological drugs that can be used are:[3]
- Cisapride (Level 1 and 2 Evidence)
- Prucalopride (Level 1 Evidence)
- Intravenous administration of Metoclopramide (Level 2 Evidence)
- Neostigmine (a reversible cholinesterase inhibitor) or the combination of Neostigmine and Glycopyrrolate (Level 1 Evidence)
- Fampridine (selective potassium channel blocker) (Level 1 Evidence)
The table below shows the considerations and some management options.
| Bowel Management Options | Considerations for Appropriate Bowel Management Options |
|---|---|
| High Fibre Diet | Presence or Absence of Bowel Reflexes
Hand Function Patients’ Preference Other Complex Factors |
| Adequate Fluid Intake | |
| Regular Bowel Emptying Routine | |
| Digital Stimulation Bowel Reflexes | |
Medication
|
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Stiens SA, Bergman SB, Goetz LL. Neurogenic bowel dysfunction after spinal cord injury: clinical evaluation and rehabilitative management. Archives of physical medicine and rehabilitation. 1997 Mar 1;78(3):S86-102.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Deng Y, Dong Y, Liu Y, Zhang Q, Guan X, Chen X, Li M, Xu L, Yang C. A systematic review of clinical studies on electrical stimulation therapy for patients with neurogenic bowel dysfunction after spinal cord injury. Medicine. 2018 Oct;97(41).
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 Krassioukov A, Eng JJ, Claxton G, Sakakibara BM, Shum S. Neurogenic bowel management after spinal cord injury: a systematic review of the evidence. Spinal cord. 2010 Oct;48(10):718-33.
- ↑ 4.0 4.1 4.2 Vallès M, Mearin F. Pathophysiology of bowel dysfunction in patients with motor incomplete spinal cord injury: comparison with patients with motor complete spinal cord injury. Diseases of the colon & rectum. 2009 Sep 1;52(9):1589-97.
- ↑ 5.0 5.1 5.2 5.3 5.4 Hughes M. Bowel management in spinal cord injury patients. Clinics in colon and rectal surgery. 2014 Sep;27(03):113-5.
- ↑ SCIUcourses. Bowel 1.3 - Neurogenic Bowel. Available from: https://youtu.be/AYQo1R-sFHk[last accessed 30/10/18]
- ↑ SCIUcourses. Bowel 2.1 - The Perfect Program. Available from: https://youtu.be/2K7DByoxias[last accessed 30/10/18]